Liver retransplantation (LRT) is a controversial indication. Our aim was to evaluate the rate of LRT at our institution, and to analyze its indications and short- and long-term results.
MethodsWe conducted a retrospective study of a prospectively collected database, including 1645 LT from 1984 to 2018. Results have been analyzed depending on type of LRT (early vs. late), study period and indications.
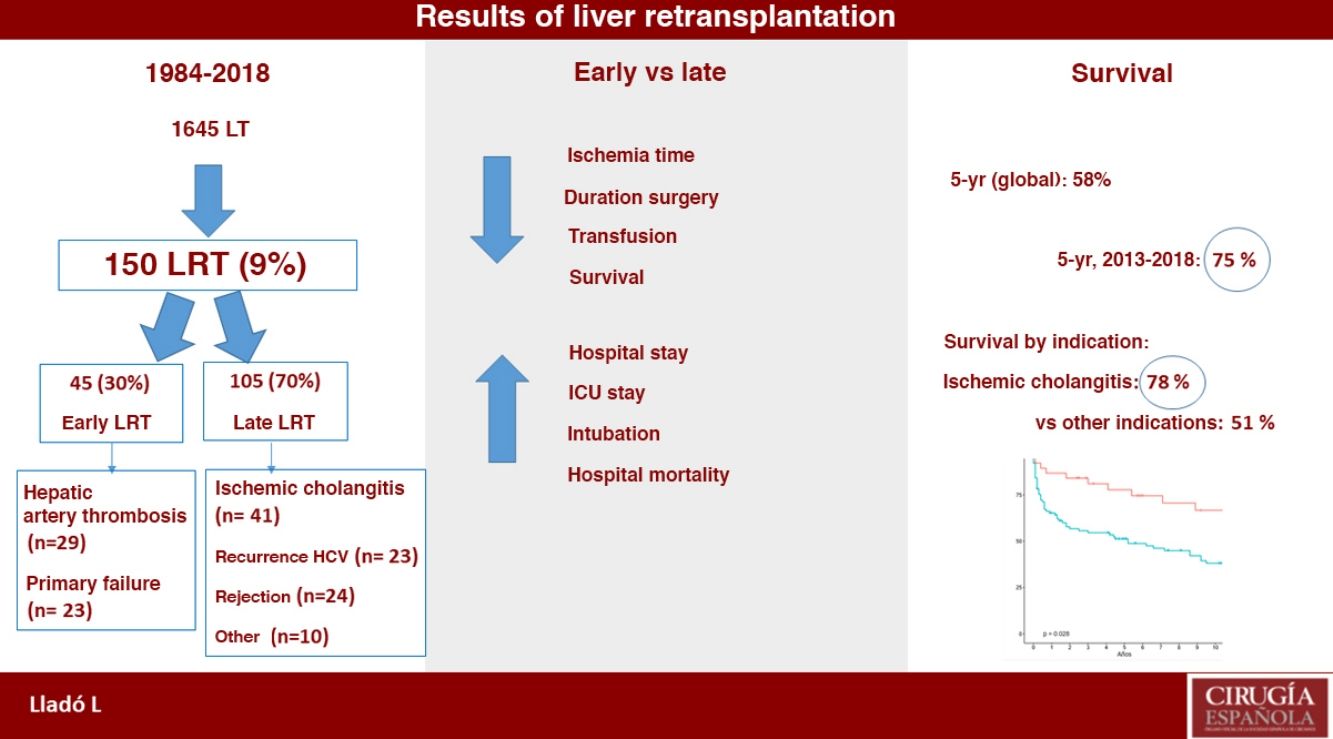
ResultsWe performed 150 LRT in 140 patients. The LRT rate was 9%. Of these, 45 LRT were early (30%), and the other 70% were late LRT. The main indications were: ischemic cholangitis (27%), arterial thrombosis (19%), primary non-function (15%), and HCV recurrence (15%). Mean surgery duration (395 vs. 270 min; P = .001), cold ischemia time (435 vs. 390 min; P = .005) and transfused units required (8 vs. 5 RBC; P = .034) were higher in cases of late LRT. Postoperative mortality (10 vs. 20%; P = .01) was better in cases of late LRT. One- and 5-year actuarial survival rates were 71% and 58%, respectively, which were significantly better during the last decade (80% and 64%). Five-year actuarial survival for ischemic cholangitis is better than other indications, such as recurrence of HCV (78 vs. 51%; P = .02).
ConclusionsLiver retransplantation is complex and associated with high morbidity and mortality. However, indications and long-term results have improved during recent years. Therefore, LRT is justified.
El retrasplante hepático (ReTH) es una indicación de TH controvertida. Nuestro objetivo fue determinar la tasa de ReTH y las indicaciones, morbilidad, mortalidad posoperatoria y supervivencia actuarial del paciente retrasplantado en nuestra serie.
MétodosEstudio retrospectivo de una serie prospectiva de 1.645 pacientes trasplantados entre 1984 y 2018. Se analizan los resultados según el tipo de ReTH (precoz vs. tardío), periodo de estudio e indicaciones.
ResultadosHemos realizado 150 ReTH en 140 pacientes. La tasa de ReTH fue de 9%. El 30% (45) de los ReTH fueron precoces, siendo tardíos el otro 70% (105). Las causas más frecuentes fueron: colangitis isquémica (27%), trombosis de la arteria hepática (19%), fallo primario del injerto (15%) y recidiva de la cirrosis por virus de la hepatitis C (VHC) (15%). La duración de la cirugía (395 vs. 270 min; p = 0,001), tiempo de isquemia (435 vs. 390 min; p = 0,005) y necesidad transfusional (8 vs. 5 CH; p = 0,034) fue mayor en los casos de ReTH tardío, mientras que la mortalidad posoperatoria (10 vs. 20%; p = 0,01) fue mejor en los casos de ReTH tardío. La supervivencia actuarial a uno y cinco años fue de 71% y 58%, respectivamente, con una mejoría significativa en la última década (80% y 64%). Por otra parte, la supervivencia en los casos de ReTH por colangitis isquémica es superior que otras indicaciones (78 vs. 51%; p = 0,02).
ConclusionesEl retrasplante es complejo y está asociado a una elevada morbimortalidad. Sin embargo, los resultados han mejorado en los últimos años por lo que su indicación está justificada.
Liver retransplantation (LRT) is the only therapeutic option in cases of graft failure. Currently, more than 1000 liver transplantations (LT) are carried out in Spain annually, and 5-year and 15-year survival rates are more than 70% and 50%, respectively.1 Some 15%–23% will present early or late-onset complications that will cause irreversible graft dysfunction and, therefore, the need for a new LT.
Although the results of LRT have improved in recent years, most series show that postoperative morbidity and mortality, as well as survival, quality of life and cost are significantly worse than after an initial LT.2–5 All this has led many hospitals to consider whether LRT is truly indicated.6,7
In addition, in the current context of reducing waiting lists thanks to the efficacy of antiviral treatments against the hepatitis C virus (HCV), Spanish LT groups are considering expanding the indications for LT.8 At the same time, the availability of donors has expanded thanks to the expansion of non-heart beating donation protocols. In the case of LRT, as in any extension of the indication, a minimum 5-year survival of 50% should be obtained, which has been established in the consensus document for the expansion of criteria of the Spanish Society of Liver Transplantation (Sociedad Española de Trasplante Hepático, or SETH).8 In this new scenario, we consider it important to know the current results of LRT in our setting in order to be able to respond objectively regarding its justification.
The objectives of this study were to evaluate the results of LRT in our series, considering the types of LRT, as well as the period and indication.
MethodsWe conducted a retrospective study of a series collected prospectively in the database of our LT unit. All transplant patients between 1984 and 2018 were evaluated. No patient was excluded.
For the analysis of the results, we established five periods, including a similar number of LT: from 1984 to 1994, 28 LRT were performed; from 1995 to 1999, 37 LRT; from 2000 to 2006, 40 LRT; from 2007 to 2012, 20 LRT; and from 2013 to 2018, 25 LRT.
Likewise, the results were analyzed according to the type of LRT: ‘early’ occurred during the first week after LT; and ‘late’ were performed after the first week post-LT.
Finally, the survival results were analyzed according to the different indications for LRT. The study did not include patients for whom LRT was ruled out, either due to disease severity or other contraindications. Starting in 2012, the Rosen score (>20.5) was established as a selection criterion to contraindicate LRT.
Statistical analysisQuantitative variables are expressed as median and 25%–75% percentiles, and qualitative variables as number and percentage. Differences between groups were assessed using parametric or non-parametric tests, as needed. The qualitative variables were analyzed with the Chi-squared or Fisher’s tests, while the quantitative variables with the Student’s t test, and in the case of non-normal distribution, the Mann–Whitney U test. Actuarial survival was analyzed according to the Kaplan–Meier method and comparisons between curves with the log-rank test. Statistical significance was established at P < .05. The statistical analysis was performed using the R 3.6 program (R Foundation for Statistical Computing, Vienna, Austria).
ResultsDuring the study period, 1645 patients received transplants, 150 (9%) of which were LRT. Eight of these LRT were a second LRT, and one patient received a third LRT. Therefore, the overall incidence of LRT was 9% of the series; by periods studied, the percentages were 11%, 12%, 9% and 7.7%, respectively (Table 1).
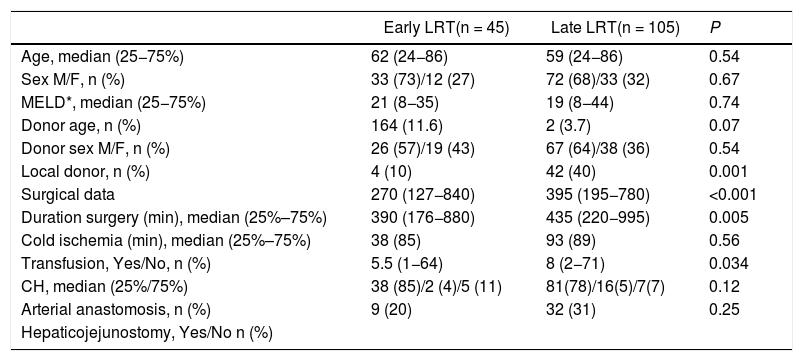
Preoperative and operative characteristics depending on the type of retransplantation.
| Early LRT(n = 45) | Late LRT(n = 105) | P | |
|---|---|---|---|
| Age, median (25−75%) | 62 (24−86) | 59 (24−86) | 0.54 |
| Sex M/F, n (%) | 33 (73)/12 (27) | 72 (68)/33 (32) | 0.67 |
| MELD*, median (25−75%) | 21 (8−35) | 19 (8−44) | 0.74 |
| Donor age, n (%) | 164 (11.6) | 2 (3.7) | 0.07 |
| Donor sex M/F, n (%) | 26 (57)/19 (43) | 67 (64)/38 (36) | 0.54 |
| Local donor, n (%) | 4 (10) | 42 (40) | 0.001 |
| Surgical data | 270 (127−840) | 395 (195−780) | <0.001 |
| Duration surgery (min), median (25%–75%) | 390 (176−880) | 435 (220−995) | 0.005 |
| Cold ischemia (min), median (25%–75%) | 38 (85) | 93 (89) | 0.56 |
| Transfusion, Yes/No, n (%) | 5.5 (1−64) | 8 (2−71) | 0.034 |
| CH, median (25%/75%) | 38 (85)/2 (4)/5 (11) | 81(78)/16(5)/7(7) | 0.12 |
| Arterial anastomosis, n (%) | 9 (20) | 32 (31) | 0.25 |
| Hepaticojejunostomy, Yes/No n (%) |
M/F: male/female.
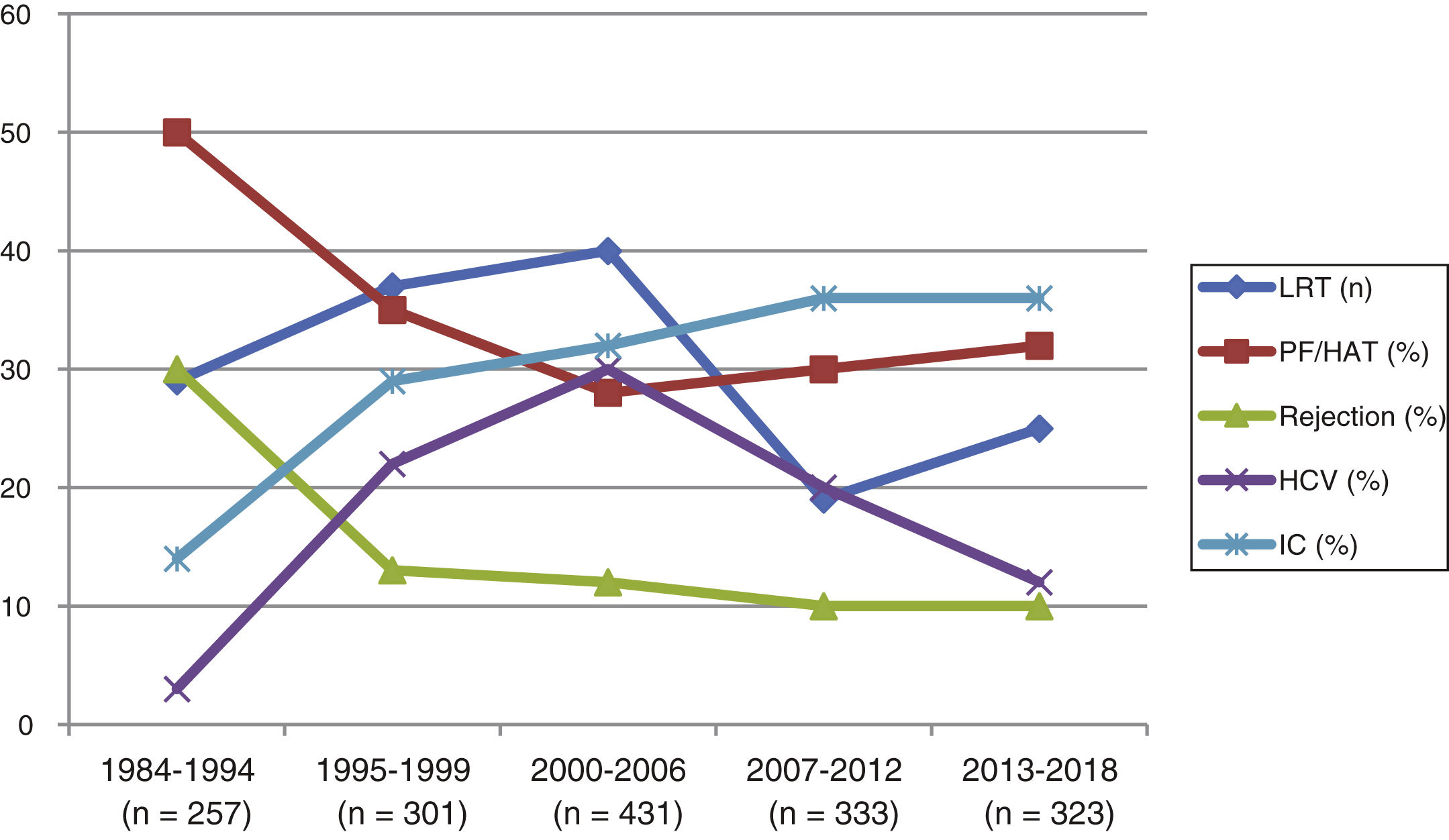
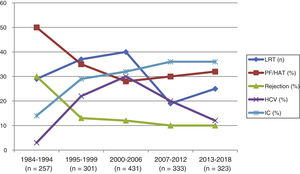
Out of the 150 LRT (in 140 patients), 45 (30%) were early retransplants, while 105 (70%) were late. The indications according to the different study periods are reflected in Fig. 1. HCV recurrence decreased as a cause of indication for LRT from 20%–22% in the initial periods to 12% in the 2013–2018 period.
Evolution of the incidence of retransplantation and indications throughout the study periods. LRT: number of retransplants; PF/HAT: LRT due to primary failure of hepatic arterial thrombosis; Rejection: LRT for rejection; HCV: LRT for recurrence of hepatitis C virus; IC: LRT for ischemic cholangitis.
The comparative analysis of preLT and surgical data between early and late LRT is shown in Table 2. The duration of surgery, ischemia time, and the need for packed red blood cells were significantly higher in the cases of late LRT. In addition, for biliary reconstruction, hepatic-jejunostomy was required more often in cases of late LRT. In both the early and late LRT cases, the type of arterial anastomosis was ‘non-standard’ in 20% and 18% of the cases, respectively.
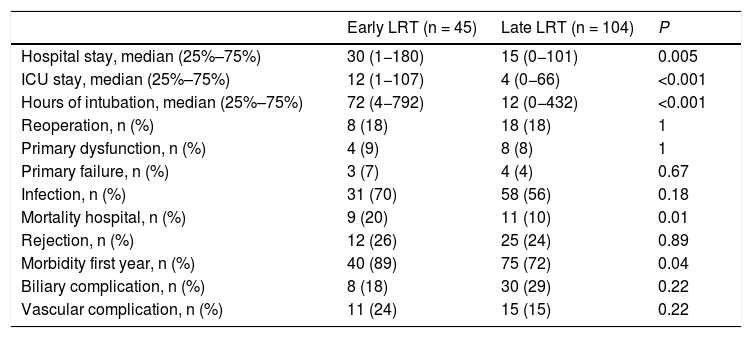
Postoperative evolution depending on the type of retransplantation.
| Early LRT (n = 45) | Late LRT (n = 104) | P | |
|---|---|---|---|
| Hospital stay, median (25%–75%) | 30 (1−180) | 15 (0−101) | 0.005 |
| ICU stay, median (25%–75%) | 12 (1−107) | 4 (0−66) | <0.001 |
| Hours of intubation, median (25%–75%) | 72 (4−792) | 12 (0−432) | <0.001 |
| Reoperation, n (%) | 8 (18) | 18 (18) | 1 |
| Primary dysfunction, n (%) | 4 (9) | 8 (8) | 1 |
| Primary failure, n (%) | 3 (7) | 4 (4) | 0.67 |
| Infection, n (%) | 31 (70) | 58 (56) | 0.18 |
| Mortality hospital, n (%) | 9 (20) | 11 (10) | 0.01 |
| Rejection, n (%) | 12 (26) | 25 (24) | 0.89 |
| Morbidity first year, n (%) | 40 (89) | 75 (72) | 0.04 |
| Biliary complication, n (%) | 8 (18) | 30 (29) | 0.22 |
| Vascular complication, n (%) | 11 (24) | 15 (15) | 0.22 |
Patients with early LRT had a significantly greater ICU stay, hospital stay, intubation requirement and hospital mortality than the late LRT cases. There were no differences in morbidity (infection, reoperation, or technical complications) between the two groups (Table 2).
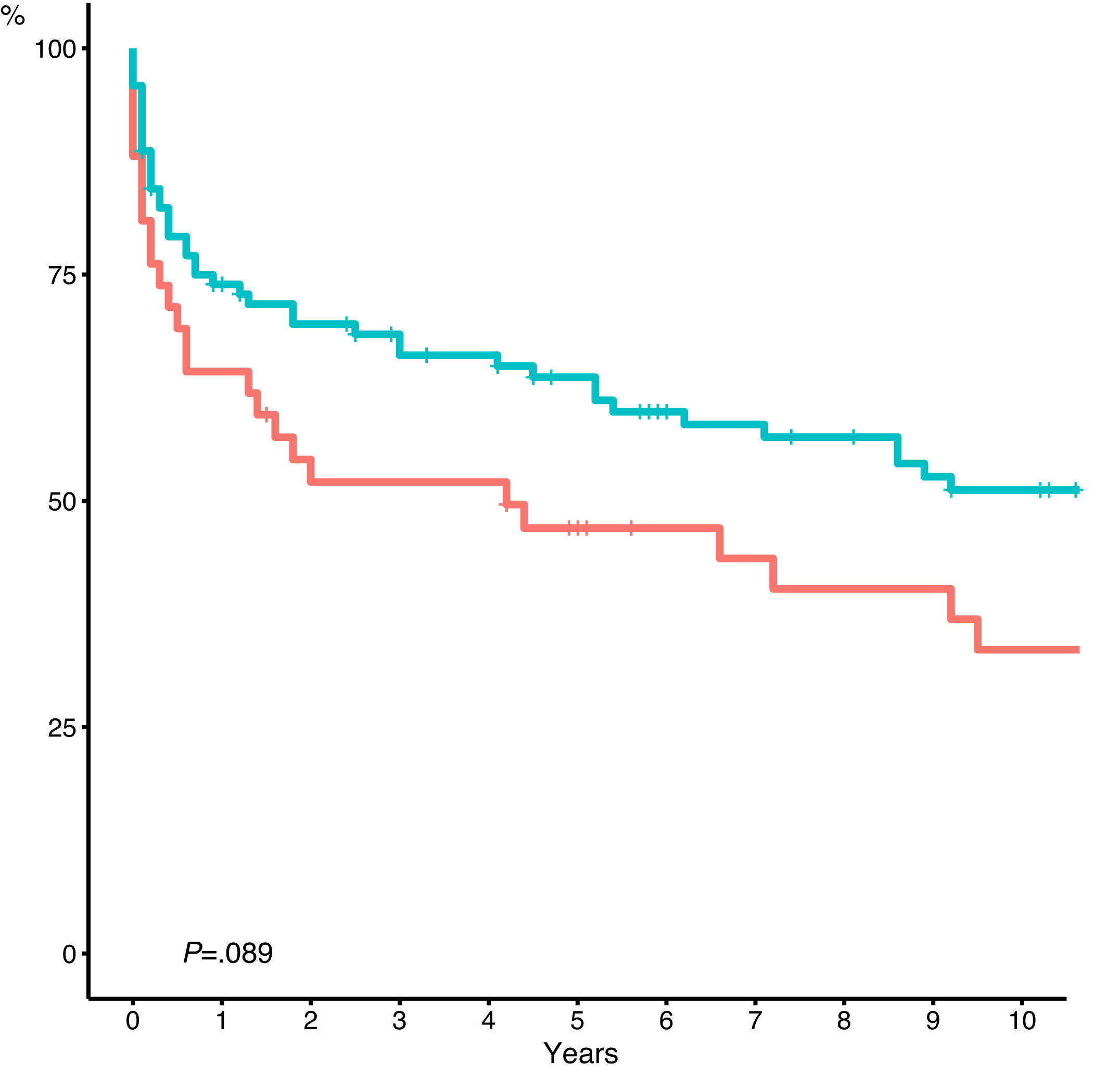
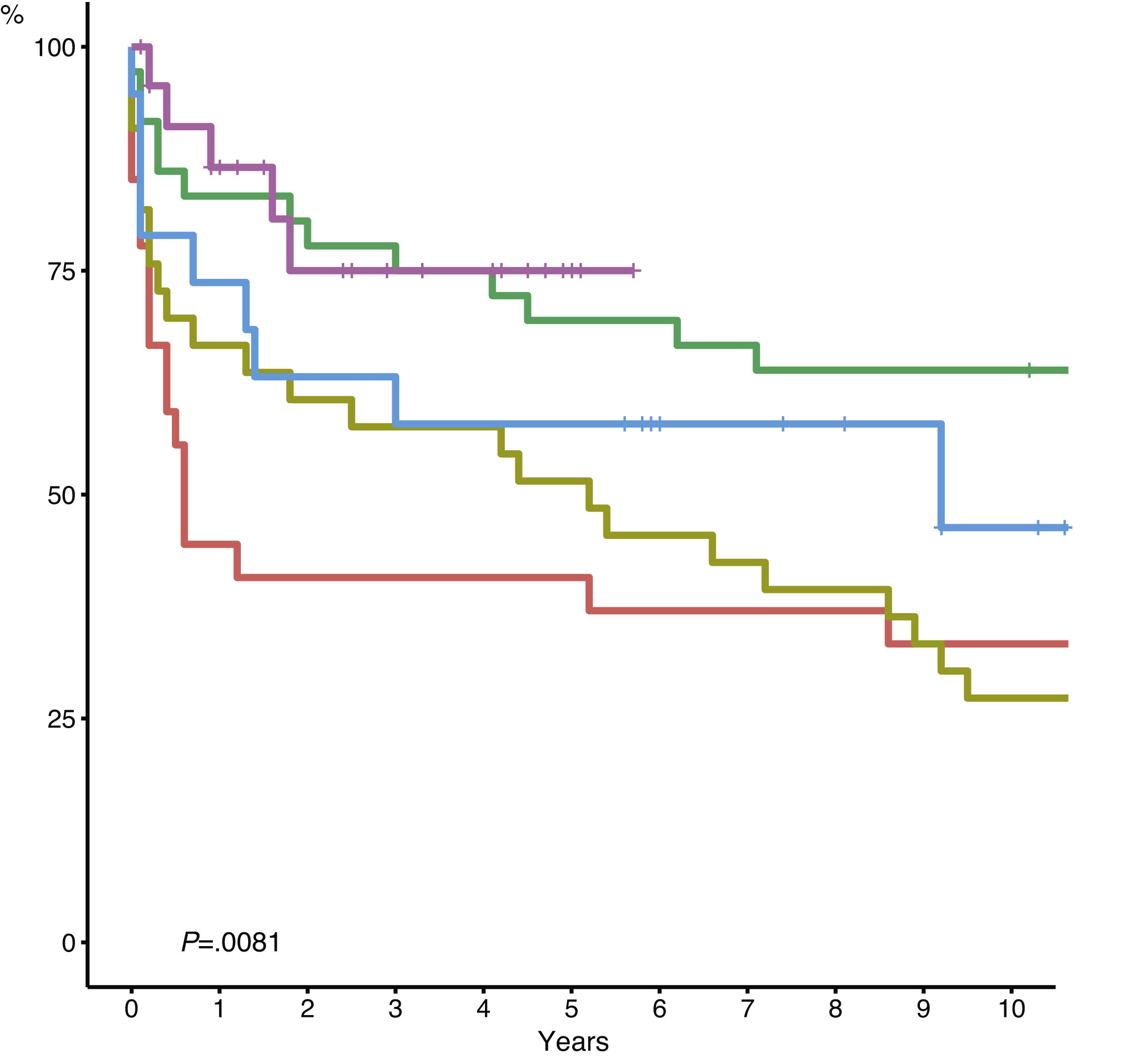
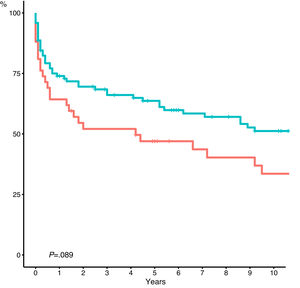
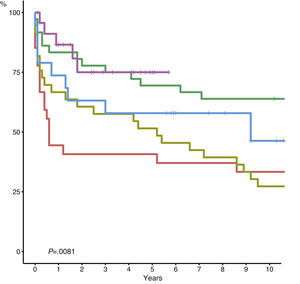
Although we did not observe statistically significant differences, the five-year actuarial survival of late LRT shows a tendency to be better than early LRT (early: 46 vs. late: 63%; P = .08) (Fig. 2). The five-year actuarial survival rates were significantly better in the groups of retransplanted patients in the last two periods (2007–2012 and 2013–2018) (P = .0081) (Fig. 3).
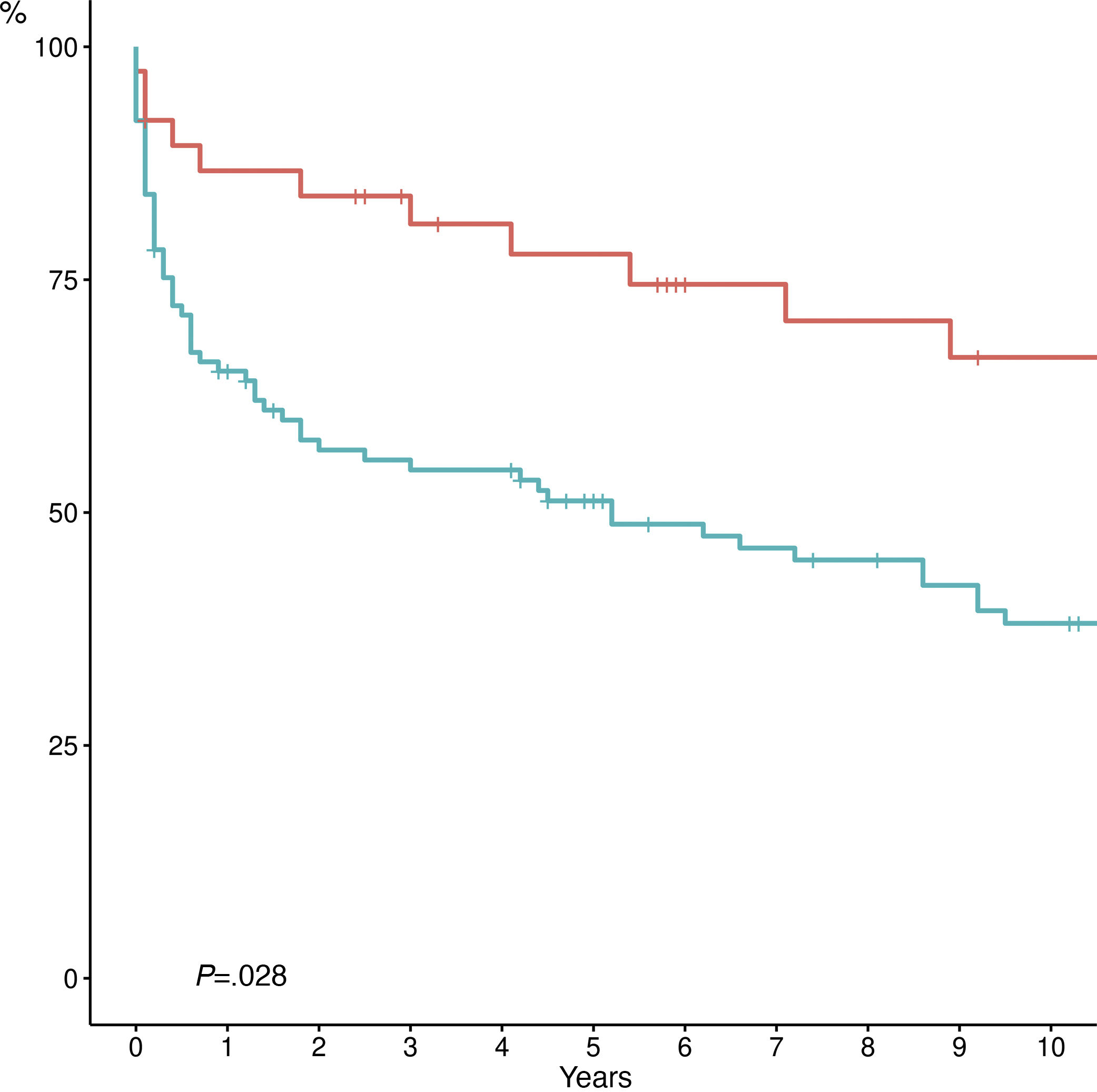
Although the actuarial survival comparison study between the different indications did not show statistically significant differences, the five-year actuarial survival of retransplanted patients due to ischemic cholangitis was significantly better than the remaining indications (ischemic cholangitis: 77 vs. others: 51.3%; P = .02) (Fig. 4).
DiscussionAccording to published series,1–3,9 LRT represent 3%–24% of indications for LT, a range which reflects the different patient selection criteria for LRT among hospitals. If we focus on the most recent data from the 2017 Spanish LT Registry,1 1203 LT were performed in Spain, 3.2% of which were early LRT and 5% late LRT. Data from the European Liver Transplant Registry (ELTR) also show an incidence of LRT that was 5% from 1999 to 2009.10 Similarly, data from the United Network for Organ Sharing (UNOS) show a global LRT incidence of 15%, which dropped to 7.9% in 200511 and to 4.3% in 2017.12 In our series, the indication of LRT was 9%: 2.7% urgent and 6.3% late. This incidence was 7.7% in the last period, which is a decrease similar to published series. These data comply with the quality data established by the SETH,13 which establishes that the incidence of acute LRT in hospitals should be less than 5%, and the incidence of late LRT less than 8%.
The causes of LRT have evolved along with the evolution of transplantation. The evolution in the criteria for donor selection, recipient selection, immunosuppression, new antiviral treatments, etc., have all led to changes in the causes of LRT.
The most frequent causes of early LRT are primary graft failure and early arterial thrombosis. The frequencies in our series are comparable to the data from other registries.1,12 The frequency and cause of urgent LRT has changed little over the years. Although the surgical technique, anesthetic management and preservation solutions have improved, at the same time we have expanded the use of marginal donors. Possibly for this reason, the incidence of primary failure and hepatic artery thrombosis remain stable.
The main causes of late LRT are biliary complications, chronic rejection, and recurrence of the baseline disease (especially HCV recurrence). In our experience, the main cause of late LRT was ischemic cholangitis. We have observed a decrease in the indication for HCV recurrence, especially in the last period. With the evolution of immunosuppression, graft rejection as a cause of LRT has been decreasing, as has HCV recurrence, thanks to new antiviral treatments.14 The increase in ischemic cholangitis as the main indication for LRT does not imply an increase in the incidence of ischemic cholangitis in our series, but rather an increase in the percentage compared to other indications for LRT. Furthermore, it should be noted that only one of the retransplanted patients due to ischemic cholangitis had received a graft from a non-heart beating donor (and this donation was made prior to the use of normothermia at our hospital).
LRT results are classically considered worse than those of an initial LT. However, as reflected in our data, early and late LRT are two clearly different patient groups. Patients requiring late LRT often require special technical resources that prolong surgery, ischemia times, and increase the risk of septic, hemorrhagic, and vascular complications. Likewise, this group of patients requires a higher consumption of blood products, a consequence of the greater technical complexity, adhesions and neovascularization that develops in some patients with late dysfunction after LT.15
Early or acute LRT is generally the same or even simpler than the initial LT.16 Given that it is indicated during the first week after LT, there is not yet a significant adhesion problem. Much less dissection is required, and the degree of portal hypertension is lower than in the first LT.16 Thus, in our experience, intraoperative data were significantly better in the early LRT group. However, this group of patients is retransplanted in an emergency situation, and their serious condition is reflected in the higher postoperative morbidity and mortality.
In previous series, in-hospital mortality in LRT is three to five times higher than after an initial LT,2,5,14 and the main cause of mortality is sepsis. In our experience, postoperative mortality in the early group was three times higher than in the global LT series at our hospital (6.6%). However, the mortality rate of the late group (10%) was only slightly higher than that of the initial LT.
As in our experience, most series show better survival rates after late or elective retransplantation than after early or urgent LRT.13–17 The results of certain Spanish groups either show no differences between early and late14 or show even better results after early LRT. In these two series, LRT due to HCV recurrence probably still carried a lot of weight, as they were from the period in which the current selection criteria were not applied in this specific group of patients. For this reason, it was established that LRT for recurrence of HCV cirrhosis would only be indicated in low-risk patients,18,19 which is applicable to most patients today given the availability of highly effective antiviral treatment.
Although data from previous studies show worse survival after LRT than after an initial LT, if we rely on more recent series, and especially the results of our study, the five-year actuarial survival rates for LRT in the last two periods analyzed (2007–2012 and 2013–2018) were 70% and 75%, respectively. These data are absolutely comparable to an initial LT. In this overall improvement, the decline in LRT due to HCV recurrence in recent years probably plays a very important role. Likewise, if we look at the most frequent indication for late LRT, the five-year actuarial survival of LRT due to ischemic cholangitis exceeds 75%. Although previous studies suggest that the indication of LRT does not clearly affect the results, the conclusions are different depending on the studies.17
Apart from the decrease in the indication for LRT due to HCV, the improved results in the last decade are also due to a greater selection of patients. The Rosen score,20 used by our group since 2012 (like most Spanish hospitals), makes it possible to rule out higher risk patients for late LRT. We emphasize the use of the Rosen score as a selection criterion, as we consider it to be the best validated score in this context. The usefulness of MELD in assessing survival after LRT has not been as well studied. The median Rosen score of the retransplanted patients after 2012 was 14 (IQR 13–18). One drawback of our study is that it is based on retransplanted patients and, therefore, we do not have data on the patients in whom LRT was ruled out due to their severe condition.
The LRT raises an ethical dilemma due to different factors that have been the subject of debate since the beginning of the history of LT. It is evident that, individually, in the event of graft failure, LRT is the best and only solution for that patient. But LRT reduces access to LT for patients who are awaiting their first LT and who, on the other hand, will have better survival options. The transplant community must find a balance between individual care and the obligation to make decisions with an eye on the common good. Unlike other medical decisions, the disparity between the need for grafts and their availability requires a decision process based on the classic ethical principles of autonomy, non-maleficence, beneficence, justice, utility, dignity and honesty.6
According to our results, early LRT has worse results than late LRT. However, despite the worse results, it seems ethically necessary to offer the patient a second chance when the initial LT has failed.
Morbidity, mortality and long-term survival rates in the case of LRT currently have comparable results compared to an initial LT, especially in the case of indication for ischemic cholangitis. These results even exceed the target established by the SETH consensus document on expanded criteria (50% over five years).8
Thus, in conclusion, LRT is an acceptable indication in the current context of expanded LT criteria.
Conflict of interestThe authors of this study have no conflict of interests to declare.
The authors would like to thank Bernat Huguet for refining the data and creating the statistical analysis.
Please cite this article as: Lladó L, Lopez-Dominguez J, Ramos E, Cachero A, Mils K, Baliellas C, et al. ¿Está justificado el retrasplante hepático en la era actual? Cir Esp. 2021;99:339–345.