We have read with interest the article by Dr. de la Plaza Llamas et al.1 about pneumomediastinum and cervical emphysema as initial signs in colorectal anastomotic dehiscence. Recently, we had the opportunity to treat a similar case, and its exceptional nature has made us inclined to share our experience and to comment on some details of the case in question.
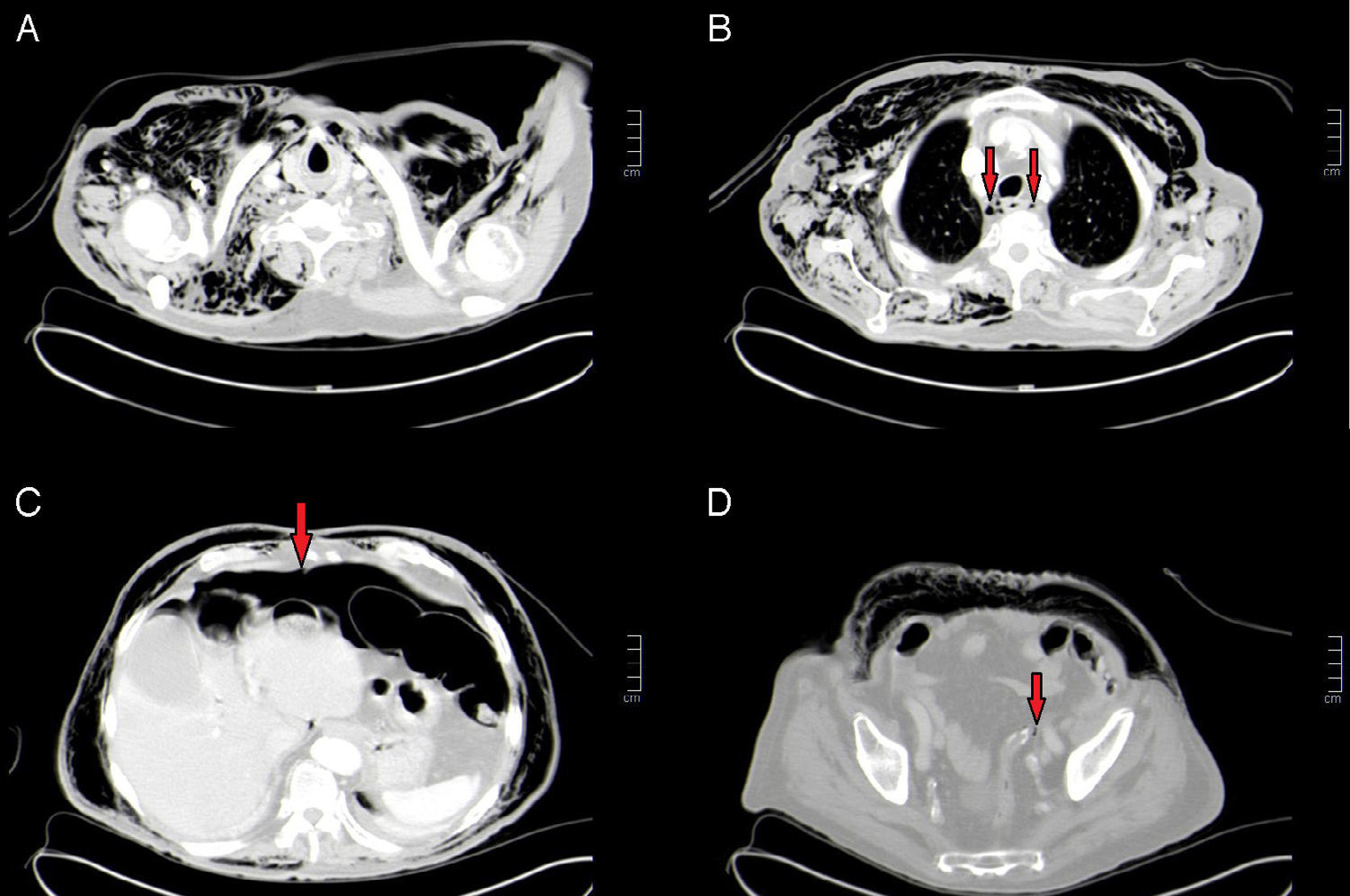
The patient is an 85-year-old male who was being studied for iron-deficiency anaemia and was diagnosed with sigmoid adenocarcinoma. Thoracoabdominal CT scan showed no evidence of metastatic disease, with a reported radiological stage of T2N0M0. He was treated by a laparoscopic approach, involving sigmoidectomy with mechanical end-to-end colorectal anastomosis. The patient progressed favourably but presented marked supraclavicular cervical emphysema on the 4th day post-op, which extended to the upper extremities, thorax and abdomen, with no associated symptoms of abdominal pain. Thoracoabdominal CT scan demonstrated important pneumomediastinum and cervical emphysema (Fig. 1A and B), moderate abdominal pneumoperitoneum in the supramesocolic compartment (Fig. 1C), 2 minimal bubbles in the vicinity of the colorectal anastomosis (Fig. 1D) and no presence of liquid or other alterations. A new laparoscopic procedure detected a punctiform dehiscence at the anterior side of the colorectal anastomosis, evidence of which was seen with an air test, although there was no presence of associated peritonitis. The anastomosis was resected and a new mechanical end-to-end colorectal anastomosis was created. During the postoperative period, the patient evolved favourably, with spontaneous resolution of the emphysema after having received no specific treatment. The patient was discharged 7 days after the reoperation.
(A) Axial CT image showing anterior and posterior supraclavicular cervical emphysema; (B) axial CT image showing pneumomediastinum (arrows); (C) axial CT scan showing moderate pneumoperitoneum (arrow); (D) axial CT image showing a minimal extraluminal bubble in the vicinity of the colorectal anastomosis (arrow).
Pneumomediastinum and cervical emphysema are uncommon signs at the onset of colorectal anastomosis dehiscence,1,2 although they have also been observed in cases of perforated diverticulitis3 and perforation after endoscopic polypectomy.4 As indicated in the literature, a delayed diagnosis determines the prognosis.2 In our case, the diagnosis occurred in the first few days post-op, which provided for early treatment and avoided the development of peritonitis and associated morbidity, at which time we were able to construct a new anastomosis. In the cited case,1 the fact that dehiscence was not diagnosed until 11 days after surgery (because the patient presented no symptoms during hospitalisation), lengthened the hospital stay to 60 days, with what we can only assume was important postoperative morbidity, and made it impossible to perform an anastomosis during the operation.
We would like to emphasise that, although pneumomediastinum and cervical emphysema can be the first signs of presentation of colorectal anastomosis dehiscence, any delay in diagnosis and intraabdominal conditions that are encountered will determine the therapeutic approach and prognosis. This should not necessarily mean a severe condition associated with high morbidity and prolonged hospital stay.
Please cite this article as: Peña Ros E, Parra Baños PA, Candel Arenas MF, Albarracín Marín-Blázquez A. ¿Es el neumomediastino y enfisema cervical un signo de mal pronóstico en la dehiscencia de anastomosis colorrectal? Cir Esp. 2016;94:202–203.