Cholecystocolic fistulas (CCF) are a late complication of long-standing gallstone disease.1 The atypical presentation and challenging diagnosis make CCF a condition limited to case reports and small series.2
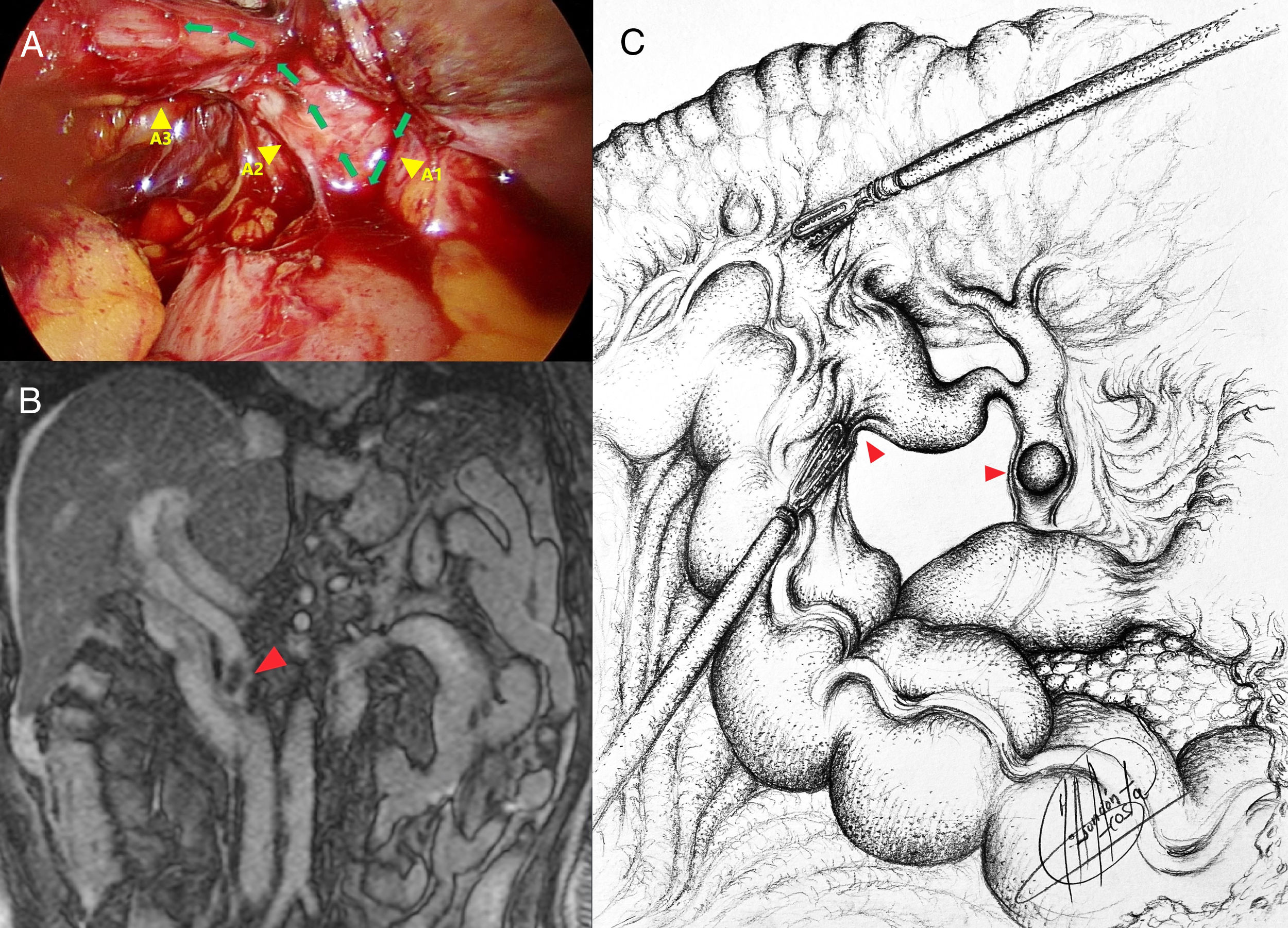
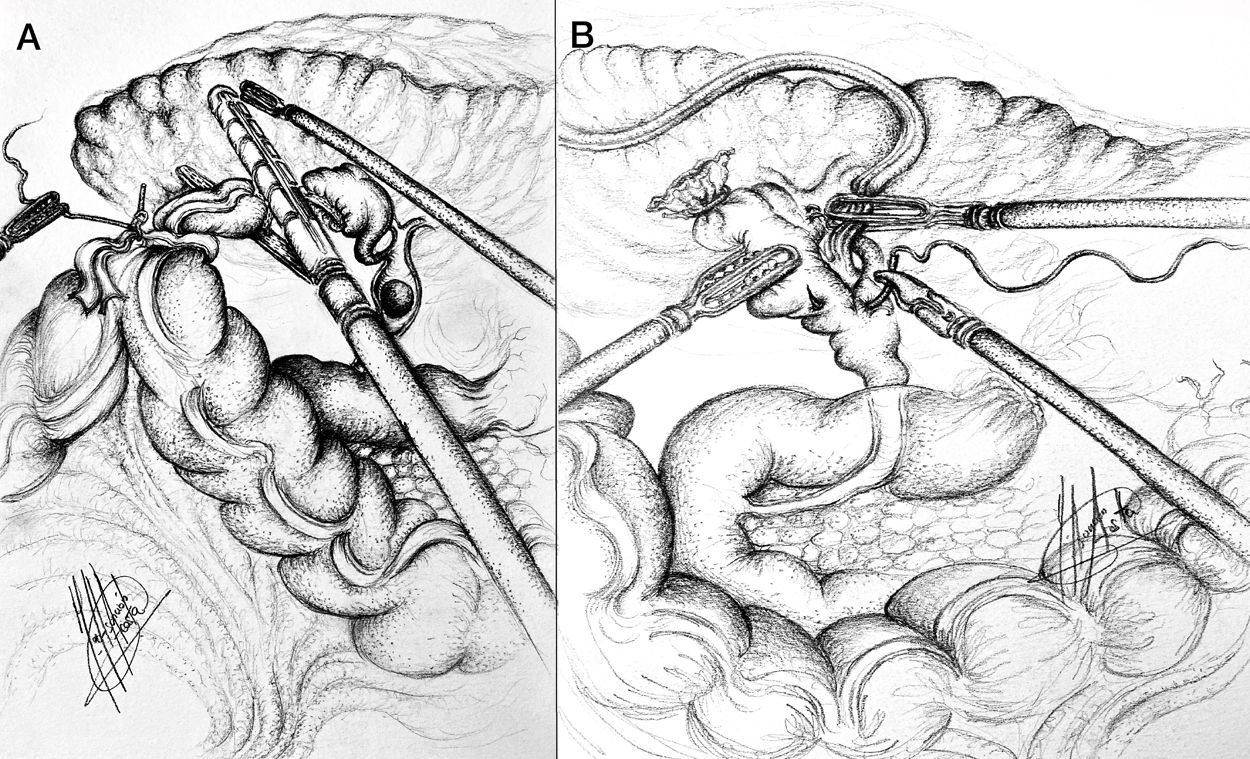
We present the case of a 58 year old man with past medical history of subtotal cholecystectomy 16 years ago followed by a Roux-en-Y gastric bypass (RYGB) 2 years later. After the bariatric procedure he presented diarrhoea that progressively worsened and developed deranged liver function tests (LFT) (total bilirrubin 42 µmol/L, AP 146 IU/L, ALT 276 IU/L, GGT 619 IU/L), suggesting obstruction of the common bile duct (CBD). Concomitantly the patient developed scurvy-like symptoms (gum bleeding and easy bruising). Abdominal CT and MRCP showed a CCF and obstruction of the CBD (diameter: 10 mm) due to gallstones. Endoscopic retrograde cholangiopancreatography (ERCP) and percutaneous hepatic cholangiogram (PTC) were not performed preoperatively due to the RYGB and the need of a completion cholecystectomy and correction of the fistula. At laparoscopy a CCF between the gallbladder remnant and the hepatic flexure of the colon was found (Fig. 1). The colonic portion was divided with endostapler (Fig. 2A), and completion cholecystectomy was performed together with transductal bile duct exploration through a choledochotomy due to the poor general condition of the patient, the hiliar inflammation, and the thought that a transcystic approach would be more time-consuming. The choledochotomy was closed over a T-tube to avoid a postoperative bile leak in a frail patient (Fig. 2B). Eight weeks after surgery the T-tube was removed after performing a clear cholangiogram. The patient’s diarrhoea, nutritional status and LFT improved after surgery; 20 months after the procedure he is asymptomatic.
Cholecystocolic fistula between the gallbladder remnant and the hepatic flexure of the colon. (A) Intraoperative findings with arrows marking the common bile duct (A1), gallbladder remnant (A2) and fistula to the hepatic flexure of the colon (A3). (B) Preoperative MRI, gallstone in common bile duct (arrowhead). (C) Drawing of the cholecystocolic fistula and gallstone in the common bile duct (arrowheads).
Cholecystoenteric fistulas (CEF) are consequence of long-standing gallstone disease due to a chronic inflammatory process. They affect 3%–5% of patients with cholelithiasis and can be found in 0.06%–4.8% of patients undergoing biliary surgery.1,3 CCF are the second most common type of CEF (6.3%–26.5%) after cholecystoduodenal.1–4 They are usually located at the hepatic flexure.4 Mean age of patients at diagnosis in Western countries is 70.8 years. However, sporadic cases before the age of 40–50 have been reported. CCF are more frequent in women (female:male ratio 2.47:1).1
Symptoms are usually non-specific.1,2 The triad of cholerheic diarrhoea, right hypocondrium pain and cholangitis is the typical clinical presentation of CCF. However, most of them present features of uncomplicated gallstone disease.1,3–5 Diarrhoea is the most commonly reported symptom in the chronic onset (71%) due to the laxative effects of the bile acids that bypass the distal ileum and reach the transverse colon unabsorbed.1,5 In our case the diarrhoea caused by the malabsorptive effect of the RYGB was worsened due to CBD obstruction, which promoted retrograde drainage of most of the bile through the fistula. This was initially exclusively attributed to the RYGB, as it was not known that the patient had a subtotal cholecystectomy. Depending on the severity of the diarrhoea a malabsorptive syndrome can develop, which can be responsible for fat-soluble vitamin deficiencies (including vitamin K).1,5–7 Moreover, patients who undergo bariatric surgery, especially those with a major malabsorptive component, are prone to develop vitamin K deficiency.7 It is usually associated to bleeding diathesis in patients with malabsorption syndromes,6,7 mimicking occasionally scurvy’s clinical presentation as our case.
Life-threatening complications can occur in some cases of CCF (0.13%): obstruction (gallstone impactation in the sigmoid colon), massive bleeding, liver abscess, cholangitis and septic shock.1,2,4,5 The risk of biliary sepsis is higher due to the communication between the gallbladder and a bowel with high bacterial load.2,4 Gallbladder carcinoma can coexist with CCF (0.1%). A frozen section of the specimen should always be taken.1,4
Most CCF are diagnosed intraoperatively. A high degree of suspicion is mandatory: a thick-walled contracted gallbladder stuck firmly to adjacent viscera in a patient with long-standing gallstone disease should alert the surgeon.1,3 Preoperative diagnosis is achieved in 7.9%–31% of the cases.1,4,8 Pneumobilia at plain X-ray (pathognomonic) is often absent. Barium enema has a high specificity but low sensitivity. ERCP and CT scan with coronal reconstructions are the most valuable diagnostic tools. Colonoscopy, liver scintigraphy, MRI and endoscopic US have variable results.1,8
No consensus has been developed to address the optimal management of CCF.2,4 The treatment will depend on the clinical situation of the patient and the complexity of the fistula. The fistula isolation and the repair of the colon should be done before cholecystectomy to avoid contamination of the abdomen by colonic bacteria.3,4 CBD imaging should always be performed to rule out choledocholithiasis. Complex fistulas may require multivisceral or atypical gallbladder resections.1 The use of intraabdominal drains, although controversial, is recommended.2–4,8 ERCP can be an alternative to surgery in frail patients or with choledocholithiasis to encourage CCF closure by reducing bile pressure in the gallbladder.1 Laparoscopic procedures are feasible but should be performed in high-volume centres by experienced surgeons as it is a demanding procedure (55% of early conversions) with a high incidence of intraoperative complications.1,3,4
CCF are an unusual condition. Preoperative and intraoperative diagnosis are challenging. The treatment should be tailored to each case. CCF is no longer a contraindication for laparoscopic surgery. However, it should only be performed by experienced surgeons. Threshold to conversion to open surgery should be low.1,3,4
Please cite this article as: Senra F, Acosta A, Doran S, Isla A. Manejo laparoscópico de una fístula colecistocólica en un paciente con un bypass gástrico con síntomas de seudoescorbuto: un reto quirúrgico. Cir Esp. 2021;99:471–473.