Gastrointestinal hemorrhage due to varices is one of the most serious complications of portal hypertension (PH).1 Esophagogastric varices appear in 50%–60% of cirrhotic patients. Variceal bleeding has a risk of recurrence of 70% within 2 years of the first episode. The mortality rate is 40%–70%.2 In cirrhotic patients, 60%–80% of gastrointestinal bleeding is due to esophageal varices and 7% to gastric varices. Gastric varices are less frequent, but those located in the fundus present a very high risk for bleeding.3
Treatment of varices is endoscopic in association with beta-blockers to prevent recurrence. Hemorrhage due to fundal varices has a poorer control rate and a higher rate of recurrence. In patients in whom this therapy fails, surgery is an alternative if liver function is preserved or liver transplantation is contraindicated.1 There are 2 large groups of surgical techniques: portosystemic shunts and devascularizations.4,5 In patients with good hepatic function and portal system thrombosis, devascularizations are the surgical treatment of choice. The classic technique by Sugiura involves esophagogastric devascularization and esophageal transection. The Hassab technique associates transection of the fundus rather than the esophagus to reduce any associated complications, which decreases recurrence associated with fundal varices.6 A mixed technique was also proposed combining periesophagogastric devascularization, fundectomy and splenectomy to obtain greater control of long-term bleeding.7 Recently, the Northwestern University of Chicago group has reported the utility of transsplenic percutaneous portal revascularization associated with transjugular portosystemic shunt (TIPS) in patients with thrombosis of the main portal trunk prior to transplantation.8
We present 3 cases of recurrent hemorrhage secondary to esophagogastric varices with portosplenomesenteric thrombosis and preserved liver function treated with the Han technique, along with long-term follow-up.
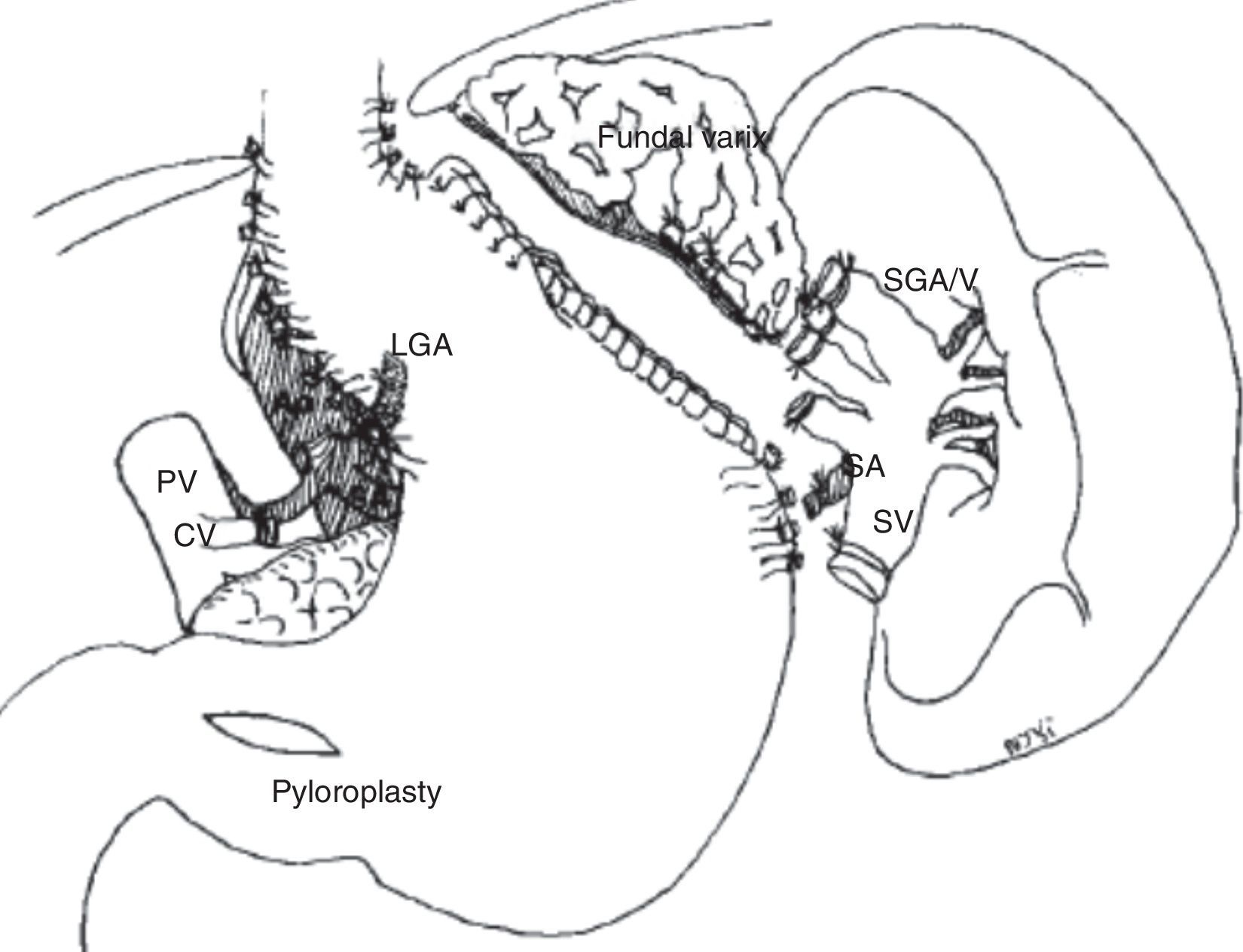
The surgical technique used included a left subcostal incision, splenectomy with ligature of the short vessels as well as the splenic hilum, anterior and posterior periesophageal devascularization of the distal 5cm, perigastric devascularization of both curvatures from the cardia to the incisura angularis, ligation of varices and fundectomy of the affected area using mechanical transection with suture reinforcement. In one patient, pyloroplasty was performed to improve gastric emptying due to the suspicion of left vagal injury of the hiatus (Fig. 1).
Esophagogastric devascularization in accordance with the Han technique (Han et al.7).
The patient is a 49-year-old male with alcoholic cirrhosis (diagnosed in 2003) associated with complete thrombosis of the portal system and recurrent variceal hemorrhage, despite multiple endoscopic treatments with ligation, sclerosis and cyanoacrylate of the fundal varices. In 2004, the patient underwent the Han technique. Postoperative evolution was satisfactory, requiring antibiotic treatment for a residual intra-abdominal collection. Twelve years after surgery, the patient has no esophagogastric varices and has presented no recurrent bleeding.
Case 2The patient is a 57-year-old woman diagnosed with congenital hepatic fibrosis in 1996, pancytopenia secondary to hypersplenism and several episodes of hemorrhage due to esophageal and fundal varices, which were being followed endoscopically. In 2005, a TIPS was placed, which led to thrombosis affecting the portomesenteric axis. The Han technique was then performed. The patient progressed favorably, although she did present fever without a source that was treated empirically with antibiotics. After 10 years of follow-up, no recurrence of digestive hemorrhage has been observed. Endoscopy has revealed grade 1 esophageal varices but no fundal varices.
Case 3The patient is a 59-year-old woman with factor V deficiency and essential thrombocytosis associated with portosplenomesenteric venous thrombosis, as well as several episodes of severe gastrointestinal bleeding secondary to grade IV esophageal varices and fundal varices requiring ICU hospitalization on several occasions. The patient underwent the Han technique and required reoperation 24h later due to bleeding of the gastric transection line. The postoperative period was complicated by a pyloroplasty fistula, which was treated conservatively. The patient was discharged on the 30th postoperative day. After 2 years of follow-up, she is asymptomatic with no evidence of varices observed in the follow-up endoscopic studies.
Using this technique, Han et al. have reported a 5-year survival rate of 62% and a mortality rate of 17.7%, which has been reduced in recent years given the greater experience of surgeons, improved preoperative patient conditions and early indication for surgery. Major complications and mortality were related to previous failed endoscopic controls and complications of cirrhosis, such as decompensation and hepatocarcinoma.7 In the long term, the Han group has published recurrence rates of 5%–40%, mainly due to esophageal varices, which can be more easily treated endoscopically.9
In our experience, the Han technique in selected patients has been associated with low morbidity and excellent long-term results. This technique should be considered in patients with recurrent digestive hemorrhages associated with fundal varices with good liver function or in cirrhotic patients with contraindication to liver transplantation, especially if there is thrombosis of the portosplenomesenteric axis.
Authorship ContributionAll the authors have contributed equally to the data collection, composition of the article, critical review and approval of the final version of the text.
Please cite this article as: Pacheco D, Marcos JL, Pinto P, Rodríguez M, Velasco R. Resultados a largo plazo de la devascularización esofagogástrica, según técnica de Han, en el tratamiento de la hemorragia digestiva secundaria a varices esofagogástricas y trombosis portal. Cir Esp. 2017;95:54–56.