Magnetic devices have been successfully used in bariatric surgery. To the date, the only reported use of the magnet was for liver retraction. Our purpose in this study is to demonstrate the safety and viability of using a magnetic system in different steps in single port and reduced port bariatric surgery.
MethodsProspective and observational study was performed. Patients older than 18 years, undergoing primary laparoscopic sleeve gastrectomy (SG), one-anastomosis gastric bypass (OAGB), and Roux-en-Y gastric bypass (RYGB) or revisional surgery by single-port or reduced-port approach between July 2020 and June 2021 were included.
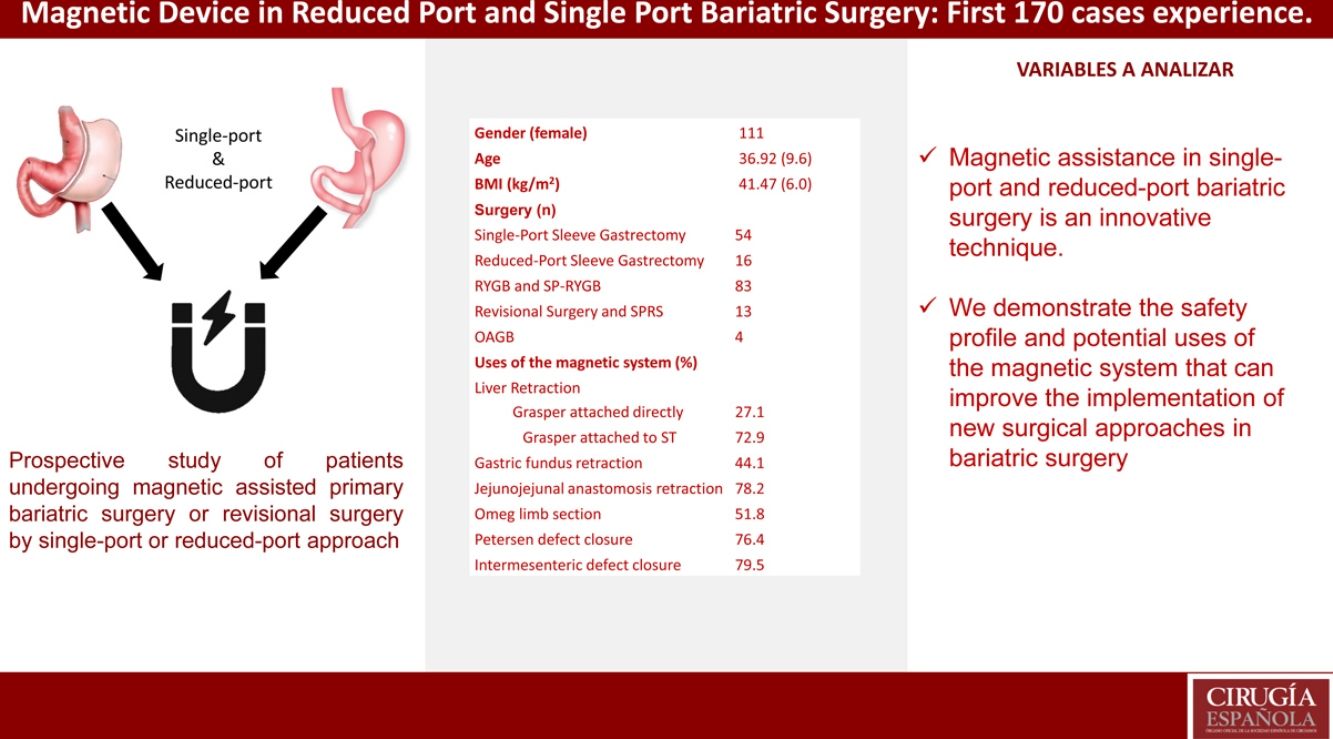
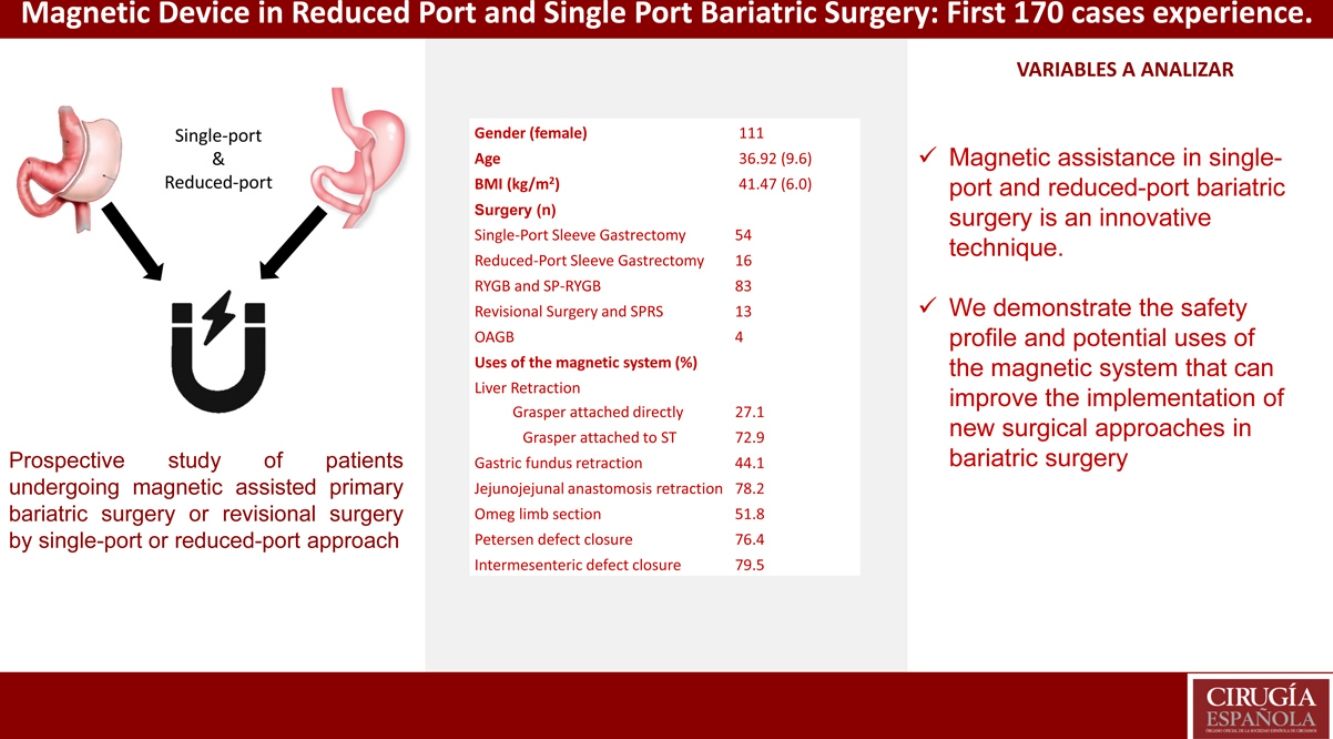
ResultsA total of 170 patients (mean BMI, 41.47kg/m2; mean age 36.92 yrs) completed laparoscopic bariatric surgery (54 single-port sleeve gastrectomy [SPSG], 16 reduced-port SG, 83 RYGB, 4 OAGB and 14 revision surgeries), using the magnetic surgical system in different steps of the surgery. Mean surgical time for SPSG and reduced-port SG was 65.52min and 59.36min respectively; and for RYGB 74.19min, OAGB 70.98min, and revisional surgeries 88.38min. As for intraoperative complications, 2.94% mild liver laceration without significant bleeding was reported. There were no 30-day mortalities and no major complications.
ConclusionMagnetic assistance in single-port and reduced-port bariatric surgery is an innovative technique. With this prospective study we attempt to demonstrate the safety profile and potential uses that may improve the implementation of new surgical approaches in bariatric surgery.
Los dispositivos magnéticos se han usado satisfactoriamente en cirugía bariátrica. Hasta la fecha, el único uso reportado de los imanes ha sido para la retracción hepática. Nuestro propósito con este estudio es demostrar la seguridad y viabilidad de usar dispositivos magnéticos en diferentes pasos de la cirugía bariátrica por puerto único y por puerto reducido.
MétodosSe realizó un estudio prospectivo y observacional. Se incluyeron pacientes mayores de 18 años que fueron sometidos a cirugía laparoscópica primaria de manga gástrica (MG), bypass gástrico de una sola anastomosis (BAGUA), bypass gástrico en Y de Roux (BGYR) y cirugía de revisión por abordaje de puerto único o puerto reducido entre los meses de julio de 2020 y junio de 2021.
ResultadosA un total de 170 pacientes (media IMC, 41,47 kg/m2; media edad 36,92 años) se les realizó una cirugía bariátrica laparoscópica (54 MG por puerto único, 16 MG por puerto reducido, 4 BAGUA y 14 cirugías de revisión) utilizando el dispositivo magnético en diferentes pasos del proceso quirúrgico. El tiempo promedio de la MG por puerto único y MG por puerto reducido fueron 65,52 min y 59,36 min, respectivamente; mientras que para BGYR 74,19 min, BAGUA 70,98 min y cirugías de revisión 88,38 min. Entre las complicaciones intraoperatorias se reportaron 2,94% de laceraciones hepáticas leves sin sangrado significante. No hubo ningún porcentaje de mortalidad ni de complicaciones mayores a los 30 días.
ConclusionesLa asistencia magnética en cirugía bariátrica por puerto único y por puerto reducido es una técnica innovadora. Con este estudio prospectivo intentamos demostrar el perfil de seguridad y los usos potenciales que pueden mejorar la implementación de nuevos abordajes quirúrgicos en cirugía bariátrica.
Obesity is a global problem that affects 40% of the worldwide population, mostly in developed and developing countries.1 Obesity is a risk factor for diabetes mellitus, hypertension, sleep apnea hypopnea syndrome (SAHS), cancer, and other diseases.2 Bariatric surgery represents the best treatment option for achieving a significant and maintained weight loss and control or remission of comorbidities associated with obesity.3
Annually, thousands of bariatric procedures are performed worldwide, among them, the most common ones are sleeve gastrectomy (LSG) and Roux-en-Y gastric bypass (RYGB).4 As bariatric surgery and minimally invasive surgery (MIS) advances, there is a growing demand from science and patients to further improve the surgical techniques employed.
In 2007, the concept of magnetic surgery was introduced.5 Since then, this device has been successfully used in several procedures, such as cholecystectomy, colorectal surgery, and bariatric surgery. According to these studies, the only use reported for the magnet in bariatric surgery was for liver retraction.6,7
Our purpose in this study is to demonstrate the safety and viability of using the magnetic system in bariatric surgery beyond liver retraction. It can be successfully used in some important steps in the procedures, like gastric fundus retraction, jejunojejunal anastomosis confection, intermesenteric and Petersen's defect closure, among others. Apart from this, the use of the magnetics system in bariatric surgery can promote the use of reduced-port and single-port technique safely, as it can improve the visualization of the gastroesophageal junction in single-port sleeve gastrectomy and reduced-port gastric bypass, facilitating the visualization and presentation of the tissues in the aforementioned steps.
MethodsA prospective and observational study was performed. Patients older than 18 years, undergoing primary laparoscopic sleeve gastrectomy (SG), one-anastomosis gastric bypass (OAGB), and Roux-en-Y gastric bypass (RYGB) or revisional surgery in a bariatric surgery unit that is based at three locations in which the magnet system has been used were included. In this study, we report our experience with our first 170 cases reached; achieved during the months of July 2020–June 2021. Exclusion criteria included uncontrolled co-morbidities; patients with pacemakers, defibrillators, or other electromedical implants; abnormal coagulation blood tests; and patients with hepatic diseases. This study was approved by the Institutional Review Board at the institution where the study was performed and informed consent was obtained from all the participants included in the study.
Operative techniquePrimary and revisional surgery were performed in French position. Pneumoperitoneum was established with Veress needle at 15YmmHg. Four trocars were commonly used: one trocar (12mm) in the umbilicus, two trocars in the right hypochondrium (5mm), and one trocar (3mm) in the left hypochondrium. For single-port technique, the device was placed in the umbilicus and an additional trocar in the right hypochondrium (5mm).
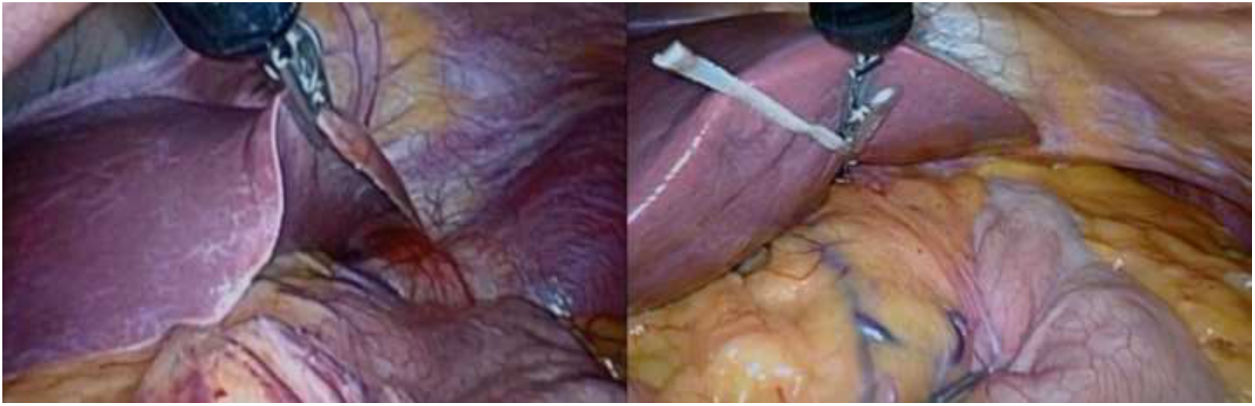
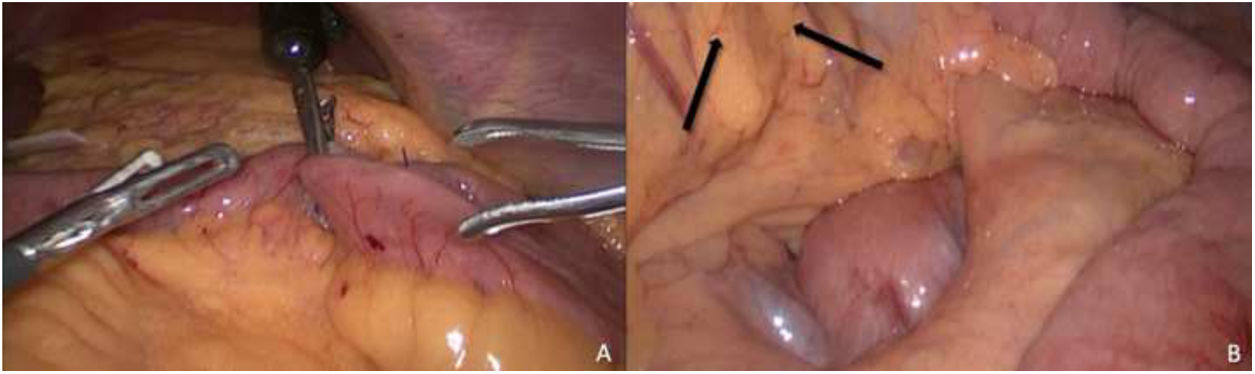
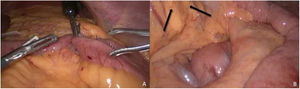
In SG, we begin making the hepatic retraction with the grasper couple with the magnet or/and silastic tube attached to the right diaphragmatic crus (Fig. 1). We start the dissection of the major curvature with bipolar energy from the incisura angularis in cephalic direction up to the His angle. When reaching the division of the short vessels, the grasper couple to the magnet is positioned in the fundus to retract the stomach (Fig. 2) obtaining a better exposure; the division continues until the gastroesophageal junction. Once the division is complete, the vertical stapling of the stomach is started 4cm from the pylorus using a 38Fr. Bougie. We generally use four 60mm cartridges (1 green for antrum, 4 blue for gastric body) with an automatic linear stapler, and afterward the reinforcement of the gastric staple line is made with non-absorbable polypropylene 2/0 suture.
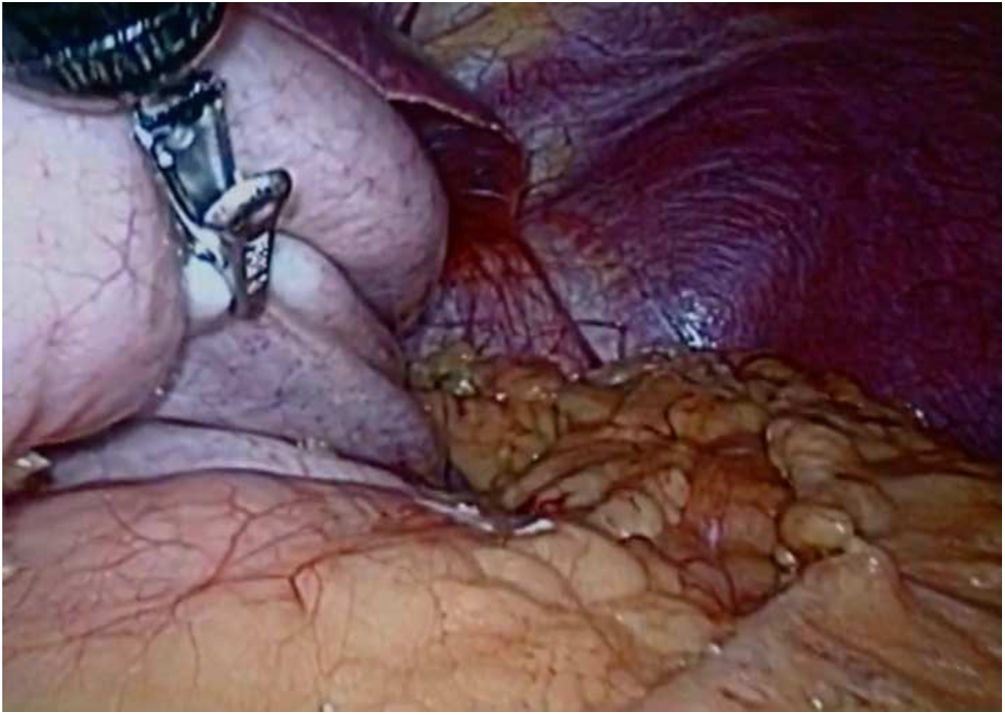
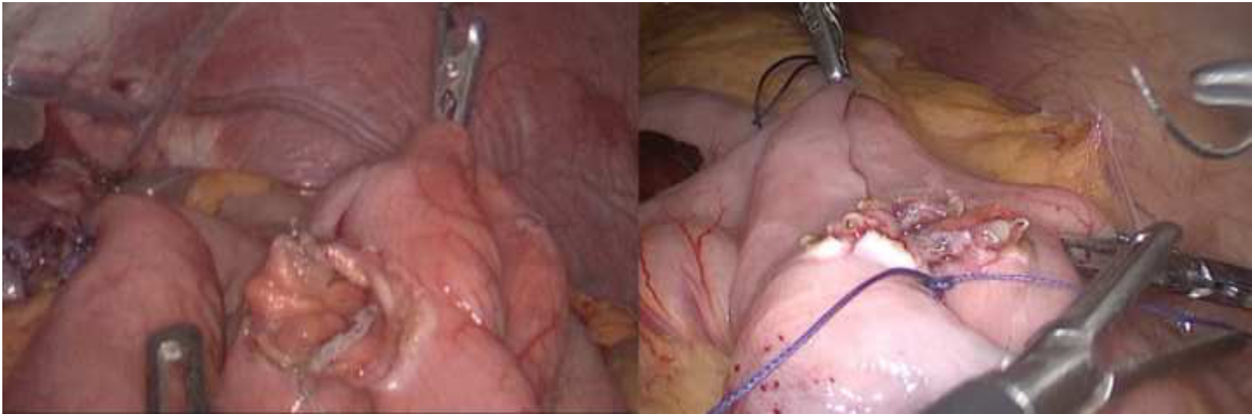
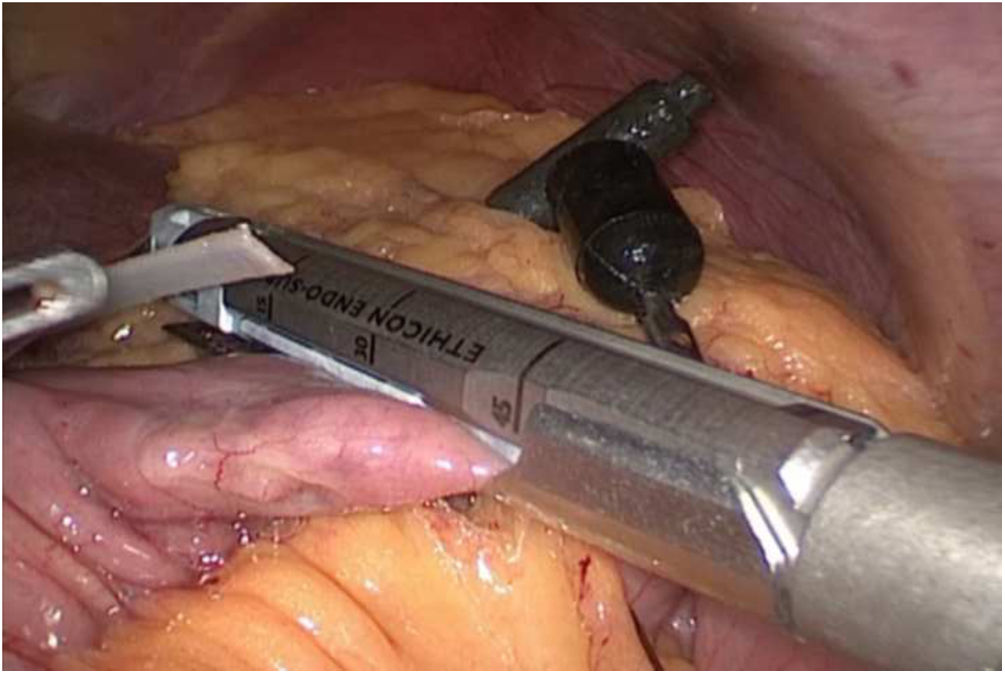
In the case of RYGB, we began using a magnetic grasper for liver retraction (Fig. 1) as previously described. We started with the creation of a 30ml pouch, starting with a horizontal section with an automatic linear stapler with 45mm blue cartridge and 60mm two blue cartridges sections towards the His angle to finish the pouch. Continuing with the procedure, the Treitz angle is located and measured between 70 and 100cm for the biliopancreatic limb from this point where the gastrojejunal anastomosis will be performed with a 45mm blue cartridge. Then, with the gastrojejunal anastomosis completed, the measurement of the alimentary limb at 100cm is made and the jejunojejunal anastomosis is performed with 45mm white cartridge; to close the anastomosis, the grasper coupled with the magnet is positioned on the upper part of the anastomosis to retract and assist the closure of the opening (Fig. 3). Posteriorly the magnet is positioned on the limb or to make the retraction and to assist for the section of the omega with a 45mm white cartridge (Fig. 4) to finish with the Roux-en-Y design. The intermesenteric defect closure is assisted with the magnet positioned in the same way as for the retraction of the jejunojejunal anastomosis, then also the Petersen defect is closed with the magnet positioned on the transverse mesocolon for retraction (Fig. 5). A methylene blue dye leakage test is performed and a sentinel drain (Blake 19F; Ethicon) is left at the gastrojejunal anastomosis. The magnetic device allowed to perform all the stapling through one 12mm trocar located in the umbilicus.
The OAGB was performed under the standard technique as previously described of confection of the gastro-jejunal anastomosis at 200cm from the angle of Treitz. Different types of revision surgeries were performed, in all of them the magnetic system was used in different steps, similarly to the ones previously mentioned.
In this study, the magnetic surgical system used was the introduced by Dr. Dominguez in 2007.5 The system comprises an external neodymium magnet, a grasper coupled with magnet, grasper with magnet plus silastic tube, and a magnetic enhancer (Fig. 6).
The primary endpoint of the study was the implementation of the magnet device, safety, and feasibility in primary and revisional surgery. Secondary endpoints included intra and postoperative complications, related and non-related directly to the use of the magnetic system.
The variables measured were demographic characteristics (gender, age, race, BMI, comorbidities). Abdominal circumference was measured at the midpoint between the last rib and the iliac crest border. Operative variables like operative intraabdominal time, steps in which the magnet was used, conversion rate, device malfunction and the need for additional ports, among others were recorded. Length of hospital stay was also assessed.
ProtocolAfter the patients have met the inclusion criteria, they are taken to elective surgery after discussion with the multidisciplinary team. The magnet system is used on all patients in our unit who undergo primary bariatric surgery or revision surgery. Depending on the type of surgery being performed, with this study we have elaborated a series of steps in which it can be used.
The step which is used in all the cases of this series is for liver retraction in which we have two options to perform it. As a first option with the magnetic grasper attached directly on the border of the liver at the site where the greatest exposure of the surgical field to be worked on can be achieved. And as a second option using a grasper with a silastic tube and to this tube we attached de magnetic grasper for retraction. One or the other is used depending on the intraoperative liver dimensions, morphology evidenced or any disease associated.
For the single-port or port-reduced gastric sleeve we have developed one step in which it can be used for surgical assistance. In this step the magnetic grasper is used and positioned at some point of the gastric body in the left direction to achieve retraction and the subsequent dissection of the short vessels and also exposure of the His angle. This step is used depending on the size of the patient's stomach and the degree of retraction that can be achieved In difficult cases we can use a second magnetic grasper attached to the gastric antrum to move the stomach to the right inferior quadrant of the patient simultaneal.
In the case of magnet-assisted Roux-en-Y gastric bypass the magnet system was implemented mainly in four steps. In the first step that is developed is at the time of closing the opening of the jejunojejunal anastomosis; the magnetic grasper is placed on a stitch previously made to make the approximation of the limbs prior to the enterotomies. The previously mentioned step is used according to the patient's intra-abdominal space and the appropriate degree of retraction that can be achieved to close the anastomosis. We also implemented the use of the magnetic system to assist in the closure of mesenteric defects. In the closure of the intermesenteric defect, the magnetic grasper is positioned in the same way as the retraction is performed for the closure of jejunojejunal anastomosis, either directly on the limb or the suture point. On the other hand, for the closure of the Petersen defect, the magnetic grasper is positioned at the point of greatest retraction which can be reached in the transverse mesocolon. The use of the magnet system to assist defect closure depends on the size of the defect, the degree of visceral adiposity, the patient's anatomical disposition and the intra-abdominal space available. Finally, the magnetic grasper is used for the section of the omega, in this step it is positioned at a point between 8 to 10cm from the gastrojejunal anastomosis that allows an appropriate midpoint to make the opening in the mesenteric border of the limb and with a line stapler section the limb. The considerations that are taken into account to perform the previously mentioned step are the degree of retraction and tension that can be reached to perform the correct section of the limb.
In the case of OAGB and revision surgery, the magnet system is used under the same protocol previously mentioned according to the step in which it can be performed.
Statistical analysisStatistical analysis was performed using SPSS v27 for MacOS. A descriptive analysis of our sample was performed, with our parametric variables reported as mean and standard deviation (SD). Intraoperative and postoperative outcomes are reported, as well as the percentage of use of the magnetic device.
ResultsA total of 170 patients met the inclusion criteria and completed laparoscopic bariatric surgery using the magnetic surgical system in different steps of the surgery. Of all the patients within this study, 111 of them were females and 59 of them males, with a mean age of 36.92 years (range 13–64 years). Mean preoperative body mass index (BMI) was 41.47kg/m2 (range 29–64kg/m2). There was one case reported with a BMI of 29kg/m2 from a revision surgery following a sleeve gastrectomy with gastroesophageal reflux refractory to medical treatment.
Regarding the comorbidities of our patients 44 patients had a previous diagnosis of hypertension, 35 type 2 diabetes mellitus/insulin resistance, 27 non-alcoholic fatty liver disease, 15 dyslipidemia, and 5 sleep apnea hypopnea syndrome. Mean waist circumference was 113.1cm (80–179cm). Anthropometric characteristics are summarized in Table 1.
Participant demographic characteristics.
| Attribute | Results |
|---|---|
| Gender | |
| Female | 111 |
| Male | 59 |
| Age | |
| Average (SD) | 36.92 (9.6) |
| Min. | 13 |
| Max. | 64 |
| BMI (kg/m2) | |
| Average (SD) | 41.47 (6.0) |
| Min. | 29 |
| Max. | 64 |
| Co-morbidities | |
| HTA | 44 |
| DM2 or insulin resistance | 35 |
| NAFLD | 27 |
| Dyslipidemia | 15 |
| OSA | 5 |
| Abdominal circunference (cm) | |
| Average | 113.1 |
SD, standard deviation; BMI, body mass index; HTA, hypertension; DM2, diabetes type two; NAFLD, non-alcoholic fatty liver disease; OSA, obstructive sleep apnea.
Our series included 157 primary surgeries and 13 revisions. The primary cases were 70 sleeve gastrectomies (54 single-port and 16 reduced-port), 83 Roux-en-Y gastric bypass (79 reduced-port and 4 single-port), and 4 One anastomosis gastric bypass (OAGB). In the case of the revision surgeries, there were a total of 13 as previously mentioned which included 2 single-port conversions from SG to RYGB, 5 reduced-port conversions from SG to RYGB, 1 conversion from endoscopic plicature to RYGB, 1 conversion from laparoscopic plicature to SG, 1 conversion from vertical banded gastroplasty to OAGB, 2 biliopancreatic limb distalization and 1 pouch reconfection. All procedures were performed by a single-port or reduced-port approach (4 ports, as described in the Operative technique section).
The magnet system was used in 100% of the cases for liver retraction, it was used in 27.1% of cases with the grasper attached directly to the liver and in 72.9% of cases with the grasper attached to a silastic tube. For gastric fundus retraction either to the left or right side of the surgical field was used in 44.1% of cases. Jejujonojejunal anastomosis retraction from the upper side for assistance to its closure was used in 78.2% of the surgeries where this step was involved. The magnet system was also used to assist in the closure of Petersen and inter mesenteric spaces in 76.4% and 79.5% respectively. Finally, the magnet was used in 51.8% of the cases to retract the limb and section the omega loop in order to finish the confection of the RYGB. In 100% of primary and revision surgeries, the magnetic system was used in at least one surgical step.
The mean surgical time for single-port sleeve gastrectomy (SPSG) and reduced-port SG was 65.52 (SD, 18) min and 59.36 (SD, 16.7) min respectively, and for RYGB was 74.19 (SD, 22.2) min and for OAGB 70.98 (SD 8.7) min. Operative time for revisional surgeries averaged 88.38 (SD, 24.9) min. No device malfunction was reported in this study. Only in one case it was necessary to add an additional port during RYGB due to a severe grade of visceral fat to improve the triangulation and retraction. There were no conversions to open surgery. As for intraoperative complications, we only reported 2.94% of mild liver laceration without significant bleeding. There were no 30-day mortalities and no major complications reported; only 5.29% cases of minor complications that presented nausea and vomiting resolved with medical treatment. In our series, the average length of hospital stay was 1.17 (1–4) days. All the previously mentioned data are summarized in Table 2.
Intraoperative results through discharge.
| Attribute | Results |
|---|---|
| Surgery | |
| Single-port sleeve gastrectomy | 54 |
| Reduced-port sleeve gastrectomy | 16 |
| RYGB and SP-RYGB | 83 |
| Revisional surgery and SPRS | 13 |
| OAGB | 4 |
| Surgical time (average (SD), minutes) | |
| Single-port sleeve gastrectomy | 65.52 (18.0) |
| Reduced-port sleeve gastrectomy | 59.36 (16.7) |
| RYGB | 74.19 (22.2) |
| Revisional surgery | 88.38 (24.9) |
| OAGB | 70.98 (8.7) |
| Uses of the magnetic system (%) | |
| Liver retraction | |
| Grasper attached directly | 27.1 |
| Grasper attached to ST | 72.9 |
| Gastric fundus retraction | 44.1 |
| Jejunojejunal anastomosis retraction | 78.2 |
| Omega loop section | 51.8 |
| Petersen defect closure | 76.4 |
| Intermesenteric defect closure | 79.5 |
| Need for an additional port (N) | |
| Yes | 1 |
| No | 169 |
| Device malfunction (N) | |
| Yes | 0 |
| No | 170 |
| Conversions (%) | |
| Open surgery | 0 |
| Reintervention (N) | |
| Yes | 0 |
| No | 170 |
| Intraoperative complications (%) | |
| Low-grade hepatic laceration | 2.9 |
| 30-Day postoperative complications (%) | |
| Nause and vomiting | 5.2 |
| Length of hospital stay (d) | |
| Average (SD) | 1.17 (.43) |
SD, standard deviation; RYGB, roux-en-y gastric bypass; SP-RYGB, single port roux-en-y gastric bypass; SPRS, single port revisional surgery; OAGB, one anastomosis gastric bypass; ST, silastic tube.
This study aims to demonstrate the potential uses of magnetic devices in different steps in multiple bariatric procedures. The use of the magnet system can bring multiple benefits, among the possible most prominent would be the increased use of new minimally invasive techniques as reduced-port and single-port surgery with better visualization and presentation of the tissue and different organs.
Up to our knowledge, this is the study with the largest cohort of patients in which the magnet system was used in different types of bariatric surgeries, including SG, RYGB, OAGB, and revision surgeries. In addition to the multiple uses of the magnet system mentioned before, it allowed 37% of procedures performed by single port techniques and the rest by reduced-port approaches.
In our study, we also measured different anthropometric variables such as BMI and abdominal circumference. Demonstrating the viability and the technical use that can be given in patients with different characteristics that could influence the use of the magnet. For example, in patients who do not have so many difficult factors it can reduce the number of trocars used and in the case of complex patients it can improve the visualization of the surgical field as well as the retraction. It is important to highlight that in 100% of the surgeries it was possible to perform liver retraction regardless of the BMI.
The use of the magnet system for liver retraction in bariatric surgery has been reported in different studies with satisfactory results.6,7 It should be noted that following the same line, our study visualized the potential use of the magnet system beyond liver retraction. The magnetic system was used in multiple surgical steps with an intraoperative complication rate of 2.9%, conversion rate of 0%, and postoperative complication rate of 5.2%. Thus, we may demonstrate the safety profile of the use of magnets, without an increasement in intra and postoperative complications. The average operative time in our study was 71.1min, which is in accordance with those reported in other studies previously mentioned.
The magnetic system in laparoscopic surgery can assimilate the third arm of the robotic surgery system. This system gives greater autonomy to the surgeon and correctly exposes the surgical field and makes a correct triangulation of the instruments for the development of single-port or reduced-port bariatric surgery.
Some of the most important benefits we may obtain of single-port or reduced-ports approaches are the reduction of abdominal wall incisions and their related complications.8–10 However, the main drawbacks are the increased difficulty of the surgical technique. In our experience, the use of the magnetic device can be extremely helpful during these approaches. According to our subjective perception it is simple to use the magnet system, it does not increase importantly the surgery time, and the use of magnets and improve the feasibility of new approaches in bariatric surgery; however, all this must be demonstrated with future randomized controlled studies.
Another benefit of single-port or reduced-port approaches, is the aesthetic results from a lower number of scars. Narvaez et al. reports that 77% of bariatric patients believed that the aesthetics of the result is one of the most important factors to take into account.11 One of the problems that can bring the implementation of the single or reduced port approach is the difficulty of the learning curve of this technique, however for the technique of single port laparoscopic cholecystectomy using this magnetic device has been reported in 22nd patient.12 Further studies are needed to evaluate the learning curve of this technique in bariatric surgery.
The limitations of our study include the absence of a control group, the comparison with other retraction methods. Further studies must confirm the benefits of the magnet system uses, in comparison with the standard technique.
In conclusion magnetic assistance in single-port and reduced-port bariatric surgery is an innovative technique. With this prospective study we attempt to demonstrate the safety profile and potential uses that may improve the implementation of new surgical approaches in bariatric surgery.
Ethical approvalAll procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consentInformed consent was obtained from all the participants included in the study.
FundingNone.
Conflict of interestThe authors declare they have no conflict of interest.