Bile duct or choledochal cysts are a rare congenital disease with an incidence that ranges from 1/50000 to 1/2000000 newborns.1 They are more frequent in females and in far Eastern countries, mainly Japan.1–3 Close to 40% of cases are observed after the first decade of life1,3,4 and usually present with abdominal pain, and sometimes with associated jaundice. The finding of an abdominal mass, according to classical descriptions, is more frequent when the disease becomes evident at a paediatric age.1,3,5,6
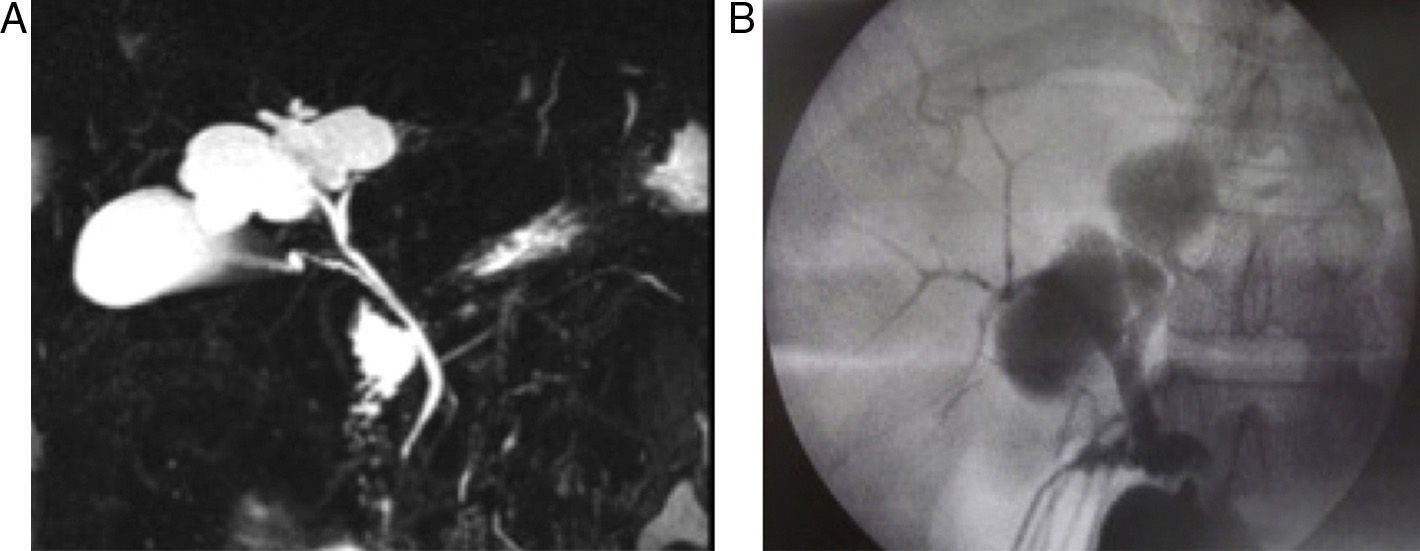
We present the case of a 35-year-old female patient with no medical history of interest that came to our consultation with symptoms of biliary colic without jaundice. Lab work-up showed no alterations. Ultrasound revealed an intrahepatic cystic image measuring 20mm×40mm, with echogenic material in its interior and areas of detritus and lithiasis, located in close contact with the gallbladder in segments 8, 5 and 4b. Magnetic resonance cholangiopancreatography confirmed the existence of a cystic dilatation dependent on the bile duct (Fig. 1A).
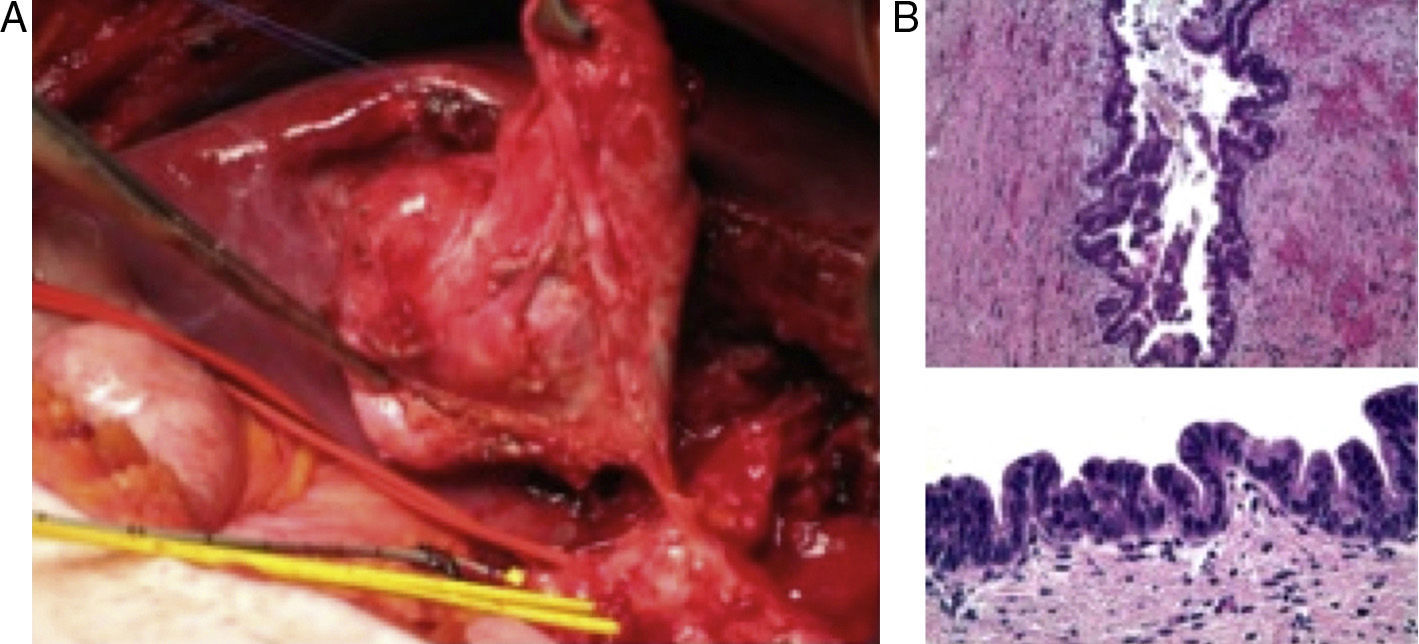
With the diagnosis of Todani7 type v choledochal cyst, the patient was treated by surgery, and intraoperative ultrasound detected cholelithiasis and a cyst with calculi in its interior in segments 8, 5 and 4b. Intraoperative transcystic cholangiography demonstrated a non-dilated bile duct and a filled cyst, without any evidence of continuity with the right or left ducts, which appeared to be separate from the cyst (Fig. 1B). We performed cholecystectomy, hepatotomy and enucleation of the cyst with CUSA®, ligating 2 dependent bile canaliculi of the right and left intrahepatic branches, connected to the cyst (Fig. 2A). The bile duct was checked for leaks by injecting saline through the transcystic catheter. There were no complications during the postoperative period.
Macroscopically, the cyst was 6cm×3cm, multilocular, and had multiple yellowish calculous formations and a greenish liquid in its interior. The microscopic study showed evidence of an epithelium with a biliary phenotype that formed micropapillary projections, covered by cells with hyperchromatic nuclei in a pseudostratified distribution. In some areas, the mentioned papillary projections were larger in size, with vesicular nuclei, and no observed images of stromal invasion (Fig. 2B). The epithelium was immunoreactive for CK7 and negative for CK20. The stroma of the cyst wall was negative for oestrogen and progesterone receptors, which ruled out mucinous cystic neoplasm. The final diagnosis was cyst-forming intraductal papillary neoplasm of the bile duct, BIN II (WHO 2010 classification), with no invasive component.6,8
According to the Alonso–Lej classification as modified by Todani, there are 5 types of bile duct cysts: type i involves dilatation of the extrahepatic bile duct (cystic, segmental or fusiform), type ii choledochal diverticulum, type iii choledochocele, type iv multiple extrahepatic cysts and type v intrahepatic cysts, either single or multiple (Caroli disease).1,2,6,7 Type i is the most frequent.2,7
Close to 80% of the patients affected by this cystic disease develop complications such as lithiasis, pancreatitis, cholangitis, cystic rupture, secondary biliary cirrhosis or malignant degeneration. The gold standard diagnostic test is magnetic resonance cholangiopancreatography. Ultrasound provides the initial suspected diagnosis, since abdominal pain is frequently the only manifestation. Computed tomography is useful for observing signs of malignancy, such as increased cyst wall thickness, intracystic mass or distant disease.1–3,8
Bile duct cysts are considered a premalignant condition as they entail a risk for malignization that is 20–30 times greater than in the general population.4 Some recent series report the existence of a malignant transformation in up to 3% of the cases reviewed. However, according to historical descriptions in the literature by different authors, the risk for malignancy ranges from 4% to 40% of cases.2,3,5 Malignization of these cysts is frequently silent, although they do have prognostic implications. Curative resections are associated with a 5-year survival rate of 25%–50%, while determinant factors for survival include compromised lymph nodes and surgical margin involvement of the neoplastic disease.4
Factors involved in carcinogenesis are chronic inflammation, biliary stasis, the possible development of carcinogenic agents and the reduction of glands in the mucosa of the duct.9 The risk for malignization is greater in types i, iv and in cases with associated biliopancreatic junction anomalies.3 The most frequent histological type is adenocarcinoma, followed by anaplastic carcinoma that is undifferentiated and squamous. In 2010, the WHO modified the classification of biliary cystic neoplasm based on the different grades of cellular atypia.2,6,8
The recommended treatment for bile duct cysts is resection and, in cases that require it, a biliodigestive anastomosis, while selecting the surgical technique according to the cyst type and the existence of any associated malignancy.1,10 Internal drainage of the cystic cavity is not recommended since it is related with the appearance of complications and does not eliminate potential histopathological changes towards malignancy.1 After the definitive treatment, the patient should be followed up in the outpatient setting.1,3
Please cite this article as: Aguilar Martí MD, Montalvá Oron EM, Ballester Pla N, Pérez Rojas J, López Andújar R. Malignización de quiste de colédoco en edad adulta: una entidad poco frecuente. Cir Esp. 2016;94:e41–e43.