The presence of ectopic breast tissue is due to the lack of involution of the primordia of the mammary glands along the “mammary lines”. Its incidence is between 0.6% and 6%,1 and its behavior is similar to normal breast tissue, with the same physiological changes. It may develop either benign or malignant disease, although this is unusual, and the location is mostly axillary.2 For this reason, in the presence of an axillary tumor, the differential diagnosis should include ectopic breast cancer, lipoma, axillary adenopathy, follicular cyst, hidradenitis, fibroadenoma, etc.3
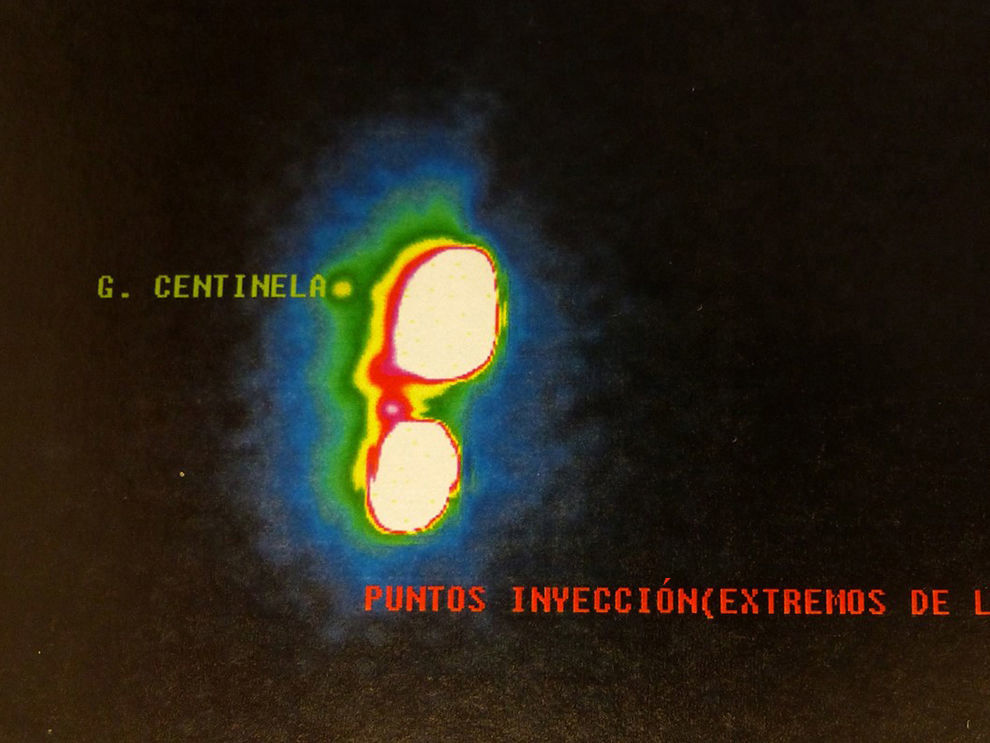
We present the case of a 71-year-old woman diagnosed with infiltrating ductal carcinoma in axillary ectopic breast tissue. She consulted for a self-palpated right axillary nodule. Given the clinical suspicion of a lipoma or adenopathy, the mass was removed surgically, even though no previous imaging or histological study had been performed (Fig. 1). The histopathological study demonstrated an infiltrating ductal carcinoma of mammary origin, grade 2, that was positive for E-cadherin. The immunohistochemical study determined positivity for hormone receptors, HER-2 negative, 3% Ki-67 and positivity for mammaglobin, GCDFP-15 and cytokeratin 19. In the microscopic study, surrounding breast tissue was observed with absence of lymph node structures. It was concluded that the mass was an infiltrating carcinoma in ectopic breast tissue. Imaging tests showed no alterations. Re-resection of the surgical margins was planned with selective sentinel lymph node biopsy (SLNB) and double tagging (isotope and dye) due to the technical difficulty caused by supersaturation in the right axilla (Fig. 2). One sentinel lymph node (SLN) with no metastatic involvement was obtained in the One-Step Nucleic Acid Amplification (OSNA) study. The tumor committee recommended systemic treatment with letrozole. No radiotherapy was used in the breast as the tissue was ectopic mammary tissue and the breast itself showed no alterations.
Breast carcinoma in ectopic tissue poses two difficulties: optimal tagging for SLNB and the need for radiotherapy of the breast. For the former, lymph node staging should apply the same principles as in orthotopic gland carcinoma by means of SLNB in initial stages.4 This technique reduces the morbidity of lymphadenectomy and offers advantages over the surgical approach.5 Lymphoscintigraphy prior to surgery is able to identify the lymphatic regions at risk and is especially useful in extra-axillary drains. Furthermore, it is able to determine the number and location of the SLN within a specific lymphatic area and to identify SLN located between the primary tumor and the usual regional lymphatic drainage area.6 If the location is axillary, the use of radioisotope (technetium-99) may be difficult due to the proximity between the primary tumor and the axillary drainage area. On the other hand, said location has a very predictable lymph node drainage pattern toward the axillary region, therefore the simultaneous use of dye can be quite useful. One question that has yet to be resolved, and for which there is still no consensus in the case of conventional breast cancer,4 is the radiotracer injection site, as there have been reports of peritumoral, intradermal and even periareolar injection.2,7 In a carcinoma over ectopic breast tissue, the optimal site for the injection is the biopsy scar, as it exactly reproduces the lymph drainage of the previous surgical site. This is in contrast with what has been established in orthotopic breast cancer, in which the periareolar or peritumoral pathways have been proposed.7 In addition to tagging, manual exploration of the axilla is recommended, as well as lymphadenectomy if palpable lymphadenopathies are identified or if there is no clear distinction between the axillary ectopic beast tissue and the axillary structures.2
The indication for radiotherapy should be based on prognostic factors and final staging of the process. On this question, no consensus has been established as some authors recommend radiation therapy of the tumor site, axilla and ipsilateral breast; others recommend the tumor site and axilla,6 while some recommend only the tumor site.8 Nonetheless, Patel et al.2 establish that, in cases with extensive excision of ectopic tissue, radiotherapy should only be applied in the presence of positive axillary lymph nodes or other factors for a poor prognosis.2,4 This was the situation of our patient, in whom we decided not to administer radiotherapy and assumed excision of the ectopic gland tissue to be sufficient locoregional treatment as no disease was present (the mass had been removed previously) and the SLNB was negative.
In conclusion, management of breast carcinoma in ectopic breast tissue requires lymph node staging based on SLNB, whose tagging should reproduce the lymph drainage from the original tumor site. The indication of postoperative radiotherapy should be assessed by the Beast Cancer Committee, which should take into account breast imaging studies and lymph node staging pathology results.
FundingThis manuscript has received no funding.
AuthorshipJordina Munrós: manuscript concept and design, data collection, article composition and approval of the final version
Macarena Vázquez, Paz Santiago and Gabriela Romay: data collection and approval of the final version
Benigno Acea: manuscript concept and design, data collection, critical review and approval of the final version
Please cite this article as: Munrós J, Vázquez M, Santiago P, Romay G, Acea B. Tratamiento del carcinoma de mama en tejido mamario ectópico axilar. Cir Esp. 2017;95:232–233.