Choledochal cysts are a rare disease, with an incidence in western countries of 1 in 100 000–150 000 births.1 The rate is considerably higher in Asian populations, where the reported incidence is 1 in 1000 births. The exact etiology is still unknown, although they predominantly affect females with a ratio of 4:1.1 According to the Todani classification, the distribution of the different types of choledochal cysts is: type I 50%–80%; type II 2%; type III 1.4%–4.5%; type IV 15%–35%; type V 20%.1 Mixed type I and II choledochal cysts are extremely rare and represent less than 1.1% of cases. A review of the literature has found only 6 reported cases.2,3 Around 80% present with symptoms before the age of 10. The described symptomatic triad of abdominal pain, jaundice and a palpable abdominal mass occurs in less than 20%.4
The complications of choledochal cysts include bile stasis, the formation of calculi, recurring infections and inflammation. The initial study of these patients involves ultrasound, which is able to establish a diagnosis in most cases. The pancreato-biliary malformations entail a common canal between the junction of the pancreatic duct and the bile duct, which are outside the duodenal wall.5 These malformations are a risk factor for neoplasms of the biliary tract. Pancreatic juices and bile combine constantly, producing toxic substances. Due to this, the mucus of the bile tract is repeatedly damaged and repaired on many occasions, which causes an acceleration of proliferative activity and multiple gene mutations. In turn, this causes histological changes, such as hyperplastic epithelium, metaplastic epithelium, and dysplastic epithelium, which lead to carcinogenesis of the bile duct.6
The frequency of anomalies at the pancreato-biliary junction ranges between 0.08% and 3.2% of the population.7 Kimura defined 2 types of anomalies of the pancreato-biliary junction. In type 1, the pancreatic duct empties into the common bile duct at an acute angle and the distal bile duct does not have stenosis. In type 2 (95%), it is the common bile duct that empties into the pancreatic duct and the distal bile duct usually presents stenosis; therefore, there is greater and earlier dilatation of the bile duct.8 In this article, we report the case of a mixed type I and II choledochal cyst associated with a Kimura type 2 malformation of the pancreato-biliary junction.
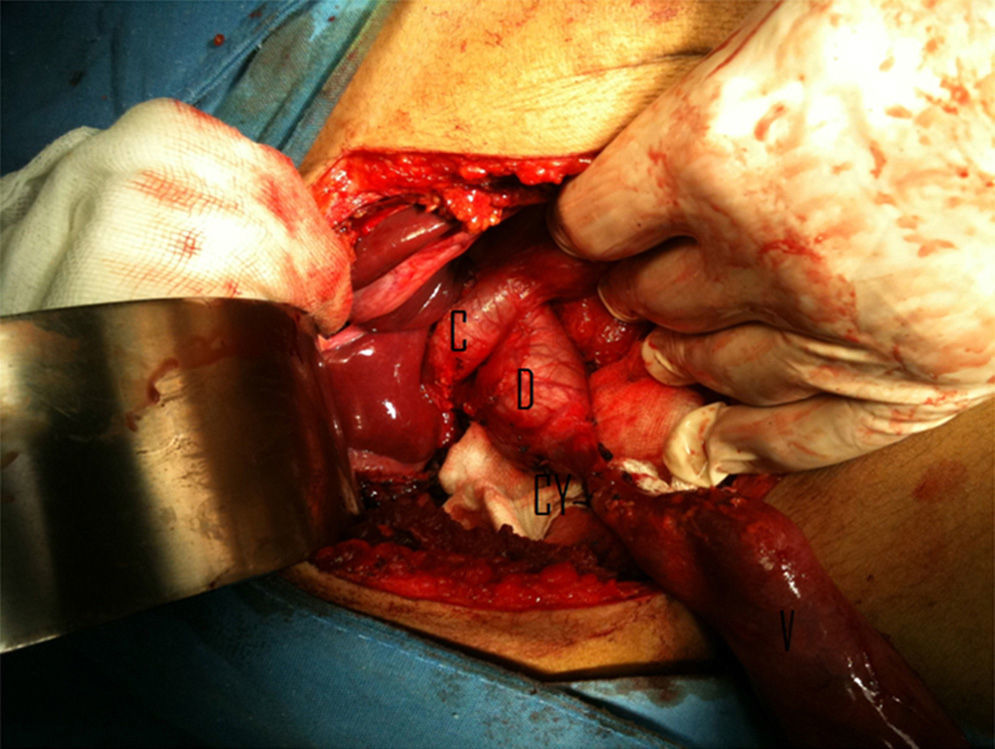
Case ReportThe patient is a 20-year-old male with a history of episodes of acute pancreatitis of undetermined etiology that had been treated in primary care clinics, as well as several episodes of jaundice. He was referred to our unit for study and treatment. Abdominal ultrasound showed evidence of dilatation of the intra- and extrahepatic bile duct, a choledochal cyst and pancreas with inflammation. Abdominal tomography showed dilatation of the intra- and extrahepatic bile duct up to the ampullary region. Surgical findings were: a gallbladder measuring 8×4×2cm, which drained through the cystic duct to a diverticulum measuring 2×2×1cm of the common bile duct, which was dilated to 2.5cm, approximately (Fig. 1). Transcystic cholangiography was performed, and a dilated type II choledochal cyst was observed. We proceeded with diverticulectomy/cholecystectomy, choledochorrhaphy and Kehr tube placement. The histopathology study reported a gallbladder measuring 7×3×1cm, with a 3mm wall and hemorrhagic-looking mucosa, drainage of the cystic duct to a cystic lesion measuring 2×1×1cm with irregular outer surface and thickened walls.
During post-op, there was a high level of bile discharge through the Kehr tube of up to 2100cc in 24h. Cytology was ordered of the bile liquid, which reported 183,654IU amylase and 159.617IU lipase. Cholangiography was performed through the Kehr tube, and a common bile duct of 18mm was observed as well as pancreato-biliary malformation (Fig. 2). There was no evidence of residual calculi and adequate passage of contrast medium to the duodenum was observed. We therefore decided to close the Kehr tube and scheduled an endoscopic retrograde cholangiopancreatography (ERCP) and sphincterotomy in order to reduce pancreato-biliary reflux, both of which were done without incident. Cytology of the bile liquid showed that the pancreatic enzymes had doubled over the previous analysis, so the diagnosis of pancreato-biliary reflux was established. We decided to perform exeresis of the main bile duct with Roux-en-Y hepaticojejunal anastomosis, with findings of type I choledochal cyst. The histopathology study reported a common bile duct measuring 3.5×2.5cm, follicular lymphoid hyperplasia and no evidence of malignant cells. The patient presented an uneventful recovery and, 12 months after surgery, has had no new episodes of pancreatitis or jaundice.
In a review of 356 patients over a period of 40 years, Kaneyama reported 4 cases in children who presented dilatation of the main bile duct with the presence of a diverticulum in the middle third of the duct, and the gallbladder drained by means of a cystic duct directly to the diverticulum.2 In 2003, Katsinelos reported a similar case of a mixed type I and II cyst with pancreato-biliary junction malformation in a 72-year-old woman that had begun with an episode of pancreatitis. The patient was managed conservatively with endoscopic cholangiopancreatography and sphincterotomy.3 In our case, we opted to perform cholecystectomy and resection of the diverticulum with Kehr tube placement; afterwards, we performed an endoscopic cholangiopancreatography study with extensive sphincterotomy, which showed evidence of a long pancreato-biliary common duct measuring 24.5mm (normal range 4.6±2.6mm).9 With these criteria, we established the diagnosis of pancreatic reflux. In our case, there was evidence of that the sphincterotomy did not diminish the pancreato-biliary reflux. Given the evidence of pancreato-biliary malformation associated with dilatation of less than 20mm, complete exeresis of the bile duct was indicated.
Congenital pancreato-biliary malformations have a risk of malignization of 10%–30%, which is 20–30 times more frequent than in the general population.10 In these cases, it is essential to utilize precise imaging techniques and to evaluate the risk–benefit of preoperative ERCP to document pancreato-biliary malformations.
Please cite this article as: Raful Zacarías-Ezzat J, Ramos-Cruz I, Palafox-Vidal D, Chapa-Azuela Ó, Etchegaray-Dondé A. Quiste de colédoco mixto (tipo I y II) asociado a malformación de la unión pancreatobiliar. Reporte de un caso y revisión de la literatura. Cir Esp. 2015;93:346–348.
This paper was presented at the 10th Congress of the International Hepato-Pancreato-Biliary Association in Paris, France from July 1–5, 2012.