According to the latest WHO tumor classification,1 mucinous cystic neoplasms (MCN) of the gallbladder are defined as epithelial cystic neoplasms composed of cells which contain intracytoplasmic mucin. Traditionally, it is also known as mucinous cystadenoma (or cystadenocarcinoma when associated with an invasive carcinoma) and it shares many histologic similarities with other neoplasms with the same name located in the pancreas or in the intra- or extrahepatic bile duct. They are extremely rare.
We present the case of a 75-year-old woman with no prior medical history of interest. During studies for abdominal pain and obstructive jaundice, an ultrasound image was seen of a cyst in the hepatic hilum, associated with choledocholithiasis.
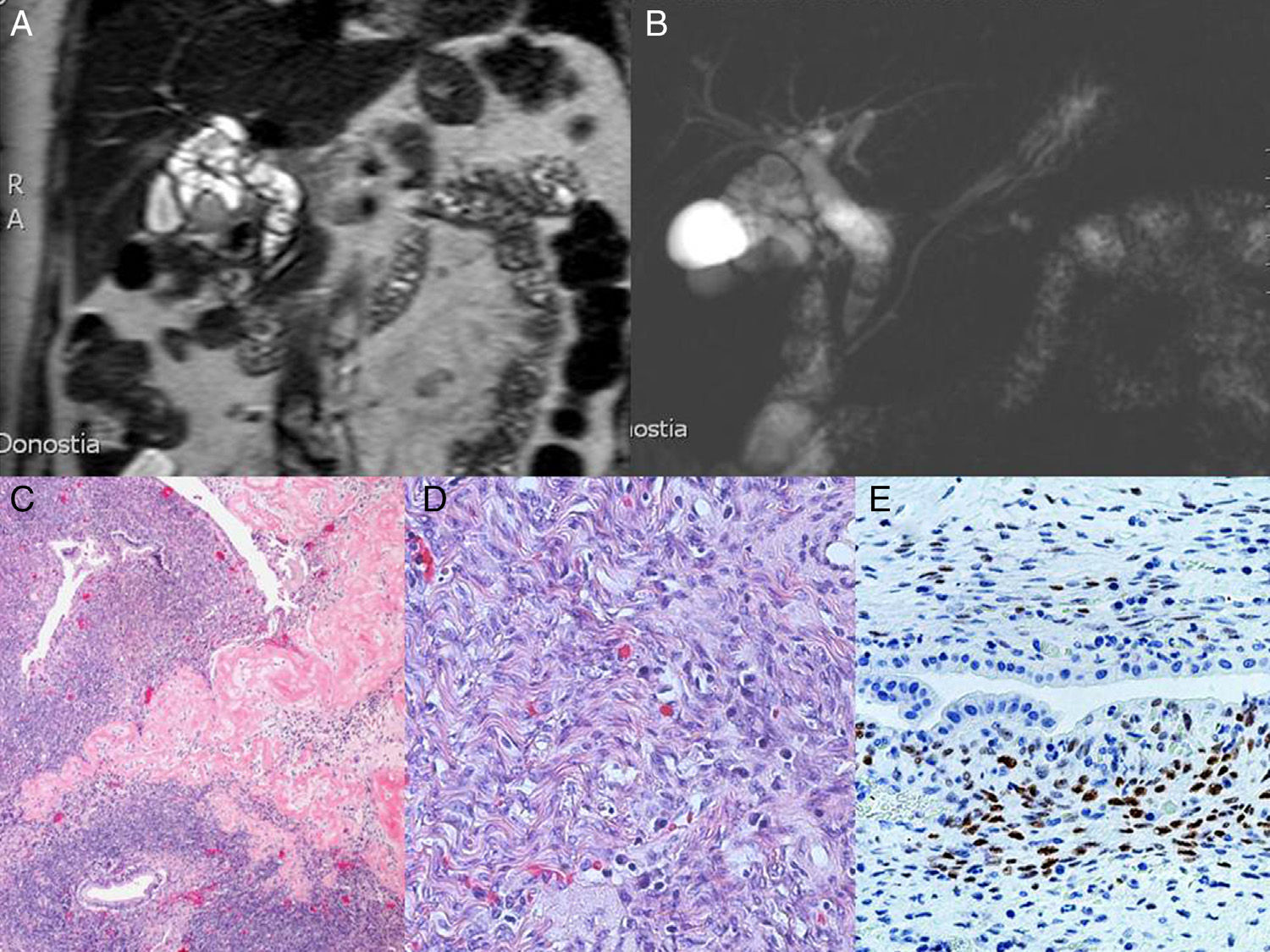
Magnetic resonance cholangiography revealed a multiseptated cystic mass in the region of the hepatic hilum (Fig. 1A and B), in addition to mild dilatation of the intra- and extrahepatic bile duct with a filling defect in the common bile duct, suggestive of choledocholithiasis. Serology for hydatid cyst was negative.
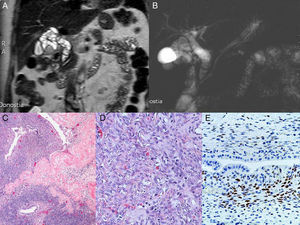
(A and B) MRI prior to surgery; (C) hyalinized structure that histologically similar to corpus albicans. The stroma is hypercellular and contains bile-type duct structures, hematoxylin eosin (HE ×10); (D) detail of the stroma composed of fusiform, wavy ovarian-like cells (“ovarian-like stroma”) and occasional lymphocytes and plasma cells. No mitosis is observed (hematoxylin-eosin stain, HE ×40); (E) immunoreactivity of the stromal cells versus estrogen receptors (RE+).
CPRE confirmed the dilatation of the bile duct, and a calculus was extracted. No other obstructive cause was found in the bile duct. As no malignancy was suspected, the patient's evolution was followed-up in the outpatient consultation.
After a couple of asymptomatic months, the patient presented a new episode of obstructive jaundice with no radiological changes in the previously described cystic tumor formation. Another CPRE confirmed the existence of another calculus in the bile duct, which was extracted.
Given the recurring symptoms and the lack of a definitive diagnosis, the patient was scheduled for surgery. Using laparotomy, we located a solid-cystic polypoid gallbladder mass with a small implantation base in Hartmann's pouch that occupied the entire lumen of the cystic duct and prolapsed toward the common bile duct. Cholecystectomy and choledochoscopy were performed; dilatation of the bile duct was observed with no other findings. The intraoperative study of the tumor formation was negative for malignancy, at which point the intervention concluded.
The postoperative period ran its course with no notable incidences. A postoperative magnetic resonance cholangiography showed complete resection of the cystic tumor formation.
The definitive pathology results reported a normal gallbladder with an implanted lesion compatible with mucinous cystic neoplasm (Fig. 1C–E), and therefore the patient received no further additional treatment.
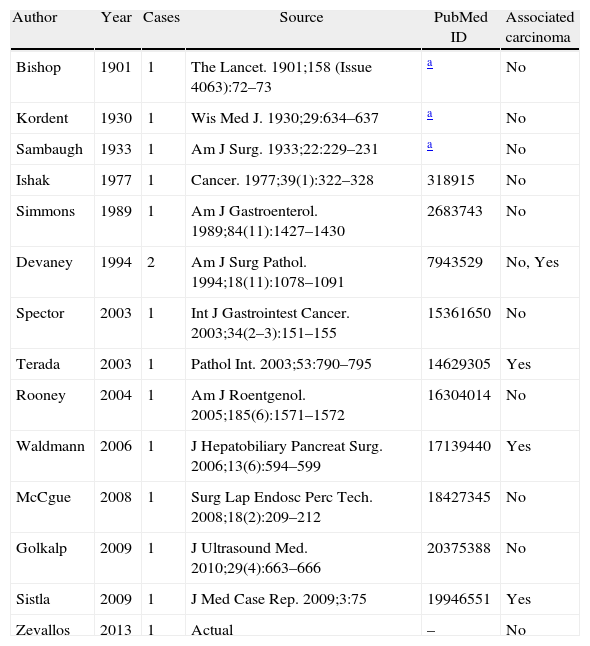
We performed a search of the available scientific literature on Pubmed using chain searches of the references found. Most likely, the first case published of this disease was by Bishop et al. in The Lancet in 1901 under the title “An undescribed innocent growth of the gallbladder”.2 Since then, only 13 cases of this condition have been published in the literature.
We collected information of the 13 cases published, and together with ours we have created a series that can help to better understand this disease (Table 1).
List of Published Cases of Mucinous Cystic Neoplasms of the Gallbladder.
| Author | Year | Cases | Source | PubMed ID | Associated carcinoma |
| Bishop | 1901 | 1 | The Lancet. 1901;158 (Issue 4063):72–73 | a | No |
| Kordent | 1930 | 1 | Wis Med J. 1930;29:634–637 | a | No |
| Sambaugh | 1933 | 1 | Am J Surg. 1933;22:229–231 | a | No |
| Ishak | 1977 | 1 | Cancer. 1977;39(1):322–328 | 318915 | No |
| Simmons | 1989 | 1 | Am J Gastroenterol. 1989;84(11):1427–1430 | 2683743 | No |
| Devaney | 1994 | 2 | Am J Surg Pathol. 1994;18(11):1078–1091 | 7943529 | No, Yes |
| Spector | 2003 | 1 | Int J Gastrointest Cancer. 2003;34(2–3):151–155 | 15361650 | No |
| Terada | 2003 | 1 | Pathol Int. 2003;53:790–795 | 14629305 | Yes |
| Rooney | 2004 | 1 | Am J Roentgenol. 2005;185(6):1571–1572 | 16304014 | No |
| Waldmann | 2006 | 1 | J Hepatobiliary Pancreat Surg. 2006;13(6):594–599 | 17139440 | Yes |
| McCgue | 2008 | 1 | Surg Lap Endosc Perc Tech. 2008;18(2):209–212 | 18427345 | No |
| Golkalp | 2009 | 1 | J Ultrasound Med. 2010;29(4):663–666 | 20375388 | No |
| Sistla | 2009 | 1 | J Med Case Rep. 2009;3:75 | 19946551 | Yes |
| Zevallos | 2013 | 1 | Actual | – | No |
This series includes 12 women (86%) and 2 men (14%). Only 4 cases had mucinous cystic neoplasms associated with an invasive carcinoma, which is 28%, but the 2 men of the series both had invasive carcinoma.
The data concur with those from the largest series of cases published of mucinous cystic neoplasms of the gallbladder: 70 cases of neoplasms situated in the gallbladder and in the intra- and extrahepatic bile duct published by Devaney et al.3 They found that when there was no associated carcinoma, 96% of the cases were women; however, in cases where there was invasive carcinoma, no association is observed with the female sex.
It should be highlighted that in the literature 2 histologic types have been reported. One is not very aggressive and has an epithelial stroma similar to ovarian stroma and is immunoreactive for estrogen and progesterone receptors. This subtype affects middle-age women. The second subtype is more aggressive, without the ovarian-like mesenchymal stroma, and it affects senior males4 (in our review, the 2 males were 75 and 88 years old, respectively).
When there was no associated invasive carcinoma, the symptoms depended on the degree of bile duct obstruction and they were almost always associated with cholelithiasis or choledocholithiasis. On the other hand, in cases that did present this association, the main symptom was abdominal pain and, in one case, a palpable mass in the upper right abdomen.4–6
Cystic lesions originating in the gallbladder fossa may be dependent upon the lower surface of the liver or gallbladder. In addition, hepatic lesions such as simple cysts, hydatid cysts or abscesses are more frequent than lesions located in the gallbladder. This is why a detailed clinical history, meticulous physical examination and multiple imaging tests are so important to determine the location and characteristics of the lesion (echogenicity and blood flow on Doppler ultrasound, densities on tomography and intensity variations on magnetic resonance cholangiography). Cystic lesions originating in the gallbladder can include hydatid cysts, lymphangiomas and epithelial cysts in association with gallbladder adenocarcinoma or mucinous cystic neoplasm. It is also recommended to always order a complete work-up with cholestasis tests, liver function, acute phase reactants and serology for hydatid cyst. If there are symptoms of cholestasis, an endoscopic retrograde cholangiopancreatography or percutaneous transhepatic cholangiography should be done to assess the degree of obstruction in the bile duct.
There have been descriptions of the use of ultrasound-guided fine-needle aspiration to try to take samples from irregular areas, but cytologies have not been useful for ruling out malignancy given the poor cellularity of cystic lesions.4
In all cases, cholecystectomy should be performed with an intraoperative study to rule out malignancy. The definitive diagnosis is made after the resection of the tumor with the pathology study.
In cases with no malignant disease, cholecystectomy has been shown to be curative,7–10 even for cases of mucinous cystic neoplasm in which there are only nests of malignant cells in a mass with a predominance of non-invasive component.5 The most aggressive surgeries with liver segmentectomy or multi-organ resection are reserved for cases of invasive carcinoma when local dissemination of the disease is observed, as in the case reported by Waldmann et al.6 In no case was any adjuvant treatment given.
Please cite this article as: Zevallos Quiroz JC, Jiménez Agüero R, Garmendi Irizar M, Ruiz Montesinos I, Comba Miranda JW. Neoplasia mucinosa quística de vesícula biliar con obstrucción intraluminal de colédoco, una entidad rara con un nuevo nombre. Cir Esp. 2014;92:567–569.