Frailty is associated with greater postoperative morbidity and mortality. Individualized multidisciplinary management of these patients can improve the quality of care. The objectives of this study are to determine the percentage of frail patients with colorectal cancer in our population, and to describe the morbidity and mortality associated with surgery and the evolution of palliative treatment.
MethodsA prospective, observational study of patients with surgical colorectal cancer (February 1, 2018–April 30, 2019). Frail patients were screened and classified according to degrees of frailty. Therapeutic decision-making (surgery or palliative treatment) was determined by the degree of fragility and explicit will of the patient. Postoperative comorbidities were analyzed (according to Clavien–Dindo and Comprehensive Complication Index), as were mortality and oncological follow-up.
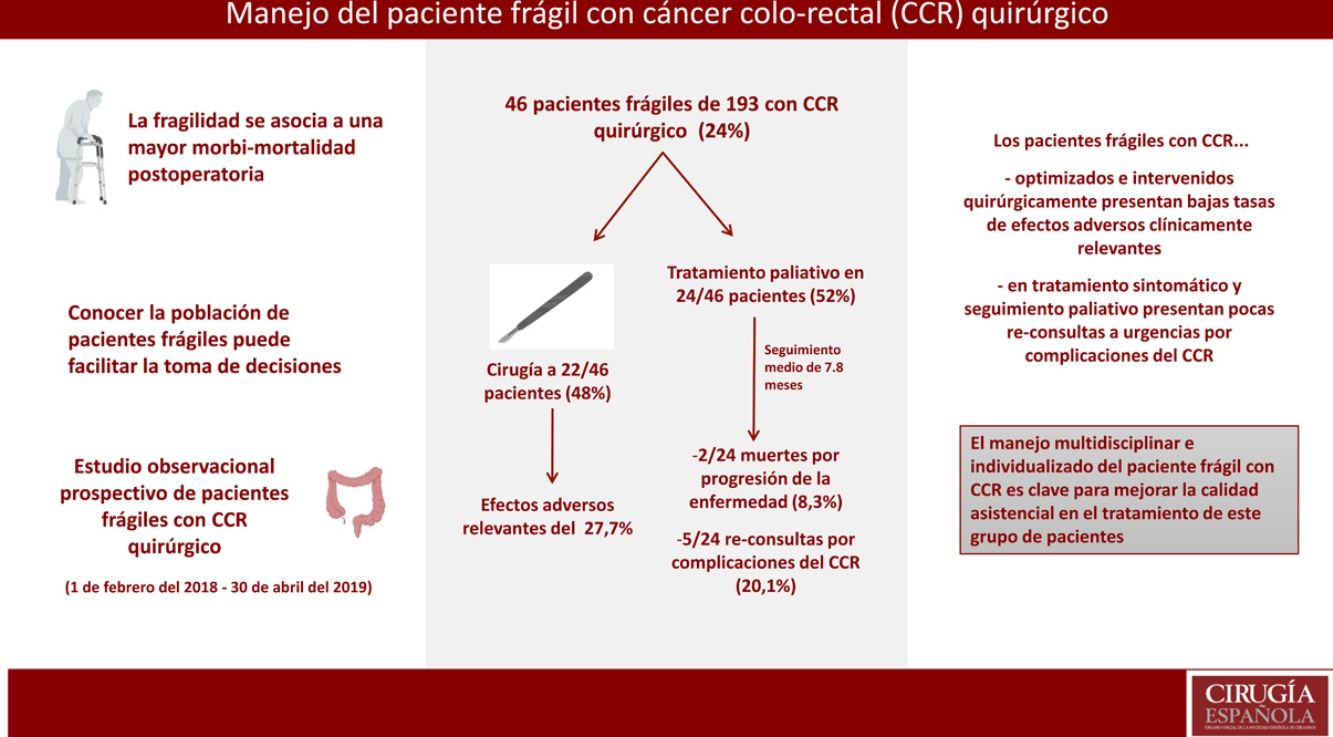
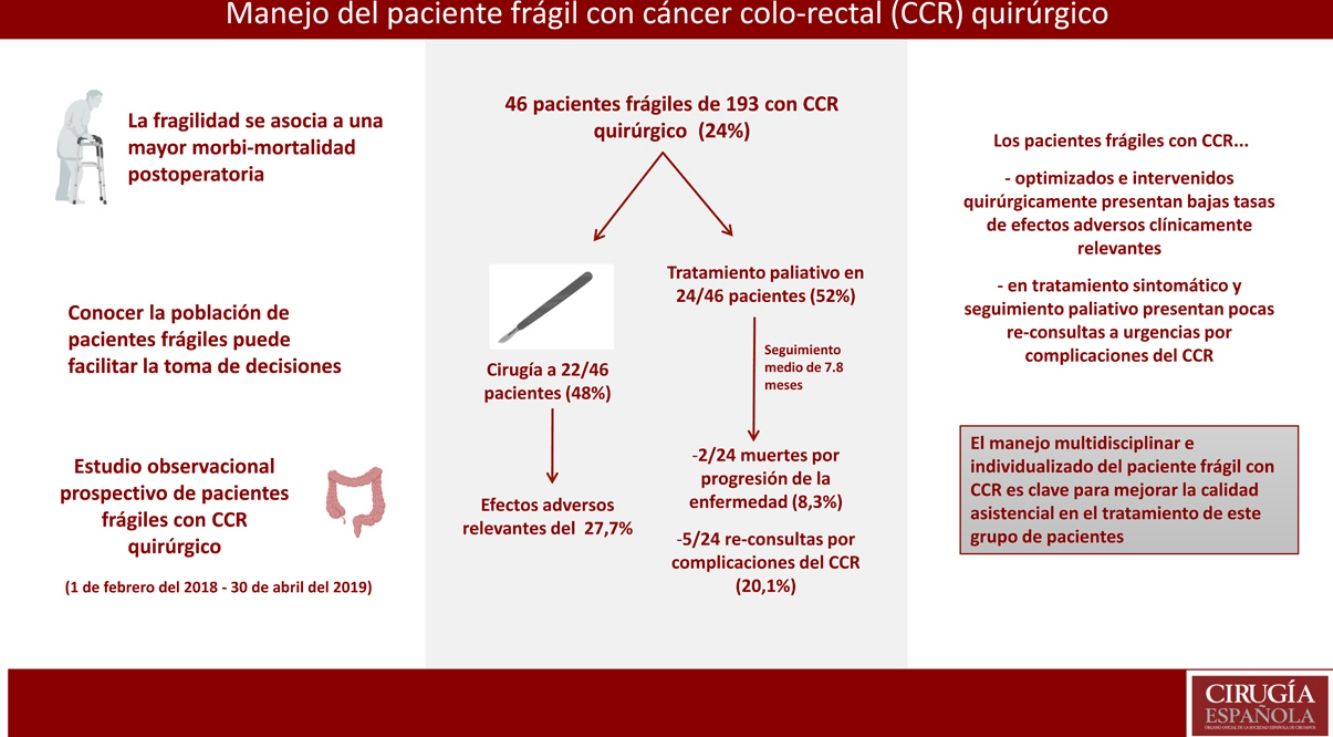
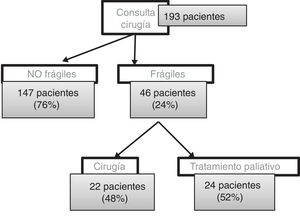
ResultsThe study included 193 patients with surgical colorectal cancer, with a mean age of 74 years (44–92). Screening identified 46 frail patients (24%), with a mean age of 80 years (57–92). Twenty-two patients were optimized and underwent surgery (48%), with a mean age of 78 years (57–89). Relevant adverse effect rate was 27.7% (4 grade iva adverse effects, one IVb and one V, according to Clavien–Dindo). Comprehensive Complication Index was 17.5. Palliative treatment was administered in 24 patients (52%), with a mean age of 82 years (59–92). Mean follow-up was 7.8 months. There were 2 deaths due to disease progression (8.3%), 5 re-consultations due to complications of colorectal cancer (20.1%).
ConclusionsThe multidisciplinary and individualized management of frail patients with colorectal cancer is key to improve the quality of care in the treatment of this patient group.
La fragilidad se asocia con una mayor morbimortalidad postoperatoria. El manejo multidisciplinar individualizado de estos pacientes puede mejorar la calidad asistencial. Los objetivos de este trabajo son conocer el porcentaje de pacientes frágiles con cáncer colorrectal en nuestra población y describir la morbimortalidad asociada a la cirugía y la evolución del tratamiento paliativo.
MétodosEstudio observacional prospectivo de pacientes con cáncer colorrectal quirúrgico (1 de febrero del 2018-30 de abril del 2019). Cribado de paciente frágil y clasificación según grados de fragilidad. Decisión terapéutica (cirugía o tratamiento paliativo) según grado de fragilidad y voluntades explícitas del paciente. Análisis de comorbilidad postoperatoria (según Clavien-Dindo y Comprehensive Complication Index), mortalidad y seguimiento oncológico.
ResultadosFueron visitados 193 pacientes con cáncer colorrectal quirúrgico, con una edad media de 74 años (44-92). Cribado: 46 pacientes frágiles (24%), con una edad media de 80 años (57-92). Se optimizó e intervino a 22 pacientes (48%), con una edad media de 78 años (57-89). Efectos adversos relevantes del 27,7% (4 efectos adversos grado iva, uno ivb y otro v, según Clavien-Dindo). Comprehensive Complication Index de 17,5. Tratamiento paliativo en 24 pacientes (52%), con una edad media de 82 años (59-92). Seguimiento medio de 7,8 meses, 2 muertes por progresión de la enfermedad (8,3%), 5 reconsultas por complicaciones del cáncer colorrectal (20,1%).
ConclusionesEl manejo multidisciplinar e individualizado del paciente frágil con cáncer colorrectal es clave para mejorar la calidad asistencial en el tratamiento de este grupo de pacientes.
According to the published literature, 23%–25% of patients with colorectal cancer (CRC) are considered frail.1 Frailty is defined as a clinical syndrome that involves a progressive loss of physiological reserve.2 This loss generates individual vulnerability and a disproportionate decompensation to stressors, such as surgery, which may lead to increased adverse postoperative effects, longer hospital stays and increased mortality.3,4
Regardless of age, frailty in patients with CRC undergoing surgery has been associated with greater postoperative morbidity5 and mortality, both in the short term6,7 and 5 years after surgery.8
Preoperative detection of frail patients is important because it enables us to anticipate, and therefore prevent, potential complications.5 For example, physical exercise, nutritional interventions, or stabilizing decompensated chronic diseases can be encouraged and promoted.9 We may also opt for minimally invasive surgeries or less intensive operations in order to preserve patient quality of life.7
Another important point regarding these patients is their involvement in decision-making.10 Respect for the patient's priorities has been associated with a decrease in hospital stays and readmissions.7
To date, only one prospective randomized study has compared the postoperative results of frail patients with CRC based on whether or not they had received preoperative geriatric care. Although the authors did not find significant differences in the incidence of grade II–V complications, re-operations, repeat consultations or mortality, the group with directed care presented a lower number of serious complications, mainly medical.11
Given these data, individualized therapeutic approaches should be adopted when treating patients who meet frailty criteria, thereby avoiding disproportionate diagnostic and therapeutic measures as well as the underuse of therapeutic measures with proven efficacy.12 However, this can be difficult and generate conflict among medical professionals, and even with patients and family members.
With the aim to facilitate the management of frail patients with CRC or high surgical risk and to improve the quality of care in this group of patients, a multidisciplinary action protocol was designed. Our main objective was to determine what percentage of patients with CRC in our series could be considered frail and/or multipathological.
We also intended to: (1) estimate the risk of postoperative morbidity and mortality preoperatively; (2) modify the management of patients with CRC based on the potential risk of morbidity and mortality and the explicit preferences of the patient; (3) follow measures to medically optimize frail patients in the preoperative period; (4) determine the results in terms of morbidity and mortality of patients in whom curative surgery is decided; and (5) monitor patients with CRC who had opted for palliative treatment.
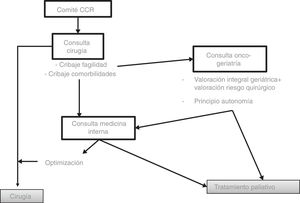
MethodsWe designed a prospective observational study of patients diagnosed with CRC consecutively at a hospital with about 450 acute-care beds. The CRC cases were presented to a multidisciplinary hospital committee, where treatment was decided according to the recommendations of the National Comprehensive Cancer Network13 (Fig. 1).
If surgery was indicated, the patient was evaluated by one of the members of the Coloproctological Surgery Unit. During this consultation, frail patient screening was conducted with the validated PRISMA-7 questionnaire.14 Patients with 3 or more positive items were considered frail and were referred to the frail cancer patient consultation. Patients with less than 3 positive items followed standard CRC patient management.
Frail cancer patients were subsequently seen by a geriatric specialist. At this office visit, a comprehensive geriatric assessment was performed with the validated IF-VIG questionnaire.15 In addition, patients and family members were informed of the different treatment alternatives (including the possibilities of palliative care and symptomatic treatment). The management was individualized, based on the result of the IF-VIG and the explicit wishes of each patient.
All frail patients with CRC in whom surgery was indicated were referred for consultation with an internist. Efforts were made to stabilize possible underlying diseases, and recommendations were given for healthy lifestyle habits. When the patient was correctly optimized or could become so, optimization measures were applied and the surgical preparation circuit was followed. Otherwise, palliative treatment was chosen.
Inclusion criteria were: patients with CRC who were candidates for surgery, and a positive PRISMA-7 form for frailty. Exclusion criteria were: minors, negative PRISMA-7 form, or patients who did not wish to enter the study.
We collected data for demographic characteristics, medical-surgical history, PRISMA-7 items and results, IF-VIG forms and PROFUND comorbidity index,16 therapeutic option, patient wishes and post-treatment results of all participants. The data were collected consecutively and prospectively in an Access database with a protected format.
We also analyzed comorbidities associated with the treatment performed, defined as adverse effects according to the Clavien–Dindo classification17 and the Comprehensive Complication Index18 (30 days after the intervention), as well as mortality and oncological results.
Data processing and analysis were carried out with the IBM 21 SPSS statistical data editor. Quantitative variables are expressed as mean and standard deviation, while categorical variables are described in absolute numbers and percentages.
To estimate the population size necessary for the analysis in order to determine the actual percentage of frail patients, we estimated the proportion to be around 45%, with an alpha value of 0.05 and a maximum error of 10%. Under these conditions, a minimum general population of 96 patients was necessary.
The project was approved by the ethics committee of the Institut d’Investigació i Innovació Parc Taulí, with reference number 2017644.
The STROBE indications for observational studies were also followed for article design and writing.
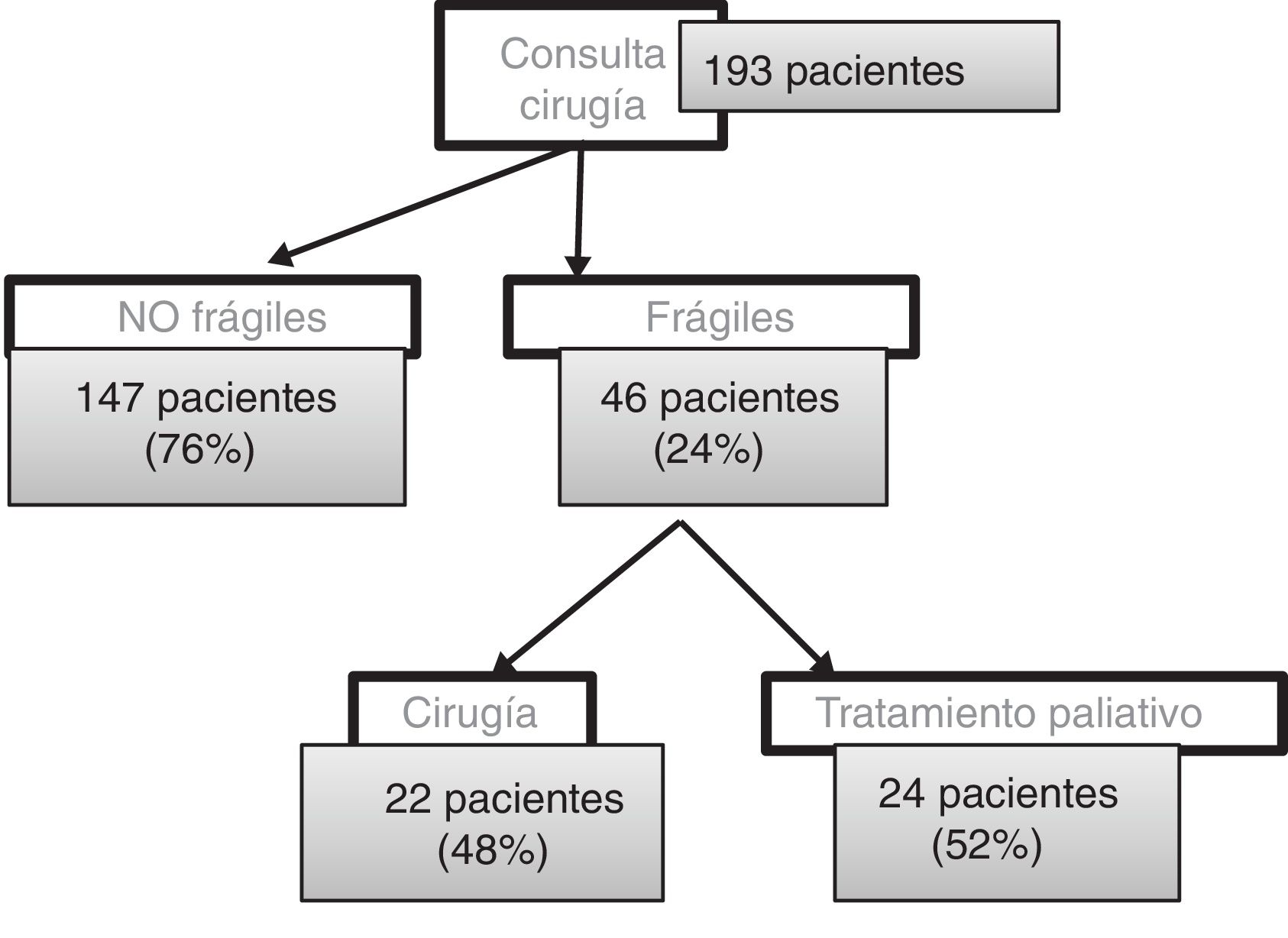
ResultsBetween February 1, 2018 and April 30, 2019, we had consultations with 193 patients (85 women and 108 men) with an average age of 74 years. Out of these, 147 patients (76%) submitted a negative frailty questionnaire and followed the usual protocol. Forty-six patients (24%) presented a positive PRISMA-7: 19 women and 27 men, with a mean age of 80 years (57–92). The average IF-VIG was 0.35 (upper limit of mild frailty) (Fig. 2).
From this total, we have operated on 22 patients (48%), 8 women and 14 men, with a mean age of 78 years (57–89). The average IF-VIG score was 0.22 (mild frailty), distributed in 16 patients with mild frailty and 6 with moderate frailty. We have not operated on any patient with severe frailty. The average waiting time between the first office visit in outpatient surgery and the surgical procedure was 70 days (20–147).
Six adverse effects higher than grade II have been collected according to the Clavien–Dindo classification17 (27.7%): 4 grades IVa, one grade IVb and one grade V. Four of these were concentrated in the same patient: an 81-year-old woman with moderate frailty (IF-VIG 0.36), who presented an intraoperative intestinal perforation that went unnoticed and required reoperation and admission to the critical care unit, leading to her death. The organ-cavity infection rate was 13.6% (3 out of 22 patients), with a nosocomial infection rate of 22.7% (5 out of 22 patients). The mean Comprehensive Complication Index18 was 17.57. The mean Comprehensive Complication Index of the patients who presented clinically relevant complications was 29.7.
Palliative treatment was applied in 24 patients (52%; 11 women and 13 men) with a mean age of 82 years (59–92). The mean IF-VIG was 0.46 (moderate frailty), distributed in 6 patients with mild frailty, 8 with moderate frailty and 10 with severe frailty.
With a mean follow-up of 7.8 months (2–14), 5 deaths have been recorded (20.1%). Four of these patients had moderate frailty and one mild frailty. Two patients presented respiratory failure secondary to superinfection that led to death, and one patient underwent surgery for a femur fracture, followed by a complicated postoperative period that led to death.
Only 2 patient deaths (8.3%) were due to complications secondary to the progression of the disease, one of whom presented mild frailty.
In this follow-up period, 8 patients (45.8%) have had 11 ER re-consultations, 5 of which (20.1%) were due to symptoms associated with CRC.
DiscussionFrail patients have a higher risk of postoperative complications and/or death and, therefore, require individualized therapeutic approaches.12
Comprehensive geriatric assessment is the gold standard for assessing frailty, although the need for specifically trained personnel and the time required make it difficult to use outside geriatric units.15 There are also different frailty screening tools that allow us to measure the degree of vulnerability of each patient.15,19 Among these, we chose the PRISMA-714 because it rapidly detects frail patients with high sensitivity and is validated for patients in the outpatient setting. Our series found that 24% of patients with CRC were frail, which is a value very similar to previously published series.
In the Geriatrics consultation, all frail patients are assessed using IF-VIG, a frailty index based on comprehensive geriatric assessment that is a simple validated tool, with discriminative capacity and a high correlation with mortality.15 A prospective longitudinal observational study published in 2017, which analyzed the prognostic capacity of IF-VIG, concluded that there is a greater correlation between IF-VIG and mortality than between age and mortality. This correlation can help us optimize the use of resources by stratifying patients. Thus, in individuals with advanced frailty and, therefore, a high risk of death, well-being should be prioritized through symptomatic control.
The same authors of the article believe that the IF-VIG is only a guide, and that it is necessary to respect the explicit wishes of the patient. Therefore, although initially our intention was to only operate on patients with mild frailty and to apply palliative treatment in patients with moderate and severe frailty, in the end we operated on 6 patients with moderate frailty, while palliative treatment was applied in 6 patients with mild frailty, respecting the express wishes of the patients.
Originally, the PROFUND questionnaire was used as a comorbidity screening tool in all frail patients for whom surgery was decided, and only patients with a positive questionnaire were seen in Internal Medicine consultations. This score is able to predict one-year mortality in pluripathological patients.16 Over the course of time, we decided that all frail patients with indication for surgery should be evaluated by internists. This has allowed for these patients to be optimized. In most cases, it is only necessary to reinforce healthy lifestyle habits, such as physical exercise and diet. Only a few cases require modifications to medication or an evaluation by other specialists. The internist also offers postoperative support for these patients.
Frail patients with CRC who underwent surgery presented low rates of clinically relevant adverse effects and organ-cavity and nosocomial infection rates within acceptable values.20 Despite being complex patients in whom greater postoperative morbidity and mortality could be expected, they are highly selected patients (we have not operated on the frailest patients), optimized in the preoperative period. In addition, they receive medical support in the immediate postoperative period, which provides satisfactory results.
Despite the fact that, in previous studies, the preoperative optimization of frail patients undergoing CRC surgery has not demonstrated a decrease in clinically relevant complications, reoperations and death,11 the complications presented are generally of low severity and clinical relevance. In fact, the complications that led to the death of one of the patients with moderate frailty were surgical complications that can occur regardless of the patient's frailty. Regardless, we would like to emphasize that this case highlights the low functional reserve of frail patients, which causes a lower capacity to respond to aggressors, making complications in this group of patients clinically more relevant than in other patients with CRC.
In the study period reported, we have rejected surgery in 24 frail patients, with follow-up results that are also better than could be expected. We would like to emphasize that these patients are complex and have underlying comorbidities. They could be expected to have complicated postoperative recoveries, with prolonged hospitalizations and high morbidity and mortality; however, unlike what may be expected, they have few ER repeat consultations. We believe that the symptomatic treatment of these patients and their palliative follow-up lead to a surprisingly low number of emergency department consultations for complications. In fact, only 5 patients (20.1%) re-consulted for symptoms associated with CRC. Mortality in this group of patients is also expected. Most deaths were of patients with advanced frailty, who have, according to the IF-VIG, a one-year probability of death close to 100%. Only 2 deaths (8.3%) were due to progression of the disease.
Therefore, we believe that there is a group of patients in whom a cure should not be our main objective. Rather, we should focus our therapeutic effort on maintaining quality of life and symptomatic control.
Finally, we would like to highlight that our series also includes frail patients under the age of 60 as well as elderly patients with a negative frailty screening test. This supports the theory that chronological age is not a good indicator in decision-making about the medical–surgical management of patients.
We are aware of the low statistical weight provided by an observational study. Nevertheless, we are so convinced of the need to apply a frail patient management protocol that patient randomization did not seem ethical to us. For this reason, we preferred to provide a detailed description of the outcomes of these patients in our series.
For the calculation of the sample, an estimated proportion of around 45% was used, with an alpha value of 0.05 and a maximum error of 10%. An estimated proportion of 45% was used, which was the expected proportion of frailty in the patients with CRC in our population, with a lack of a clear bibliographic reference. Under these conditions, it was necessary to analyze a minimum general population of 96 patients. We understand that the maximum accepted error is high, but our intention was to know roughly the proportion of frailty in our population. Our percentage of frail patients was 23.83% (coinciding with recent publications1) with a confidence interval of 18%–30.5%—wide, but sufficient to provide an initial estimate of the general situation. In any event, in the future we intend to expand data collection to a larger population in order to reach greater statistical power and establish a predictive model of mortality in frail patients with CRC patients treated with surgery.
Another possible criticism of the protocol is the delay of surgery in frail patients. On average, the surgery was 70 days after the first visit to the outpatient consultation (range: 20–147 days). While it is true that the extra office visits for frail patients lengthen the waiting time, we believe that this is essential for correct patient selection and optimization. Additionally, the 70-day average includes patients who have explicitly requested more time to make a final decision.
With these results, we believe that multidisciplinary and individualized management of frail patients with CRC is key to improving the quality of care in the treatment of this group of patients.
AuthorshipS. Serra-Pla has carried out the study design, data analysis and has collaborated with the design of the Access database in a protected format and with data collection. A. Pallisera-Lloveras has collaborated with data collection. L. Mora-López has collaborated with study design and data collection. A. Granados Maturano has carried out the medical management of the patients and has collaborated with data collection. S. Gallardo was responsible for the oncogeriatric management of the patients, the analysis of their degree of frailty, and has collaborated with the data collection. C. del Pino Zurita has collaborated in patient management. J. Serra-Aracil has collaborated in the design of the study and in the collection and analysis of data.
Conflict of InterestsNone of the authors have conflict of interests to declare.
The authors would like to thank Francesc Rodríguez Arenas for his help with the design of the Access database. Thanks also go to the entire colorectal surgery team for their participation and interest in maintaining the protocol.
Please cite this article as: Serra-Pla S, Pallisera-Lloveras A, Mora-López L, Granados Maturano A, Gallardo S, del Pino Zurita C, et al. Manejo multidisciplinar y optimización del paciente oncofrágil o de elevado riesgo quirúrgico en cirugía del cáncer colorrectal. Análisis observacional prospectivo. Cir Esp. 2020;98:389–394.