Surgical treatment of hilar cholangiocarcinoma includes the reconstruction of the bile duct by means of hepaticojejunostomy. In cases with tumor recurrence in the region of the anastomosis, surgical treatment is not usually curative. The only feasible option is palliation, which includes CT-guided percutaneous placement of stents to improve cholestasis and prevent or treat cholangitis.1–3
Occasionally, the tumor recurrence can obstruct the afferent jejunal loop, whose end acts as a blind loop, and treatment differs from that of biliary-digestive anastomotic stenosis.
We present the case of a 67-year-old male patient who had been hospitalized to study obstructive jaundice with no associated pain that had been progressing over the course of a month. Ultrasound and abdominal CT showed evidence of intrahepatic bile duct dilation and acalculous gallbladder. Retrograde endoscopic cholangiography revealed stenosis of the common bile duct at the hilum, suggestive of a Klatskin tumor.
A metallic biliary stent was implanted through the stenosis and bile was collected for cytology, which confirmed the presence of malignant cells. The imaging study showed no signs of vascular involvement or metastatic dissemination. The patient underwent resection of the extrahepatic bile duct, both hepatic ducts up until the second bile duct bifurcation, and liver segments i and ivb. Reconstruction was performed using a Roux-en-Y hepaticojejunostomy with 4 liver ducts (right anteromedial and posterolateral and left segmental ii and iii). During the postoperative period, a self-limiting anastomotic fistula was observed.
The pathology exam reported a hilar cholangiocarcinoma with possible involvement of the proximal resection margin that was difficult to assess due to the inflammatory process associated with the stent.
Thirteen months after the intervention, the patient once again developed progressive obstructive jaundice associated with high CA 19-9 tumor marker levels. Magnetic resonance cholangiopancreatography observed dilation of the left segmental and right anteromedial sectorial ducts, with atrophy of the adjacent liver parenchyma. The symptoms, elevation of tumor markers and type of initial surgical resection (probably R1) suggested tumor recurrence. Further surgery was ruled out and we opted to perform palliative percutaneous bile drainage.
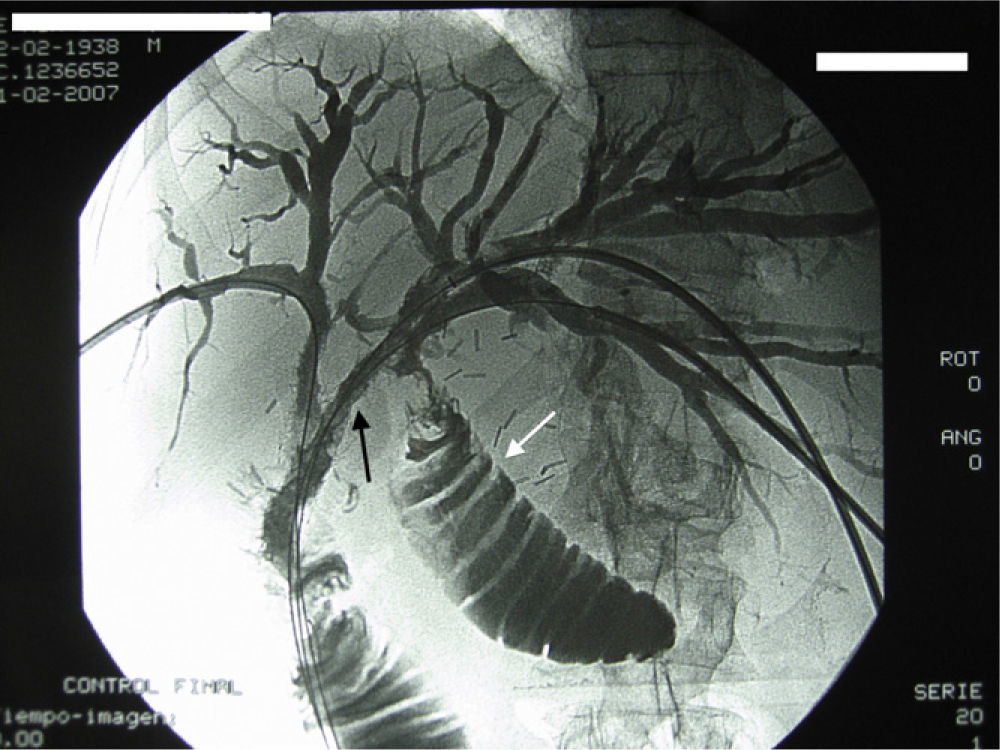
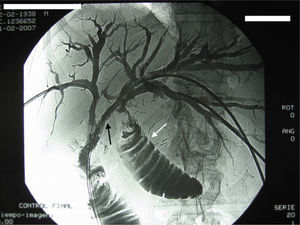
Percutaneous transhepatic cholangiography showed evidence of a tumor mass that affected the afferent loop of the hepaticojejunostomy, causing an obstruction with the appearance of a blind loop toward the proximal end where the left ducts drained. At first, an internal-external bile drain tube was inserted in the right anterior sectorial duct and external bile drainage was performed of both the left ducts. Afterwards, the duct of segment ii was guided with a metal guide through the tumor stenosis to connect the blind loop with the functional loop. The third step was to repeat the procedure through the duct of segment iii,and in both left segmental ducts we inserted 8mm×60mm and 10mm×100mm stents, respectively (Fig. 1). The follow-up cholangiography showed proper passage of the contrast to the intestine. The patient presented complete resolution of the jaundice and remained asymptomatic and with a good quality of life 5 months later.
The options for non-surgical palliation of malignant bile stenosis have practically substituted surgery for this category of patients with a life expectancy of less than one year.4
In our case, the initial intervention involved extensive resection up to the second bifurcation of the intrahepatic bile ducts. The very low probability of being able to perform radical resection of the recurrence and the technical difficulties of carrying out another bile tract reconstruction led us to rule out re-operation.
In elderly patients or in those with disseminated disease of the liver/peritoneum, the therapeutic options that should be considered are radiotherapy and external biliary drainage. In contrast, in some young patients with unresectable tumors but with a good quality of life, external biliary drainage is not the best alternative.
In the case we have reported, the functioning liver remnant was the left lobe, as the right liver had become largely atrophied. Nonetheless, left biliary drainage was done into a blind loop, so an internal bile stent inserted at this level would not have palliated the jaundice.
In select cases, some authors advocate surgical bypass of the blind segment to another jejunal loop.5 This technique, however, is rarely used nowadays due to the high risk of anastomotic dehiscence in patients with important alterations in their general and nutritional status.
Transtumor internal by-pass with self-expanding stents used in gastrointestinal and colon anastomoses is a common technique in patients with gastric/colorectal cancer recurrence.2,6–9 In an extensive review of the literature, we have not found any publications of an approach similar to what we have described for malignant stenosis of biliary-digestive anastomoses.
In our case, there were no complications related to the procedure, such as digestive perforation or hemorrhage. This suggests that, when done by expert hands, the approach described can resolve the obstruction of the afferent loop of a biliary-digestive anastomosis quickly, painlessly and satisfactorily.
Please cite this article as: Mocanu SN, González López JA, Villalba Auñón J, Artigas Raventós V. Tratamiento percutáneo de una obstrucción tumoral de asa aferente de hepaticoyeyunostomía. Cir Esp. 2014;92:209–210.