In MAMMARY tumors that are large relative to breast-size, complex reconstructive methods are required. We describe an alternative system of closure. In circumstances such as this, primary closure of this skin defect may be enabled by stress relaxation of the skin and the use of a tension-relief system. Tension-relief systems secures immediate primary closure of large skin defects in patients with large for breast-size tumors by placing the tension away from the skin edges. This enables early skin closure and rapid mobilization with good functionality. Optimal healing facilitates postoperative radiotherapy on time without reconstruction failure.
En los tumores MAMARIOS grandes en relación con el tamaño de la mama, se requieren métodos reconstructivos complejos. Se describe un método alternativo de cierre, QUE PERMITE EL cierre primario del defecto mediante la relajación de la piel y el uso de un sistema de relajación-tensión. Estos sistemas de relajación permiten el cierre primario inmediato de grandes defectos cutáneos en pacientes con tumores que son grandes en comparación con el tamaño de la mama. El cierre de la herida quirúrgica sin tensión en los bordes permite una curación temprana y una rápida movilización con buena funcionalidad. Una curación óptima facilita la radioterapia postoperatoria a tiempo sin errores en la reconstrucción.
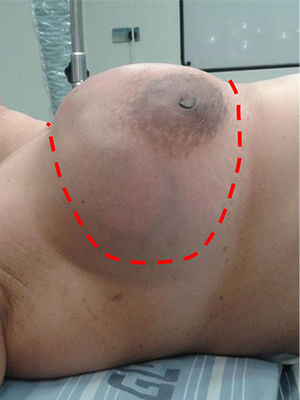
The local treatment of phyllodes tumors of the breast is complete surgical excision including tumor-free surgical margins, preferably more than 1cm from the tumor margins.1 In as many as one third of the patients, the tumor is large and mastectomy is necessary to achieve proper resection.1,2 Depending on the size of the tumor relative to the breast, primary simple mastectomy closure may not be possible in various patients and some method of reconstruction may be necessary in order to close the skin defect.3–6 We report an alternative technique of immediate primary closure of a wide skin defect, that would not be considered for primary closure with suturing techniques, following resection of a large phyllodes tumor.
Surgical TechniquePublication was approved by the institutional review board of the HYMC Medical Center (protocol HYMC-0028-17) and informed consent was obtained for publication of representative de-identified images.
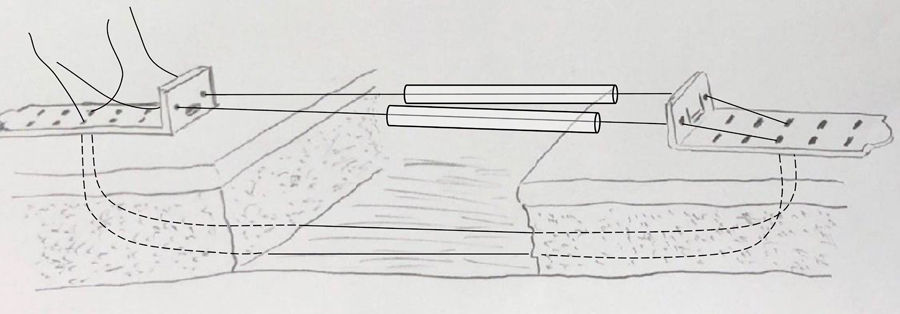
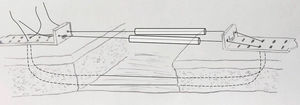
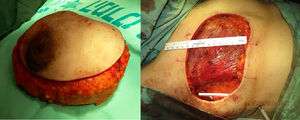
Tension Relief SystemThe TopClosure® Tension-Relief System (TRS) (TopClosure®, IVT Medical Ltd., Ra'anana, Israel) has been previously described in detail.7 It is comprised of 2 malleable polymer attachment plates that are placed at a distance of 2–3cm from the wound edges. The plates adhere to the skin by adhesive and/or secured with regular skin staples. Several pairs of plates are placed along the wound edges. Tension sutures including the skin and subcutaneous tissue are placed through opposing plates (Fig. 1). By pulling together the ends of these tension sutures, wound edges advance towards each other. Repeated application of tension by stress-relaxation results in gradual approximation of the skin. Alternating between the different tension sutures, tension is applied for 30s followed by a period of relaxation of 1−2min. Once the wound margins are approximated, the tension sutures are tightened and locked on top of the plates. The system also includes interconnecting approximation straps that may be used, if needed, for additional incremental advancement of wound edges through a lock/release ratchet mechanism.
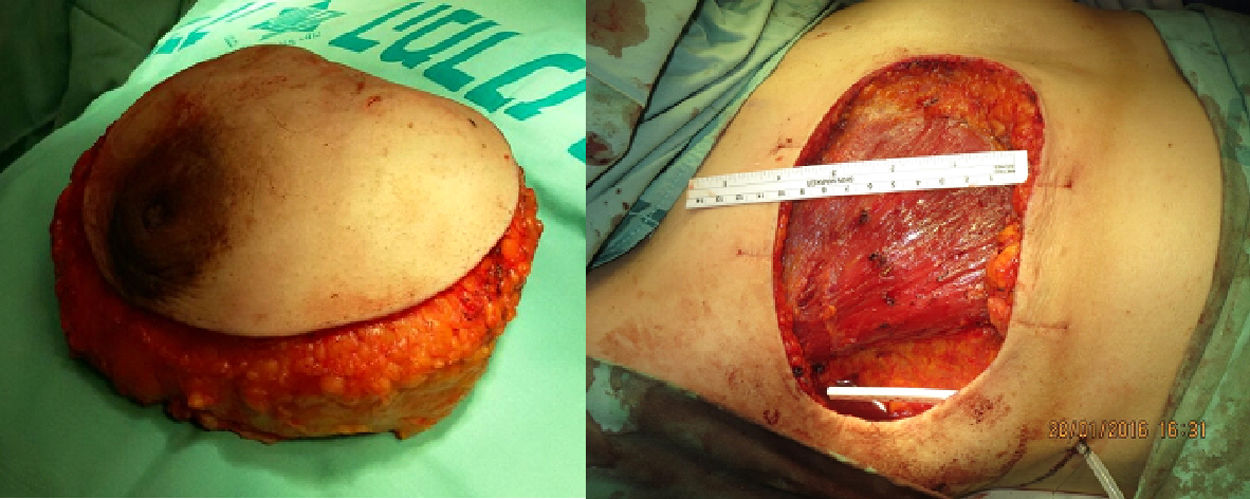
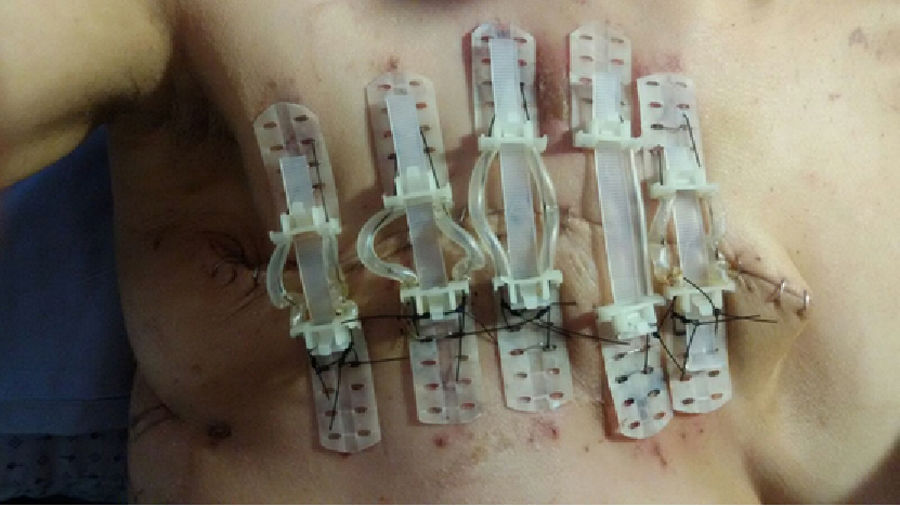
ProcedureUnder general anaesthesia the breast containing the tumor is widely excised (Figs. 2 and 3). Following resection, no further undermining of the skin is performed and several TopClosure® 8mm sets are applied for immediate primary wound closure without undue tension of the skin edges. Several pairs of plates placed along the wound edges are required for closure reinforced by 0 nylon tension suture on each TRS set. The subcutaneous tissue is approximated with absorbable sutures and the skin edges are leveled by skin staples (Fig. 4).
Application of the TopClosure® Tension-Relief System allows approximation of the wound edges within 30min of repeated stress-relaxation. Since the surgical wound is closed without excessive tension, the patient may start physiotherapy the following day, with the aim of conserving range of motion of the shoulders and upper extremities. The staples are removed in stages within two weeks and the plates held by tension sutures are gradually removed at 3–4 weeks.
DiscussionVery large for breast size phyllodes tumors may pose a reconstructive challenge in cases where adequate tumor-free margins mastectomy result in a wide skin defect that does not allow primary wound closure. Closure of these defects is usually achieved by either skin graft, local skin flaps or myocutaneous flaps, the most common being a lattisimus myocutaneous pedicle flap.3–6 Myocutaneous flaps are necessary when immediate breast reconstruction is being considered.5 Some authors have advocated conservation of healthy looking overlying skin in order to allow primary wound closure, to avoid more complex reconstructive procedures.3 This method, however, may compromise surgical margins in a disease in which positive excision margins are correlated with local recurrence of the tumor.
We describe the use of a TRS for primary closure of a large skin defect, avoiding the need to extend the scope of surgery with skin grafting or flaps and avoiding the possibility of donor site morbidity. One of the authors (MT) has extensively applied this system in both trauma and oncologic surgery, in cases were primary closure would have resulted in undue tension and ischemia of the wound edges.8 The TRS allows tension to be spread over a large area and placed away from the wound edges in an area that is better vascularized and not jeopardized by common surgical manipulations such as tissue undermining and pull. Repeated cycles of tension and relaxation lead to skin relaxation and early wound edge approximation during surgery. In order to avoid tissue ischemia by excess tension, undermining of the skin and subcutaneous tissue should be avoided. Placement of the tension sutures through the plates avoids the common skin damage by the tension sutures themselves. Postoperatively, the patient can be rapidly mobilized since added tension by early shoulder movement does not translate into direct tension on the wound edges, thus providing improved functionality.
In clean wounds in which the aim is to perform immediate primary closure, the main theoretic obstacle may be an extensive gap that cannot be approximated during surgery even following stress relaxation. Even then, approximation of the skin minimizes the gap facilitating eventual closure by either delayed mechanical creep or other techniques.8,9 Postoperative pain is usually not a limitation since the skin of the chest becomes relatively innervated following mastectomy. The only contraindication to the use of TRS is the situation in which approximation of the tissue will aggrevate or create compartment syndrome. Scarred, non-elatic tissues are no amenable for closure with TRS.
In conclusion, the TRS allows a straightforward safe immediate primary closure of high-tension mastectomy wound preserving tissue vitality that is sufficient to withstand acute surgical tension and postoperative irradiation challenge (Fig. 5).
Conflict of InterestsMoris Topaz is one of the developers of the TopClosure® Tension-Relief System. He is also the chairman of IVT Medical Ltd., manufacturers of the TopClosure® Tension-Relief System. Itamar Ashkenazi and Oded Olsha have no funding or other conflicts of interest to disclose.
The authors wish to acknowledge the help provided by Fernando Turégano Fuentes.
Please cite this article as: Ashkenazi I, Olsha O, Topaz M. Sistemas de relajación de la piel para el cierre de grandes defectos mamarios. Cir Esp. 2020;98:154–157.