Classically, patients with stage IV malignant melanoma presented an ill-fated short-term prognosis with an average survival of less than 6 months.1 However, thanks to advances in new targeted therapies, drugs have been developed that have increased progression-free survival, with overall survival rates of more than 2 years.2,3 These drugs include mitogen-activated protein kinase (MAPK) pathway inhibitors and immunotherapy with immune check-point inhibitors, including CTLA-4 inhibitors, anti-PD1 and anti-PD-L1 agents.4–6
This remarkable increase in survival in patients with advanced disease redefines the importance of surgical treatment for complications of disease progression, which until now has not provided a clear benefit in the evolution of the disease. We present a clinical case as an example of the role of surgery in combination with new targeted therapies for the treatment of metastatic melanoma complications.
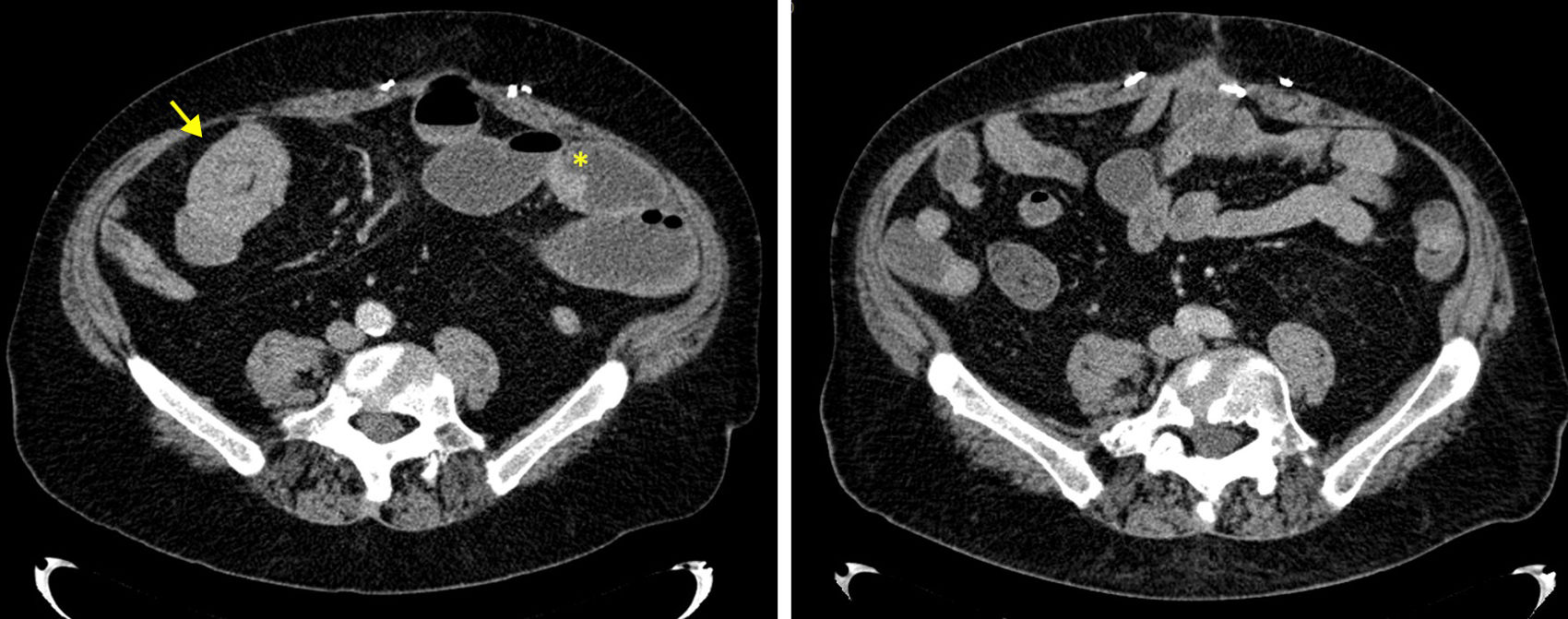
The patient is a 65-year-old male who was diagnosed in November 2012 with stage IIIc malignant melanoma after the appearance of an axillary conglomerate of lymph nodes with no known primary melanoma. Axillary lymphadenectomy was done of the 3 axillary levels. Subsequently, the patient was lost to follow-up, and 2 years later he came to the emergency room due to an intra-abdominal abscess secondary to a perforation of cecal metastatic melanoma. An extended right hemicolectomy was performed, and the posterior patient progression was positive. The study of the hemicolectomy piece demonstrated the presence of malignant melanoma metastasis with mutation for BRAF V600E. Three years later, the patient came to the emergency room due to intestinal obstruction and severe anemia (hemoglobin 3.9g/dL). Abdominal CT scan (Fig. 1) showed a small bowel obstruction secondary to intestinal intussusception in the ileum due to a 24mm tumor, associated with 4 pedunculated intestinal lesions along the small intestine (from the angle of Treitz to the distal ileum) suggestive of metastatic melanoma. Given the good clinical situation of the patient, the irreversible obstruction due to an intestinal recurrence and the knowledge of a previous recurrence with BRAF mutation, we decided to perform surgery to resolve the intestinal obstruction, followed by directed pharmacological treatment. In surgery, the preoperative findings were confirmed (Fig. 2) and ileal resection was conducted, which was limited to the intussusception and end-to-end anastomosis, without resection of the other identified metastases. The pathology results were again positive for malignant melanoma with BRAF V600E mutation, so treatment with dabrafenib and trametinib was initiated. From the second month after the start of the directed therapy, complete radiological response was observed on abdominal CT scan, showing macroscopic disappearance of the rest of the intestinal lesions. After 12 months of treatment, the patient remains asymptomatic, with complete radiological response and good tolerance to treatment.
Axial tomography of the abdomen showing the intussusception causing the intestinal obstruction (left, arrow) and the presence of other tumor implants (left, asterisk). Right photo, follow-up 12 months after surgery where the disappearance of the intestinal metastatic melanoma lesions is observed.
Approximately 40%–50% of melanomas present a mutation of the BRAF protein. This protein participates in the regulation of cell growth through the activation of mitogen-activated protein kinase (MAPK) (Ras/Raf/MEK/ERK),2 which stimulates cell proliferation by activating the transcription of cellular DNA. The mutation in BRAF V600E produces a change of protein conformation that leads to constitutionally elevated kinase activity, so the inhibition of the proteins in this pathway (BRAF and MEK) blocks cell proliferation.3 Two BRAF inhibitors are dabrafenib or vemurafenib. In metastatic patients, both have been shown to be superior to classical chemotherapy in response rate, progression-free time and overall survival.7,8 The combination with MEK inhibitors (trametinib or cobimetinib) is superior to any single treatment, demonstrating a significant improvement in survival. For this reason, they are currently considered therapies of choice in patients with metastatic melanoma who present a BRAF mutation.6,9 Intestinal metastases of melanoma are rare but may cause intussusception, obstruction or gastrointestinal bleeding.10 Historically, the possibility of surgical intervention has been assessed in those patients where resection of all macroscopic lesions was possible, since the existence of residual disease led to poor progress, with a mean survival of 4 weeks after surgery.10 In our case, the resection of all the intestinal disease was not viable, as the lesions were located along the small intestine and the resection would have to cover almost the entire intestinal tract. Knowing that the patient had a previous metastatic lesion with a BRAF V600E mutation, we planned a surgical procedure focused on the obstructed segment, associated with complementary treatment with dual drug blockade. Currently, we have tripled the expected survival of the patient with this strategy, which will probably be extended given the involution of the remaining lesions. This result is in line with recent clinical studies.4 In the current therapeutic scenario of melanoma, the surgery of complications secondary to disease progression has a relevant role (even if complete tumor resection is not achieved) in patients in whom these targeted oncological treatments can be offered, providing longer survival after resolving the complication.
Please cite this article as: de Miguel M, Jimeno J, Vidal J, Segura S, Lorente L. Tratamiento quirúrgico de rescate en paciente con melanoma metastásico con mutación BRAF V600E. Cir Esp. 2018;96:665–666.