Injuries to the portal vein are uncommon and are secondary to open abdominal trauma in approximately 90% of cases.1
In closed abdominal trauma, such injuries are even rarer and are caused by either avulsion or thrombosis.1,2 Most patients affected by this type of lesion are in severe shock and the diagnosis of portal vein damage is made during surgery.3
Isolated thrombosis of the portal vein after trauma is exceptional,4 and there are only 8 documented cases published in the literature.5
We report the case of a woman who presented with atrophy of the right liver and cirrhosis established 7 years after injury to the right hypochondrium, which had not been treated surgically.
A 53-year-old woman came to our clinic with epigastric abdominal pain. Abdominal ultrasound revealed the absence of the right hepatic lobe and a hypertrophic left lobe. Abdominal computed tomography confirmed the ultrasound findings and showed a small remnant of the right liver.
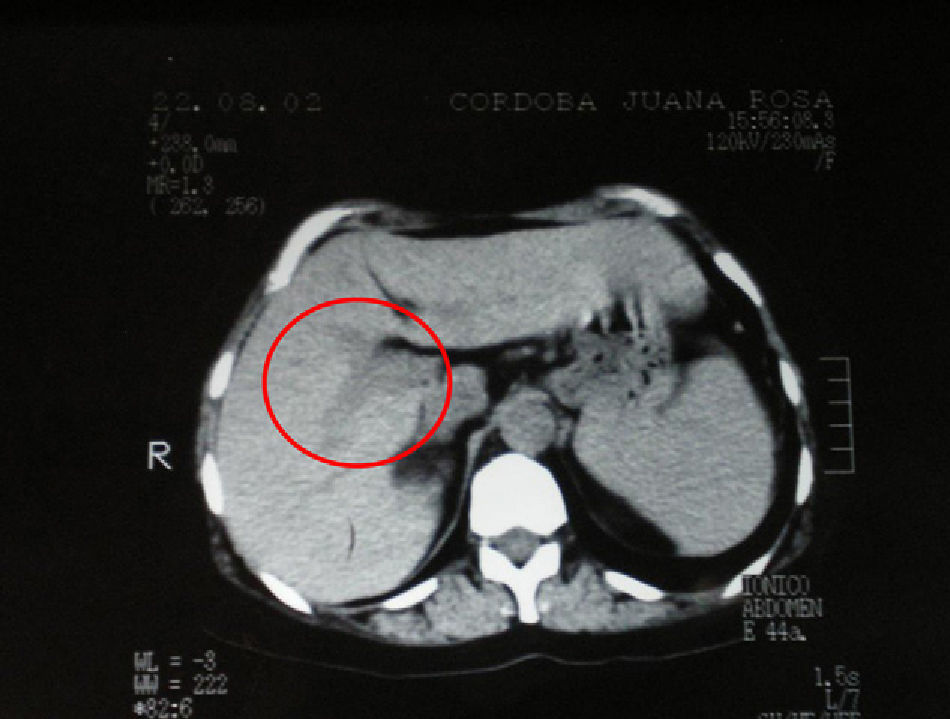
The patient's medical history included abdominal trauma to the right upper quadrant 7 years earlier (Fig. 1). The CT scan at the time was reviewed, and the liver was observed to have a normal size and shape.
Magnetic resonance angiography showed hypertrophy of the left liver with atrophy of the right liver with a small right portal vein branch irrigating the residual flap (Fig. 2). In the left liver, which is completely dysmorphic, the left portal vein branch is observed. The arterial distribution is similar.
An upper gastrointestinal endoscopy revealed esophageal varices, and the liver biopsy presented grade 3 fibrosis.
Abdominal trauma represents 7%–10% of traumas in general; it entails high morbidity and mortality, and is responsible for 10% of trauma deaths.6
Portal vein lesions are uncommon and are generally produced by open abdominal trauma. Some studies report an incidence of portal vein injuries from 0.07% to 1% in patients treated in specialized trauma centers.1–6
Closed abdominal trauma is an exceptional cause of isolated portal vein injury, and there are not many reports of this entity in the literature.1 These lesions are generally accompanied by hepatic, pancreatic and renal lesions. In a series of 2000 patients, Kenneth reported that only 2 had isolated portal vein damage.1 The review by Beaufort confirms 8 cases published in the literature.7 Pereira Fraga, in a series of 1370 cases of abdominal trauma, reported 15 portal vein injuries and only one was due to closed abdominal trauma.3
Portal vein thrombosis is caused by the association of a local factor and a systemic factor.8–10 The main local factors include cirrhosis, hepatobiliary malignancy, abdominal inflammation or endothelial lesions that lead to the formation of thrombi, due to either trauma or surgical damage.
Systemic factors include hypercoagulable states such as hereditary and acquired coagulation disorders, hematological diseases such as occult myeloproliferative syndromes, and the use of oral contraceptives.8–10
In our patient, we suggest that the right liver atrophy is related to the external trauma. A detailed review of the post-trauma tomography revealed, in addition to a morphologically normal liver, a poorly defined portal vein wall, which in retrospect suggests endothelial damage. Other local or systemic causes that would justify the clinical symptoms had all been ruled out in our patient. This physiopathological mechanism has never been demonstrated in the literature because most patients with traumatic portal vein injuries do not survive the initial trauma.
In the acute stage of trauma, abdominal pain and blood test alterations may be observed, and thrombosis of the vein may be found with ultrasound or tomography.2–4 In spite of her trauma, our patient only experienced pain and, after 24h of observation, she was discharged after presenting no changes in her symptoms.
If the thrombosis is not discovered during its acute stage, as was the case of this patient, it can progress to a chronic state with portal cavernoma and consequent portal hypertension with its respective complications.2 Our patient developed cirrhosis.
The cases published in the literature report acute injuries with immediate medical resolution of the symptoms, but no long-term follow-up of these patients who presented pain as a dominant symptom. Likewise, our patient only presented with abdominal pain. In our search of the literature, we have found no published cases of this complication as a long-term development after this type of trauma.
Isolated portal vein injury is exceptional in closed abdominal trauma. Its frequency increases in cases with open abdominal trauma associated with other injuries.
In its acute phase, thrombosis can be detected and treated with anticoagulants. In its chronic phase, symptoms of portal hypertension may appear, and should be treated. In such cases, development of cirrhosis is possible.
Please cite this article as: Buabse FM, Palazzo A. Atrofia hepática derecha y cirrosis por traumatismo aislado de la vena porta. Cir Esp. 2013;91:133–4.