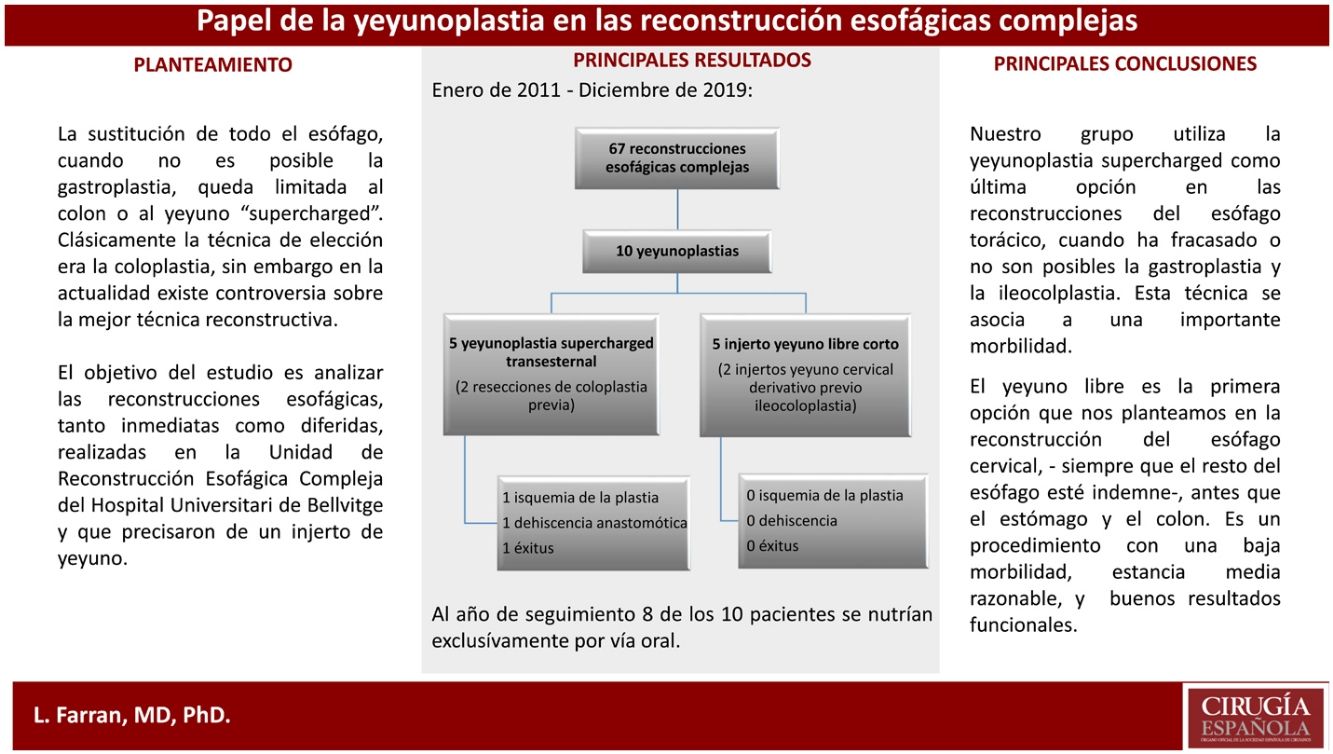
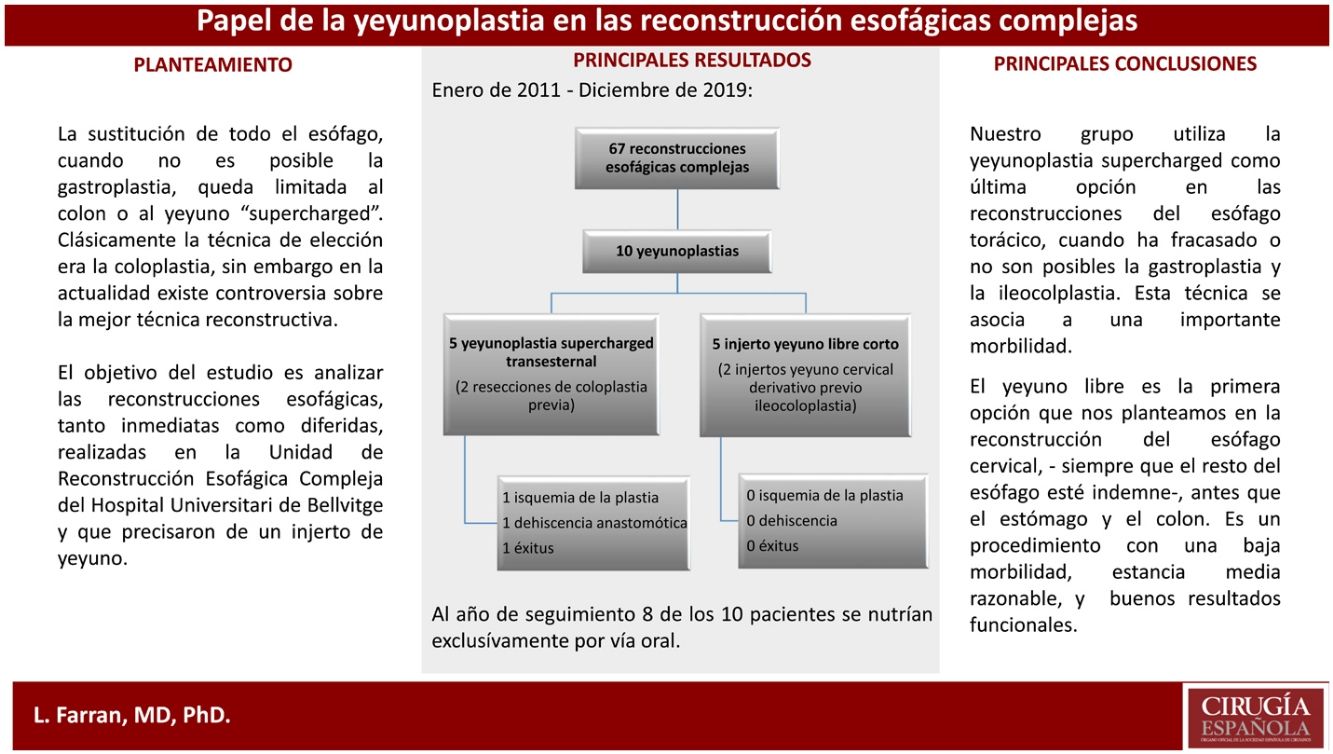
Esophageal reconstruction is a very complex surgical procedure, burdened by significant morbidity. Gastroplasty and coloplasty have classically been used. Free jejunal plasty has shown to be a very good option in the treatment of cervical esophagus pathology, but the role of supercharged jejunoplasty in thoracic esophagus reconstruction is still controversial.
MethodsA retrospective study of esophageal reconstructions with jejunoplasties performed in our unit between January 2011 and December 2019. Epidemiological data, indications, surgical technique, and morbidity and mortality were analyzed.
Results67 procedures of esophageal reconstruction were performed, 10 of which were jejunoplasties: 5 free jejunums and 5 supercharged. Morbidity, mortality, mean stay and withdrawal time from enteral feeding were lower in free than in supercharged jejunums.
ConclusionsSupercharged jejunoplasty was the last option for reconstruction of the thoracic esophagus. Median sternotomy access provides an excellent approach to the anterior mediastinum and the internal mammary vessels. The free jejunum would be the first choice, with the indemnity of the rest of the esophagus, in the reconstruction of the cervical esophagus.
La reconstrucción esofágica es un proceso quirúrgico técnicamente muy complejo, gravado por una importante morbilidad. Clásicamente se han utilizado la gastroplastia y la coloplastia, aunque la yeyunoplastia ya fue descrita por Roux en 1907. Parece demostrado que la plastia de yeyuno libre es una muy buena opción en el tratamiento de la enfermedad del esófago cervical, pero no está tan claro el papel de la yeyunoplastia supercharged en la reconstrucción del esófago torácico. El objetivo de este estudio es el análisis de las reconstrucciones esofágicas realizadas en nuestra unidad y que precisaron de un injerto de yeyuno.
MétodosEstudio retrospectivo de las reconstrucciones esofágicas realizadas con yeyunoplastias en nuestra unidad entre enero de 2011 y diciembre de 2019. Se analizan datos epidemiológicos, indicaciones, técnica quirúrgica y morbimortalidad.
ResultadosSe realizaron 67 procedimientos quirúrgicos de reconstrucción esofágica compleja de los que 10 fueron yeyunoplastias: 5 yeyunos libres en esófago cervical y 5 supercharged en esófago torácico con abordaje transesternal. La morbilidad, mortalidad, estancia media y tiempo de retirada de la alimentación enteral fueron menores en los yeyunos libres que en los supercharged.
ConclusionesEn nuestro grupo la yeyunoplastia supercharged es la última opción para la reconstrucción del esófago torácico; el acceso por esternotomía media nos permite un excelente abordaje del mediastino anterior y los vasos mamarios internos. El yeyuno libre sería la primera elección —con indemnidad del resto de esófago— en la reconstrucción del esófago cervical.
Deferred oesophageal reconstruction is a complex surgical procedure, with high morbidity and mortality associated with a high incidence of anastomotic dehiscence1,2. Gastroplasty has been the main option for the reconstruction of malignant conditions3, reserving coloplasty for benign conditions; it was considered to provide a functionally better result, although there are authors who dispute this4.
Although Roux, as early as 1907, was the first to replace the oesophagus by jejunum5, jejunoplasty did not become widespread. In 1946, Longmire described a long jejunal interposition with increased microvascularisation6. Allison7 confirmed the usefulness of a long segment of jejunum to replace the oesophagus and Ascioti8 published the first series of total oesophageal replacement with pedicled jejunum using the supercharged technique. Blackmon, in 2012, described his 10-year results with this technique9.
The suitability of the jejunum for oesophageal replacement is advocated because it is a relatively abundant organ, does not require prior preparation, has few specific diseases, has peristalsis and its calibre is similar to that of the oesophagus10. Its usefulness seems clear in cervical oesophageal resections as a free graft, microvascularised with cervical or mammary vessels11–14. A study comparing gastric pull-up reconstruction with free jejunal graft in cases of cervical oesophageal resection concluded that operative time and blood loss significantly increased in the gastric pull-up group, while graft survival was similar15.
Replacement of the entire oesophagus, when gastroplasty is not possible, is limited to the colon or supercharged jejunum. Bakshi et al. prefer right coloplasty as there is no need for the microvascular anastomosis required by the jejunum16. Other groups, however, suggest that the high rate of anastomotic dehiscence of colonic interposition is due to the volume of its intestinal flora, compared to the relative sterility of the jejunum17. Improved microsurgical techniques may be the reason behind the low rate of graft loss in jejunoplasty versus coloplasty18.
The aim of this study was to analyse oesophageal reconstructions, both immediate and deferred, performed in the Complex Oesophageal Reconstruction Unit of the Hospital Universitari de Bellvitge and which required a jejunal graft.
MethodRetrospective study of all patients who underwent oesophageal reconstruction with jejunal graft between January 2011 and December 2019. In the cases with an aetiology of antineoplastic treatment complications, all were free of active neoplastic disease. Those whose aetiology was an attempt at self-harm had been evaluated by the Psychiatry Service.
All patients underwent elective surgery performed by digestive surgeons and plastic surgeons in all cases; some procedures required the collaboration of cardiac, thoracic and ENT surgeons. We used the free jejunum graft as the first choice for reconstruction of short segments of cervical oesophagus, and reserved supercharged jejunoplasty for oesophageal reconstructions where gastroplasty and coloplasty had failed.
There was no specific preoperative preparation. Patients with jejunostomy did not follow a special preoperative diet prior to surgery.
We analysed epidemiological data, indications, type of surgery and morbidity and mortality.
The intervention is started in 2 fields simultaneously: cervical and abdominal.
In the abdominal field, through a median laparotomy, the angle of Treitz is identified and the jejunal segment irrigated by the second or third jejunal artery is selected, with a variable length depending on whether a short or long supercharged pedicled jejunal graft will be used. The jejunal vessels of the jejunal loop are dissected at their root. The mesentery is sectioned preserving the dissected main vessels and the jejunal loop with a Signia™ 710 linear stapler (Medtronic Parkway, Minneapolis, USA): proximal section in case of a supercharged long pedicled jejunum graft and a side-side (S-S) jejunal anastomosis with discontinuous manual absorbable suture in Roux-en-Y; proximal and distal section in case of a free jejunum, with discontinuous manual absorbable S-S jejuno-jejunal anastomosis.
The procedure is concluded by placing a naso-jejunal aspiration tube. No drains are left.
In the cervical field, a left cervicotomy approach is used. The cervical oesophagus is dissected and located using a Faucher oral probe. The thyroid-lingual-pharyngeal-facial trunk is located and dissected if using a free jejunum. If a long-segment supercharged jejunum is planned, a median sternotomy with Stryker System 6 oscillating saw (Syk Corp. 2825 Airview Blvd. Portage. 49002. USA) and the internal mammary vessels (between the second/third intercostal space) are dissected.
Supercharged jejunoplasty: ligation and section of the first 3 jejunal vessels at their root, perfused with 5% heparinised lactated Ringer’s solution.
Free jejunum: ligation and section of the jejunal vessels responsible for the vascularisation of the loop at its root.
Microvascular anastomosis under 15 or 20K magnification microscopy, between the internal mammary artery or a branch of the thyroid-linguo-facial trunk and the jejunal artery with continuous 8/0 nylon suture. For venous anastomosis we use the Microvascular anastomotic coupler device for mechanical vascular anastomosis (Microvascular anastomotic coupler. Alliance, Inc. a subsidiary of Baxter International Inc. Birmingham, Alabama). Jejunal flap viability is tested with IC Green infusion.
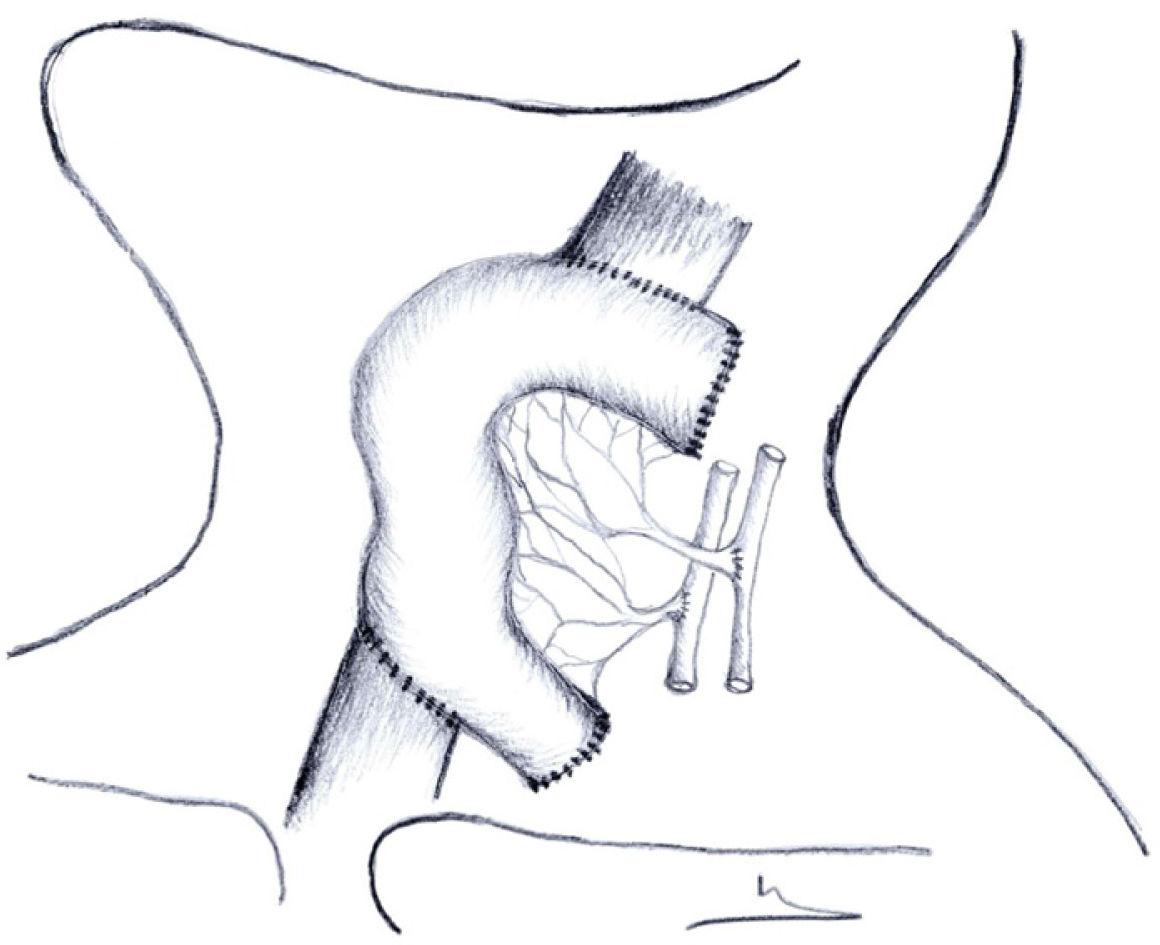
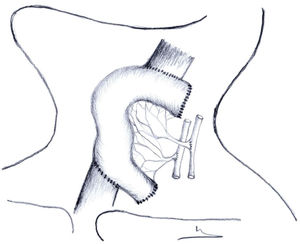
In free jejunal grafts, oesophago-jejunal and S-S jejuno-oesophageal anastomosis is performed manually with 3/0 discontinuous absorbable monolayer suture, or jejuno-cervical stoma with 3/0 absorbable loose stitches (Fig. 1). We do not leave a cervical drain.
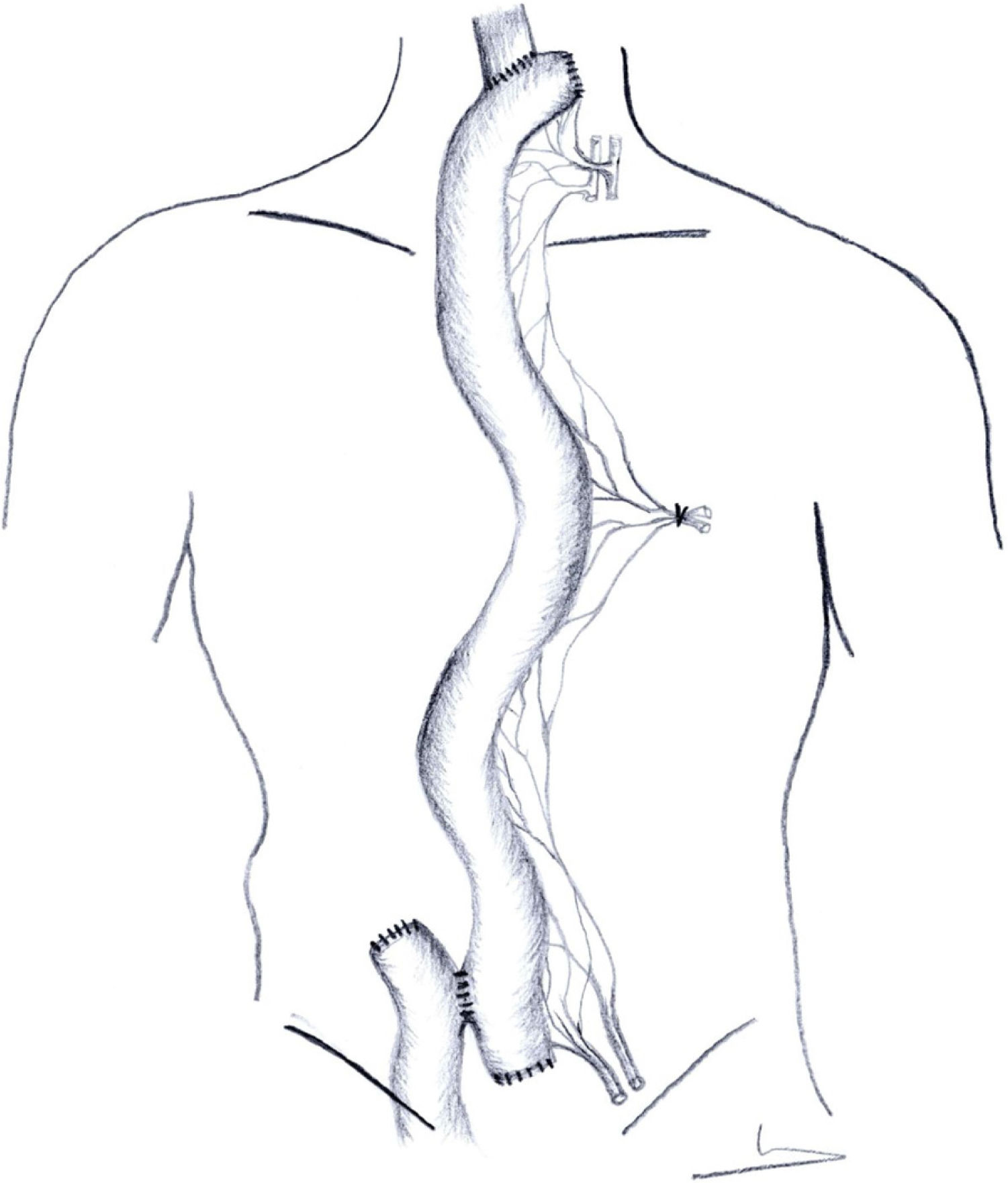
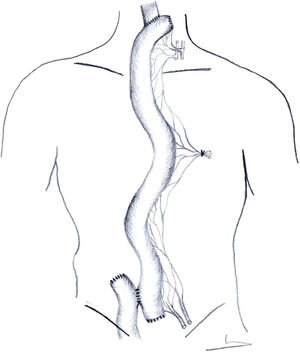
In supercharged jejunoplasties, the retrosternal jejunoplasty, oesophago-jejunal and jejuno-jejunal Roux-en-Y anastomosis are performed in the same way as described in the previous paragraph (Fig. 2).
In all cases we perform a Witzel-type feeding jejunostomy with Foley catheter n.° 14 (Well Lead Medical Co. Ltd. 511434 Panyu, Guangzhou, China).
Closure of sternotomy, laparotomy, and cervicotomy.
In the first 48–72 h, vascular viability is monitored with echo-Doppler. A cervico-thoracoabdominal CT scan is performed on the seventh day after surgery with oral and intravenous contrast. In the absence of dehiscence, oral diet is started.
Statistical analysisIBM SPSS version 18.0 statistical software (SPSS Inc., Chicago, IL, USA) was used for statistical analysis; median ± range was used in the analysis of quantitative variables.
ResultsFrom January 2011 to December 2019, 67 surgical procedures for complex oesophageal reconstructions were performed. The aetiology and the different surgical techniques used are detailed in Table 1. The indication was jejunoplasty in 10.
Aetiology and surgical procedure in complex oesophageal reconstructions.
| Aetiology | Patients | Procedure | Patients |
|---|---|---|---|
| Caustic ingestion | 27 | Ileocoloplasty | 39 |
| Complications of oesophagogastric oncological surgery | 19 | Gastroplasty | 13 |
| Boerhaave syndrome | 11 | Free jejunum + ileocoloplasty (2-stage) | 2 |
| Complications of GOR surgery | 4 | Supercharged ileocoloplasty | 5 |
| Oesophageal stenosis | 4 | Free jejunum | 3 |
| Granulosa cell tumour | 2 | Supercharged pedicled jejunum | 5 |
GOR: gastro-oesophageal reflux.
In 5 cases the reconstruction was performed with transsternal supercharged jejunoplasty, with resection of a previous coloplasty in 2 cases (Table 2). The mean operative time was 468 min (385–630). Complications included ischaemia of the plasty – secondary to bleeding from the arterial microvascular anastomosis – and a cervical fistula on postoperative day 8, which was resolved with conservative treatment (nil by mouth, enteral nutrition, broad-spectrum antibiotic therapy, and endoscopic sealing). The patient who presented with ischaemia of the plasty subsequently died of multi-organ failure. The median length of stay was 42 days (23–69).
Supercharged jejunoplasty.
| Patient-age in years | Aetiology | Previous surgery | Indication for surgery | Surgical procedure | Anastomotic dehiscence | Clavien–Dindo | Death | Hospital stay in days |
|---|---|---|---|---|---|---|---|---|
| Male, 72 | Gastric ulcer (1992) | Oesophago-gastrectomy | Adenocarcinoma in coloplasty | Transsternal colectomy Supercharged pedicled jejunoplasty | No | II | No | 23 |
| Retrosternal transverse coloplasty | ||||||||
| Male, 53 | Siewert III | Oesophago-gastrectomy | Ischaemic ileocaecal stenosis | Transsternal colectomy | No | IVa | No | 29 |
| Retrosternal ileocoloplasty | Supercharged pedicled jejunoplasty | |||||||
| Male, 49 | Siewert III | Oesophago-gastrectomy | Oesophageal disconnection | Transsternal supercharged pedicled jejunoplasty | Yes | IIIb | No | 69 |
| Retrosternal ileocoloplasty | ||||||||
| Ileocoloplasty excision | ||||||||
| Male, 66 | Siewert III | Oesophago-gastrectomy | Oesophageal disconnection | Transsternal supercharged pedicled jejunoplasty | Yes | V | Yes | 41 |
| Retrosternal ileocoloplasty | Ischaemia of the plasty | |||||||
| Ileocoloplasty excision | ||||||||
| Male, 62 | Caustic ingestion | Left hemicolectomy | Oesophageal disconnection | Transsternal supercharged pedicled jejunoplasty | No | IIIa | No | 48 |
| Oesophago-gastrectomy | ||||||||
| Retrosternal ileocoloplasty | ||||||||
| Ileocoloplasty excision |
In the other 5 patients a short free jejunum plasty was indicated for cervical oesophageal disease, with access via left cervicotomy (Table 3). In 2 cases of extensive oesophageal caustication (complete caustic stenosis at 1cm below Killian’s mouth) a cervical bypass jejunostomy was performed as the first stage of an ileocoloplasty; in 2 other patients with a granulosa cell tumour, cervical oesophageal resection with jejunal reconstruction was performed, and the last procedure was a cervical oesophago-jejunal-oesophageal bypass due to radical stenosis. The mean duration of surgery was 298 min (260–345). We had no cervical fistulae or mortality, and the median length of stay was 18 days14–21.
Free jejunoplasties.
| Patient-age in years | Aetiology | Previous surgery | Surgical procedure | Anastomotic dehiscence | Clavien–Dindo | Death | Hospital stay |
|---|---|---|---|---|---|---|---|
| Female, 36 | GCT cervical oesophagus | Cricopharyngeal myotomy | Cervical oesophageal resection | No | I | No | 20 |
| Free jejunum plasty | |||||||
| Male, 37 | GCT cervical oesophagus | No | Cervical oesophageal resection | No | II | No | 21 |
| Tracheal resection | |||||||
| Free jejunum plasty | |||||||
| End-to-end tracheal anastomosis | |||||||
| Tracheostomy | |||||||
| Female, 65 | Post-radiotherapy cervical oesophagus | Laryngectomy, gastrostomy, left supraclavicular plasty | Oesophago-oesophageal by-pass with free jejunum plasty | No | I | No | 14 |
| Female, 35 | Caustic stenosis cervical oesophagus | Oesophagogastrectomy | Cervical oesophageal bypass with free jejunum plasty | No | II | No | 17 |
| Tracheostomy | |||||||
| Male, 29 | Caustic stenosis cervical oesophagus | Tracheostomy | Cervical oesophageal bypass with free jejunum plasty | No | IIIb | No | 18 |
GCT: Granulosa cell tumour.
All patients were discharged with mixed oral and enteral diet via jejunostomy. In patients with supercharged jejunoplasty the median jejunostomy removal time was 141 days (87–194), and in the 3 who required a free jejunal graft it was 78 days (60–110).
Except for the 2 cases in which the free jejunum was the step prior to subsequent reconstruction with ileocoloplasty, the remaining patients, at 1-year follow-up, were exclusively orally fed. Two patients with supercharged ileocoloplasty were diagnosed with anastomotic stenosis and entered a programme of endoscopic dilatation.
DiscussionIt seems clear that, because of its sufficient length, predictable vascularity and requiring only one anastomosis, the stomach is the first choice for oesophageal replacement16. In the absence of a stomach, our group favours ileocoloplasty for oesophageal reconstruction that requires thoracoabdominal oesophageal replacement2. However, we agree with various groups that the free jejunum would be the first alternative in the approach to cervical oesophageal diseases11–14.
In the revision of our series, we used the supercharged jejunum when ileocoloplasty failed (Table 2). The transsternal approach was taken in the patient who developed a neoplasm in the coloplasty, as we had to perform an oncological resection prior to reconstruction19. Prior manipulation of the anterior mediastinum obliged us to consider the same approach in the other cases, which also facilitated dissection and identification of the internal mammary vessels for microvascular anastomosis. We would highlight that in 3 of these 5 patients this situation arose as a complication of surgical treatment for oesophagogastric oncological disease, and only in one case as a result of caustic ingestion. Although there are authors who advocate the supercharged jejunum as an alternative to the colon for oesophageal reconstruction in cancer patients8, we only indicate it after failure of a previous ileocoloplasty.
Morbidity was high (II, IIIa, IIIb, IVa, V of the Clavien–Dindo classification), mainly respiratory. We had one cervical fistula and one ischaemia of the plasty secondary to bleeding of the internal mammary artery which resulted in reoperation; the patient subsequently died of multi-organ failure. Despite the small number in our series, Barzin20, with the same number of cases and the same approach route (retrosternal), also reported 20% anastomotic dehiscence due to no graft loss. Chana21, with 11 patients and via subcutaneous route, reported 36.4% of cervical fistulas, with 0 losses of the graft. There was no mortality in either series. Our group used the subcutaneous route in a previous series of complex oesophageal reconstructions using the supercharged ileocoloplasty22, but the functional outcome was poor. Patients frequently required manipulation of the plasty for acceptable oral intake and the cosmetic outcome was extremely poor. Transsternal access to an anterior mediastinum with previous surgery ensures direct control over the entire course of the plasty, and facilitates dissection of the internal mammary vessels.
We used the free jejunum graft in 5 cases: in 2 patients with a granulosa cell tumour in the cervical oesophagus, one radicle stenosis and 2 stenoses post caustic ingestion (Table 3). The morbidity of the group was low (I, I, II, II, IIIB); we had no anastomotic dehiscence or mortality, and the mean length of stay was 18 days.
The oesophageal stenosis in the 2 patients caused by caustic ingestion was located 1 cm caudal to the pyriform sinus by fibrogastroscopy. We used the free jejunum as a preliminary step to definitive reconstruction, performing an oesophagocutaneous bypass, a classic ileocoloplasty with ileojejunal anastomosis was scheduled in a second stage. In 2 other patients, we proposed resection of the cervical oesophagus affected by a granulosa cell tumour23 and reconstruction with a free jejunum. In the case of oesophageal stenosis at 14 cm from the dental arch, we preferred to perform a bypass with free jejunum instead of a myocutaneous graft24, because of the 3 characteristics that we believe to be advantageous: the similar calibre between the cervical oesophagus and jejunum, the existence of digestive mucosa in both segments, and the presence of peristalsis.
Supercharged jejunoplasty is an alternative in the reconstruction of the thoracic oesophagus. The transsternal approach allows good access to the anterior mediastinum and facilitates dissection of the internal mammary vessels. It is surgery with significant morbidity.
The free jejunum is a very good option in the reconstruction of the cervical oesophagus – provided that the rest of the oesophagus is intact – and its usefulness and the advantages of jejunoplasty in replacing a short oesophageal segment have already been described by many groups. It is a procedure with low morbidity and a reasonable average length of stay, and has good functional results.
In our group, supercharged jejunoplasty is the last reconstructive option for the thoracic oesophagus when gastroplasty and coloplasty have failed. In cases of cervical reconstruction, the free jejunum is our first option to consider.
Conflict of interestsThe authors have no conflict of interests to declare.