Lymph nodes are the most common place of recurrence of papillary thyroid cancer, and surgery can be considered a therapeutic option. The risks of surgery increase with every intervention. We present 3 cases of cervical non palpable thyroid cancer recurrence managed with I125 seed radioguided cervical dissection from 2017 to 2019. Two of the cases had already a thyroidectomy and central compartment lymphadenectomy performed. The seed was placed guided by US on the lesion and its position was confirmed afterwards. The target was successfully localized in 100% of cases. There was no post surgery complications. There was no evidence of recurrence with a mean follow up of 15 months. Radioguided surgery using I125 seed it is a save technique and it offers a precise localization of the non palpable thyroid cancer recurrence.
El lugar más frecuente de recidiva del carcinoma papilar de tiroides es en los ganglios cervicales, siendo la cirugía una de las posibilidades terapéuticas. El riesgo quirúrgico para el paciente se incrementa con cada reintervención. Describimos 3 casos de disección cervical radioguiada con semilla de I125 en recidiva de cáncer de tiroides con lesiones no palpables, realizadas entre 2017 y 2019. Dos de los casos habían sido tratados previamente con tiroidectomía total y linfadenectomía del compartimento central. En todos los casos se colocó la semilla guiada mediante ecografía en la lesión sospechosa, comprobando su localización. La tasa de éxito para localizar el nódulo fue del 100%. No hubo complicaciones posquirúrgicas. Con un seguimiento medio de 15 meses no se han descrito recurrencias. La técnica radioguiada con semilla de I125 es segura y ofrece una gran precisión a la hora de localizar lesiones cervicales no palpables en recidivas de cáncer de tiroides.
Thyroid cancer is the most common endocrine cancer (95%). In most cases (90%), it is a papillary thyroid carcinoma, whose incidence is on the rise due to the greater use of cervical ultrasound in asymptomatic patients. Surgery is the primary treatment for these tumors. Total thyroidectomy is the technique of choice for tumors larger than 1 cm, although unilateral lobectomy may be an alternative to consider for differentiated tumors up to 4 cm. An adequate initial operation has an impact on the subsequent progress of the patient. The rate of lymph node involvement ranges from 20% to 90% and is more frequent in papillary carcinoma than in follicular carcinoma. While therapeutic central compartment lymph node dissection has become standardized, prophylactic central lymph node dissection is controversial and should be individualized in each case. However, its performance is accepted in tumors larger than 4 cm in diameter or with invasion of neighboring structures or lateral node involvement (cN1b), as well as in patients with risk factors for recurrence.1
Up to one-third of patients have a recurrence during follow-up, most frequently during the first 10 years after the initial surgery. Some 80% of recurrences occur at the locoregional level.2
Therapeutic dissection of the central and/or lateral compartment(s) of the neck in a patient with previous surgery must be individualized and assessed by a multidisciplinary team. This procedure should be performed in patients with persistent or recurrent disease, after biopsy confirmation, in central cervical lymph nodes ≥8 mm and lateral nodes ≥10 mm.3 Thyroglobulin is considered the most sensitive marker for detecting post-treatment disease.
Other treatment options include observation, I131 ablation, radiation therapy, radiofrequency, and tyrosine kinase inhibitors or drugs targeting vascular endothelial growth factor (VEGF) receptors.
Surgical TechniqueWe describe our experience with radioguided cervical dissection using I125 radioactive seed localization (RSL) between the years 2017 and 2019 in 3 patients.
All patients were women: 2 cases of recurrent papillary thyroid carcinoma, and one case of multifocal papillary microcarcinoma.
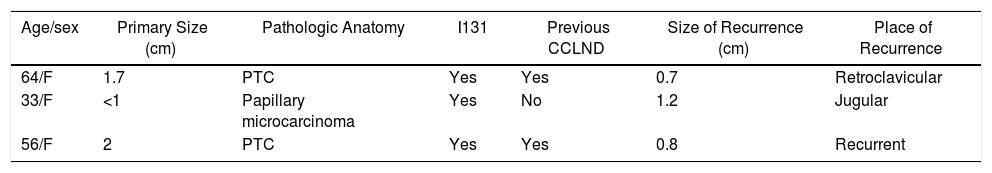
All patients received ablative treatment with I131. During follow-up, the nodule was identified in all cases by ultrasound, and the diagnosis was confirmed histologically by fine-needle aspiration. Central compartment lymph node dissection (CCLND) had been performed previously in 2 patients and the recurrence was localized, although in one patient it was the third cervical surgical intervention. The patient with papillary microcarcinoma, who had not previously undergone CCLND, presented recurrence in the right lateral compartment, for which CCLND and radioguided right lateral node dissection was carried out with I125 seed in the biopsied nodule to ensure its removal due to its small size in preoperative imaging tests (8 mm) (Table 1).
Characteristics of the 3 Patients With Recurrent Papillary Thyroid Carcinoma.
| Age/sex | Primary Size (cm) | Pathologic Anatomy | I131 | Previous CCLND | Size of Recurrence (cm) | Place of Recurrence |
|---|---|---|---|---|---|---|
| 64/F | 1.7 | PTC | Yes | Yes | 0.7 | Retroclavicular |
| 33/F | <1 | Papillary microcarcinoma | Yes | No | 1.2 | Jugular |
| 56/F | 2 | PTC | Yes | Yes | 0.8 | Recurrent |
PTC: papillary thyroid carcinoma; F: female; I131: iodine 131; CCLND: central compartment lymph node dissection.
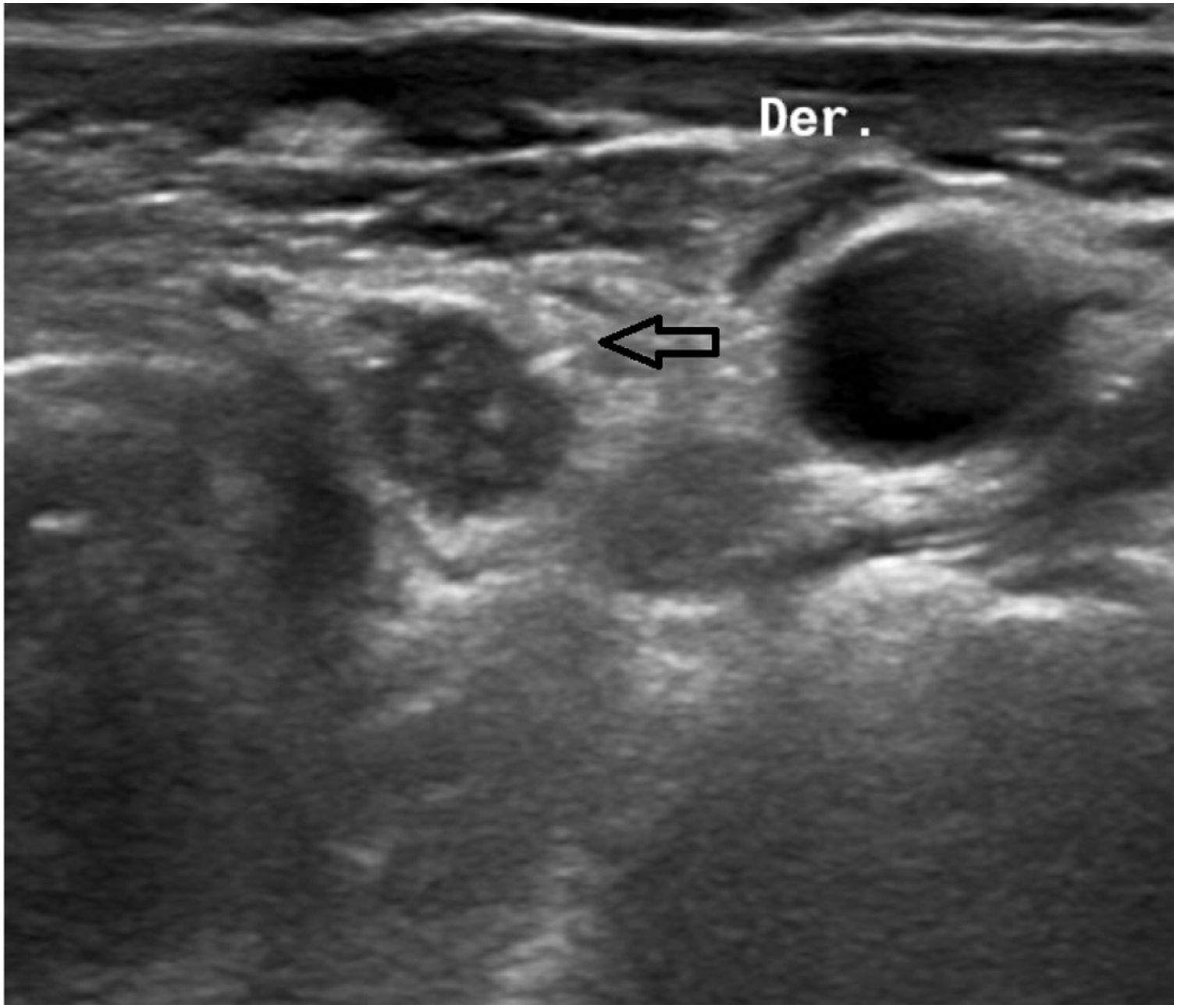
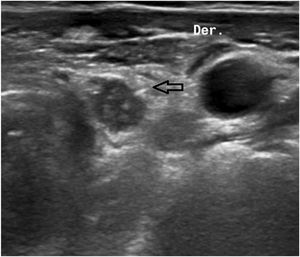
The ‘seed’ is a titanium capsule measuring 0.08 × 0.5 cm containing I125 (Fig. 1). It emits gamma radiation, allowing it to be detected at all times by a gamma probe. An 18 G needle is loaded with the seed and, guided by ultrasound, it is placed in the desired location. Once released, its location is verified by ultrasound (Fig. 2). In the Nuclear Medicine Unit, the probe locates the point with the highest count, a mark is made on the skin, and later the portable gamma camera is used for double-checking.
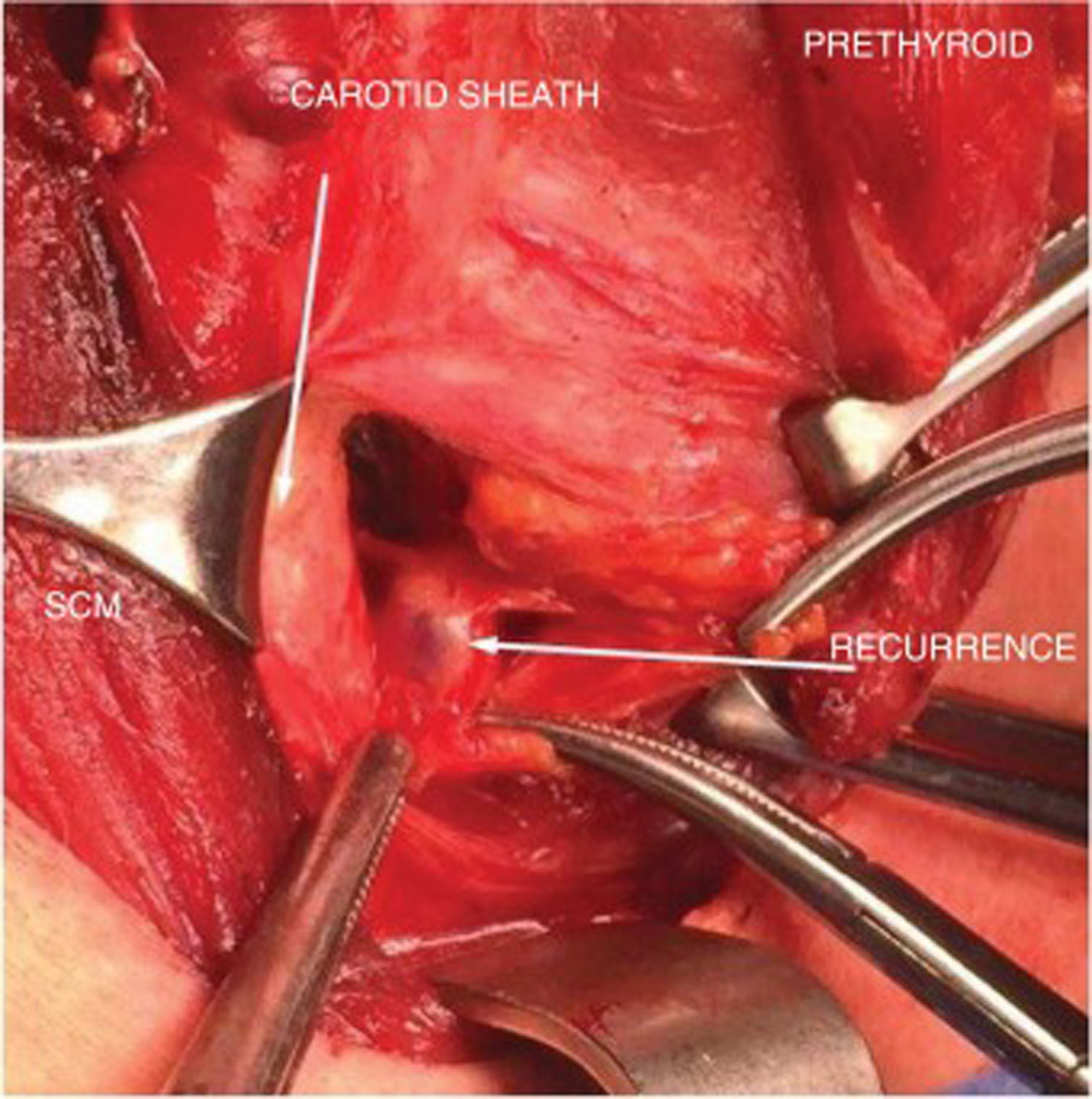
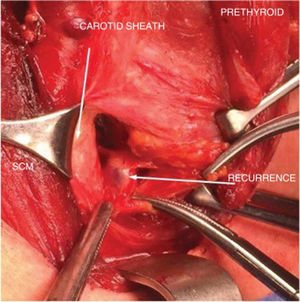
During the intervention, a small incision is made following the mark on the skin and coinciding with the previous transverse cervical incision. Probe-guided dissection is performed until the nodule or node where the seed is located is identified. It offers the surgeon the security of knowing the location of the seed and the lesion at all times, and the probe provides the ability to check each plane from all angles in order to find its exact location (Fig. 3). Once the lesion is resected, the surgical bed is again checked.
The success rate for locating the seed-marked pathological nodule was 100%. The seed did not migrate in any cases, and there were no postoperative complications. The hospital stay was one day in the 2 patients without extensive lymphadenectomies and 3 days for the patient with central and right lateral lymph node dissection.
During the 32-, 19- and 11-month follow-up periods, respectively, no new recurrences have been identified in our patients in the follow-up ultrasounds done to date, and baseline and stimulated thyroglobulin levels remain undetectable.
DiscussionAltered cervical anatomy, fibrosis and the difficulty to identify structures after an initial surgical intervention pose a challenge for surgeons and lead to increased surgical times and patient morbidity.4,5 Surgery involves risks, such as nerve damage, bleeding, hypoparathyroidism, as well as the inability to locate the recurrence because it may present a non-specific macroscopic appearance and be covered by other structures. For this reason, we consider it beneficial to perform radioguided surgery with I125 seeds in cases of non-palpable recurrence after thyroid surgery, mainly in patients with previous lymphadenectomy. The objective is to reduce postoperative complications and avoid failed resection of the nodule during the operation.
Several intraoperative localization techniques have been described, such as injection of dye,6 the use of a harpoon,7 and intraoperative ultrasound.8 Some of the disadvantages of these techniques are the diffusion of the dye to other tissues, patient discomfort and possible vascular complications, as well as the need for an ultrasound expert in the operating room.
Among the radioguided surgical procedures, the main technique implemented so far has been radioguided occult lesion localization (ROLL), which involves injecting a non-migrating radiotracer (generally Tc99m-MAA) into the lesion to detect the gamma radiation that it emits with a specific probe.9 The main disadvantage resides in the possible diffusion of the radioactive isotope, thus making it difficult to identify the outline of the lesion in the surgical field and unnecessarily extending the dissection and removing healthy tissue. Furthermore, it has a half-life of 6 h, which is a drawback for the coordination between the specialists participating in this technique.
In this study, we present the alternative used in our hospital: radioguided surgery using I125 seeds. This is a simple technique that offers the surgeon the security of knowing the exact location of the seed and the lesion at all times. In addition, its long half-life (59.4 days) allows for it to be placed days before surgery, thereby avoiding possible coordination problems between services and facilitating flexible organization. Despite being a radioactive material, the patient dose is really very low, even lower than that of a technique like selective sentinel lymph node biopsy, which is already being implemented.10
There is extensive experience in radioguided surgery using seeds in non-palpable breast lesions, a validated and standardized technique that has been used at our hospital since 2010 with great safety and efficacy. Likewise, radioguided surgery has been used in our center with I125 seeds in certain non-palpable soft tissue lesions since 2015, and we have been able to extrapolate this knowledge to patients with recurring non-palpable thyroid cancer lesions.
Our bibliographic search of the literature identified various articles about the use of I125 seeds for locating non-palpable soft tissue lesions. In contrast, we only found one study published in 2018 describing the experience in the use of seeds in 3 cases of recurrent papillary thyroid carcinoma. The authors conclude that it is a safe technique with no associated complications that provided correct identification of the marked nodule.11
Thus, the main indication for radioguided surgery with the RSL technique is in cervical recurrences of papillary thyroid carcinoma, with non-palpable nodules after thyroid surgery and previous lymphadenectomy. In turn, it is very useful to be able to mark a single non-palpable lesion in order not to lose the biopsied node due to its difficult location in the surgical field or due to its small size in the event of a lymph node dissection.
Precise localization of lesions could reduce surgical time, allow for smaller incisions and provide greater security for the surgeon, without increasing the complexity or complications of the operation. For these reasons, and within the framework of multidisciplinary and individualized treatment, radioguided seeds have become a therapeutic tool of choice at our hospital.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Vilar Tabanera A, Ajuria O, Rioja ME, Cabañas Montero J. Disección cervical radioguiada con semillas de I125 como tratamiento de la recurrencia de cáncer papilar de tiroides. Cir Esp. 2020;98:478–481.