In the last 5 years, we have witnessed a surge in the appearance of innovations in minimally invasive surgery. It all began with the advent of transvaginal cholecystectomy in 2007,1–3 which was followed by single-incision, single-port cholecystectomy.4–6 Although these new access methods have been shown to be safe in their early development, as demonstrated by the initial publications of clinical series done by groups who were quite convinced by the development of these techniques7,8 and by the National Register of Single-Port Surgery,9 their later extended use has demonstrated that we may be compromising patient safety.
Just as when the laparoscopic approach was universalized for cholecystectomy and there was much morbidity related to the common bile duct, we now find ourselves at a turning point where the universalization of single-incision cholecystectomy could repeat the same error. Moreover, in this new approach the morbidity could be twofold, affecting both the anatomical structures of the hepatic pedicle as well as the abdominal wall. By analyzing the data reported in our national register, one may think that this surgical technique is safe because there was neither mortality nor iatrogenic injuries of the common bile duct in a total of 745 cholecystectomies performed, in addition to there being a very low rate of complications with the umbilical access. But this view is somewhat biased. First of all, the register compiles data from the patients’ situations at a specific moment, but it does not report the long-term follow-up of these patients. Secondly, and more importantly, there are many Spanish cases that have not been reported to the register and have been done with different techniques, instruments and devices, with little or no possibility of auditing either initial or long-term results.
Greater postoperative morbidity with single-incision surgery has begun to be reported in some international publications. This should be a warning to us so that the same does not happen in our country. In 2010, there started to be reports of isolated cases of common bile duct injury and associated lesions in the hepatic pedicle.10,11 Garg et al.12 reported one case of bile duct injury in a short series of 35 patients (2.85%) and the need for additional ports in 28.5% of the cases in order to successfully complete the procedure. Joseph et al.13 performed a meta-analysis of 45 studies with 2626 patients and found a bile duct injury rate of 0.72% in the single-incision cholecystectomy group, a percentage that nearly doubles the universally accepted rates for conventional laparoscopic cholecystectomy of 0.4%–0.5%.
This has all been made worse by the economic situation that we are currently living in. Because of their higher cost, it has been difficult to incorporate the new single-port devices and articulated and pre-curved instruments in our armamentarium. This means that in some hospitals single-incision surgery is done under suboptimal conditions. The use of the glove-port is gaining in popularity,14 which is a low-cost solution that we are not going to criticize for being a “homemade” device. It allows for single-incision access and grouped entry ports with no massive leak of the pneumoperitoneum. However, this is a technique that must be sidelined when associated with the concept of “anything goes”. What is meant by this is that we frequently see the glove device used in association with straight instruments, standard-sized optics and angulations that are all inadequate for single-incision surgery. We should also add that there may be associated inadequate patient selection and deficient self-criticism, as it seems there is more concern for the resolution of the individual clinical case than for the overall progress of the technique and the approach. This can lead to a technique being discredited because of improper usage.
And we still have not analyzed the potential problem of the abdominal wall. It is early to be able to analyze what could happen in the medium term with the umbilical approach, but it is expected that series with long-term follow-ups will begin to report morbidity. We should begin to analyze entry port complications in detail. There are many questions that still have not been answered about this topic, such as how to perform the closure, whether to use a prosthesis or not, and infection and herniation rates.
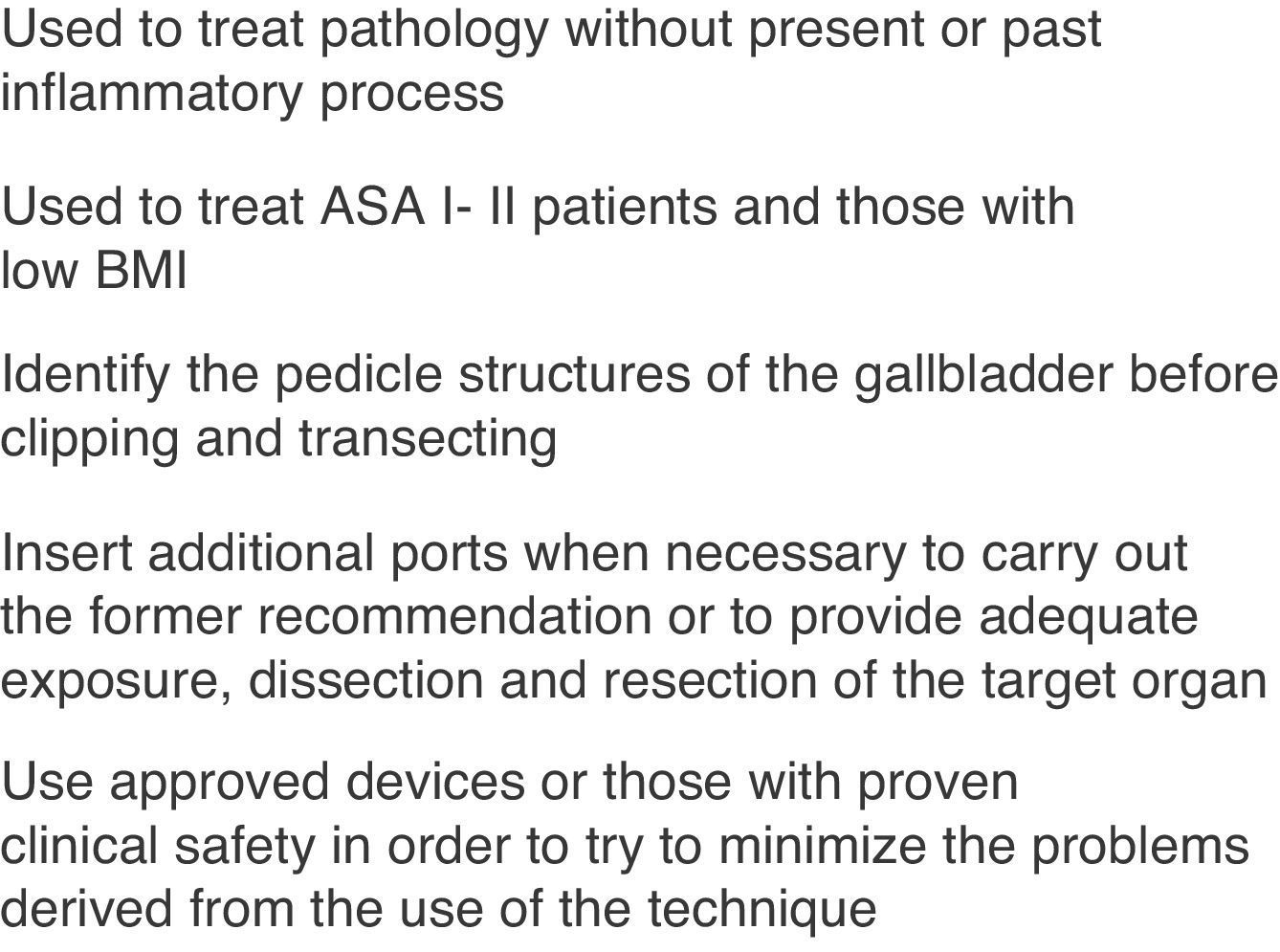
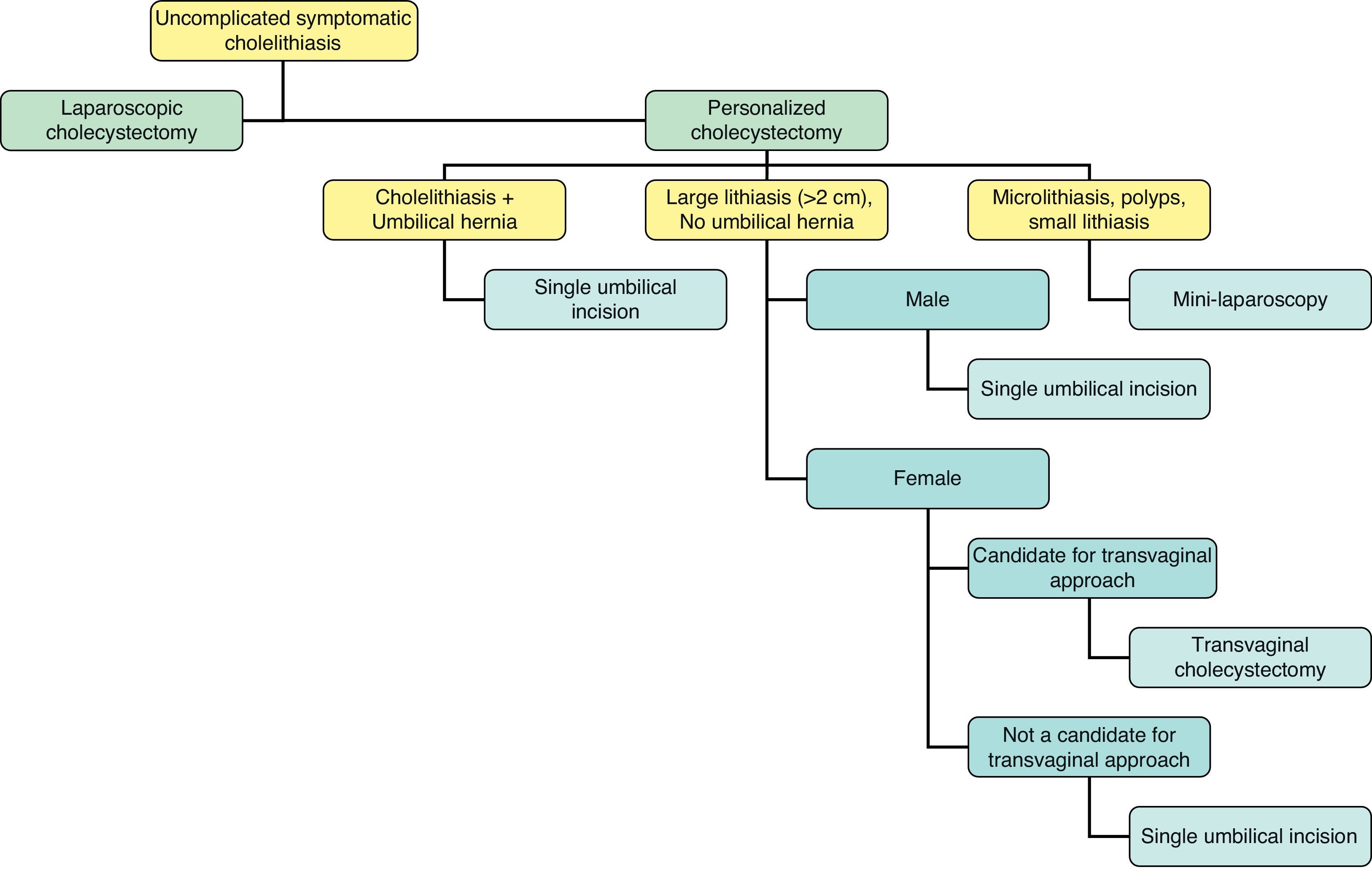
For these reasons, we should center our attention on a sensible use of single-port cholecystectomy in order not to repeat past errors by introducing innovation in minimally invasive surgery, which has enormous potential. To do so, we have included a series of recommendations followed by most workgroups that are concerned about the development of this technique and who defend the follow-up of cases as well as safety, based on a correct indication for surgery (Fig. 1). In the surgical indication of cholecystectomy, the appearance of all these new approaches sometimes leads us to ask which technique is ideal for each patient, since it is almost possible to choose “cholecystectomy à la carte”. As an example, we have provided a personal algorithm used for the indication of minimally invasive cholecystectomy by either conventional laparoscopy or using new approaches and techniques (Fig. 2).
As stated by Berci et al.15 in a recent editorial, in laparoscopic cholecystectomy our first premise should be not to cause damage, and the second should be to be careful with the presence of lithiasis in the common bile duct. Injury to the common bile duct has doubled in the era of laparoscopy compared with the era of open cholecystectomy, and we run the risk of it doubling once again in the era of single-incision cholecystectomy.
Please cite this article as: Noguera JF. Colecistectomía de única incisión: ¿una innovación segura? Cir Esp. 2013;91:401–403.