NSAID enteropathy is a very prevalent disease that is usually diagnosed after episodes of gastrointestinal bleeding or during the study of a malabsorption syndrome. However, the diagnosis of NSAID enteropathy after an episode of intestinal obstruction is rare and is usually due to diaphragmatic stenosis.
We present the case of an 89-year-old female patient who came to the emergency department for epigastric pain, vomiting and no passage of stools or gases for 4 days, associated with symptoms of asthenia and loss of 5kg in the previous 2 months. The most relevant medical history included the consumption of acetylsalicylic acid and omeprazole for more than 10 years.
On examination, she presented good general condition and hemodynamic stability. The abdomen was distended, with pain and guarding in the epigastrium but no signs of diffuse peritonitis.
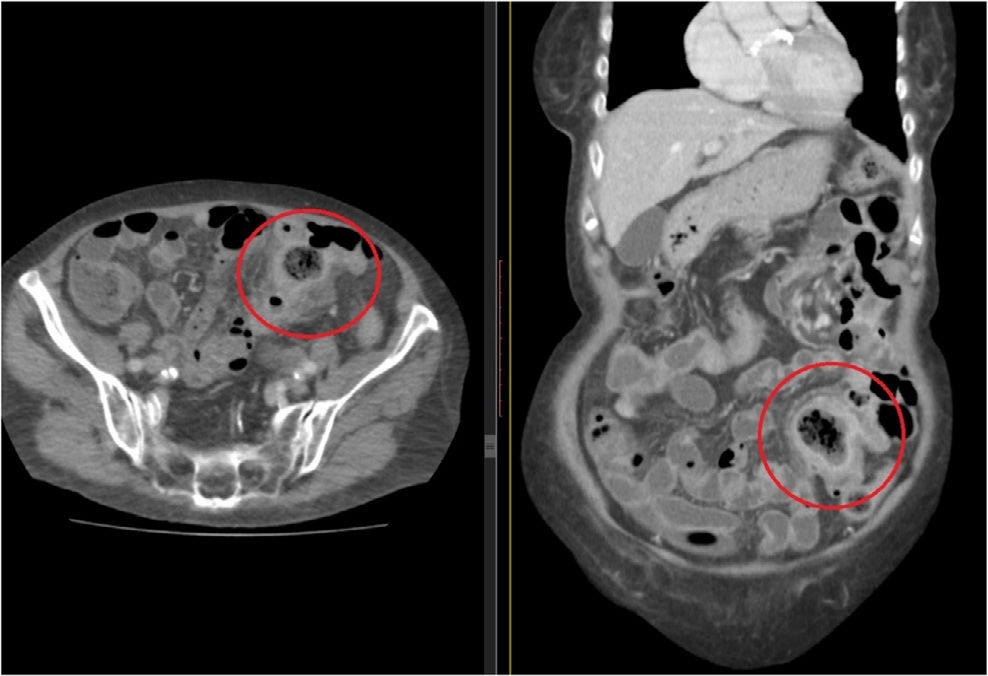
Lab work showed: hemoglobin 10g/dL, 12,000 leukocytes and C-reactive protein 56mg/L. Abdominal CT scan identified a gas-fluid collection in the left flank in close contact with intestinal loops and inflammatory changes in the adjacent fat, suggesting the presence of a perforated intestinal tumor (Fig. 1).
Exploratory laparoscopy showed 2 closely adhered bowel loops at the level of the distal jejunum and proximal ileum. With no dissection plane, a fistula between the 2 was a possibility. Both loops were exteriorized through an incision, and both were removed en bloc along with the mesentery. The procedure was completed with 2 intestinal anastomoses.
The patient was discharged on the fifth day after surgery.
The pathology results reported an ulcer of the mucosa with prominent reparative fibrosis and fistulization to the adjacent intestinal loop, with abscess in the mesentery but no signs of malignancy. These findings, together with the history of chronic aspirin consumption, led us to the suspected diagnosis of NSAID enteropathy.
An endoscopy was performed, which confirmed gastrointestinal lesions compatible with this diagnosis, and a Helicobacter pylori test was negative. This drug was withdrawn from the daily treatment and the patient was asymptomatic 3 months after the procedure.
Non-steroidal anti-inflammatory drugs are related with harmful gastrointestinal effects. Gastric and duodenal ulcers are the most frequently studied,1 but NSAID use can affect other areas of the digestive tract, such as the jejunum, ileum or colon.1
It is known that NSAIDs suppress the synthesis of prostaglandins in the mucosa, causing decreased mucus and bicarbonate secretion, reduced blood flow and epithelial repair, and altered immune function. In addition, they increase intestinal permeability, allowing for the passage of bacteria by increasing mucosal damage by activating neutrophils and nitric oxide synthesis.
However, it has been recommended that the enterohepatic circulation of some is the key factor2 in their pathophysiology.
There are studies that have found that the high intraluminal concentration of the drug causes increased permeability of the intestinal mucosa and rupture of the cell junctions, causing the drug to enter the enterocyte and causing mitochondrial injury and cell death.3 This will generate neutrophilic inflammatory infiltrate, the formation of predominantly circumferential and linear ulcers, with subsequent perforation, and the resulting process of fibrosis and scarring.
Although up to 70% of chronic consumers have some degree of enteropathy, it is underdiagnosed because most are asymptomatic. However, lesions can be found after 6 months of use.4 Capsule endoscopy has been fundamental in the study of this condition, especially in patients who have jejunal or ileal involvement.5 The degree of intestinal involvement will depend on the type of drug, dose, time of administration and patient tolerance. In the case of acetylsalicylic acid, the harmful effect is less frequent as it has greater gastric and duodenal absorption.6
While in chronic consumers the risk of presenting an acute complication like perforation or gastrointestinal bleeding is 3 times higher,7 the most frequent form of presentation is paucisymptomatic, such as small gastrointestinal hemorrhage and secondary anemia like a malabsorptive syndrome, and less frequently as intestinal obstruction due to diaphragm stenosis.8
In the latter case, the differential diagnosis will be carried out with neoplastic disease, taking into account other less probable possibilities, such as bands or internal hernias, invaginations or even inflammatory bowel disease.
However, no case has been reported in the literature like the one described above, in which we objectified an entero-enteric fistula, probably a consequence of the tissue ulceration and repair process, and which manifested itself acutely as an intestinal obstruction.
Treatment includes cessation of the consumption of these drugs. The use of proton pump inhibitors has not been shown to protect against their action. In fact, animal studies have demonstrated exacerbation of lesions due to alterations in the enteric bacterial flora.9 Sometimes surgery is required in cases with acute complications, such as perforation or intestinal obstruction, as in the case we report.
Please cite this article as: García-Romera Á, Soto-Darias I, González-Hernández S, González-Delgado C, Bravo-Gutiérrez A. Obstrucción intestinal secundaria a fístula entero-entérica: una rara complicación en consumidores crónicos de AINE. Cir Esp. 2020;98:245–247.