Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS) achieves the hypertrophy of the future liver remnant in seven days. We achieved the same hypertrophy placing a tourniquet in the parenchimal transection line associating a right portal vein ligation (associating liver tourniquet and right portal vein ligation for staged hepatectomy-ALTPS). In perihiliar tumors a “non touch” technique should be performed. ALPPS and ALTPS do not comply with this technical aspect because a dissection of the hilum is carried out in both procedures during the portal dissection. To avoid this problem we devised a new method called sequential ALTPS. It consists of placing a tourniquet in the umbilical fissure without ligation of the right portal vein during the first stage. Subsequently, on the 4th postoperative day we performed a percutaneous right portal vein embolization. We present the first case of this new technique in which we have obtained a hypertrophy of 77% of the future liver remnant seven days after portal vein embolization. In the second stage a right trisectionectomy was performed with inferior vena cava resection with a goretex graft replacement.
Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS) consigue la hipertrofia en 7 días del futuro remanente hepático. Nosotros conseguimos la misma hipertrofia colocando un torniquete en la línea de sección parenquimatosa con ligadura portal derecha (associating liver tourniquet and right portal vein occlusion for staging). En tumores perihiliares se debe realizar la técnica «non-touch», que las técnicas ALPPS Y ALTPS no cumplen al manipular el hilio hepático en la disección portal. Por ello, diseñamos este nuevo método que consiste en realizar la técnica ALTPS de forma secuencial, realizando en el primer tiempo la colocación del torniquete en la cisura umbilical sin ligadura portal derecha, y al 4° día postoperatorio la embolización portal derecha. En este caso el incremento del futuro remanente hepático fue del 77% al 7° día tras la embolización portal percutánea. En el segundo tiempo se realizó triseccionectomía derecha con resección de la vena cava inferior siendo sustituida por un injerto de goretex anillado de 2cm de diámetro.
Extensive liver resections often leave insufficient future liver remnant (FLR) when using intraoperative portal vein ligation and Percutaneous Portal Vein Embolization (PPVE) to achieve hypertrophy.1–4 These classic portal occlusion procedures lead to late hypertrophy (from 4 weeks), and tumor progression may exist.5,6 Recently, the procedure associating liver partition and portal vein ligation for staged hepatectomy (ALPPS)7–16 has been reported. It achieves greater and faster hypertrophy; it was therefore believed that it would avoid problems related to percutaneous portal embolization and intraoperative portal vein ligation.1–6
In 2011, we began using a variant of the ALPPS procedure17,18 where we did not partition the liver parenchyma, but rather occluded it by placing a tourniquet in the line of parenchymal section plus right portal vein ligation (associating liver tourniquet and portal vein ligation for staged hepatectomy – ALTPS). As recently published, our procedure reproduces the immediate postoperative results of the ALPPS procedure.19
For liver tumors proximal to the hilum or those invading it, “non-touch” procedure guidelines must be applied to prevent tumor dissemination; therefore, if the ALPPS or ALTPS procedure is performed, ligation of the right portal vein should be avoided, and if possible, also avoid sectioning the liver near the hepatic hilum. In our ALTPS procedure, no liver bipartition is conducted, since we only place one tourniquet in the parenchyma sectional line, and to avoid right portal vein ligation and liver hilum manipulation, we decided to perform the PPE on the 4th postoperative day. In this paper, we present the first case using this surgical strategy and we propose to name this new procedure “sequential ALTPS”.
Surgical Procedure (Technical Indications and Details)This was a 60-year-old female without associated morbidity (ASA class I); a hypoechoic 13cm mass in the right lobe of liver was diagnosed by ultrasound. CT and MR confirmed that it emerged from the caudate lobe surrounding over 50% of the circumference of the inferior vena cava (IVC), and was occluding the right portal vein posterior branch (Fig. 1). TEP-CT showed SUV at 8.2 without extrahepatic disease. Percutaneous biopsy identified a peripheral cholangiocarcinoma.
Right trisectionectomy plus IVC resection were indicated. Preoperative liver volumetry4 showed a left lateral sector FLR (Future Liver Remnant) of 434ml (23% of TLV–1881ml). We indicated 2-stage surgery with sequential or hybrid ALTPS procedure: tourniquet in the umbilical fissure in the first surgery and PPE on postoperative day 4.
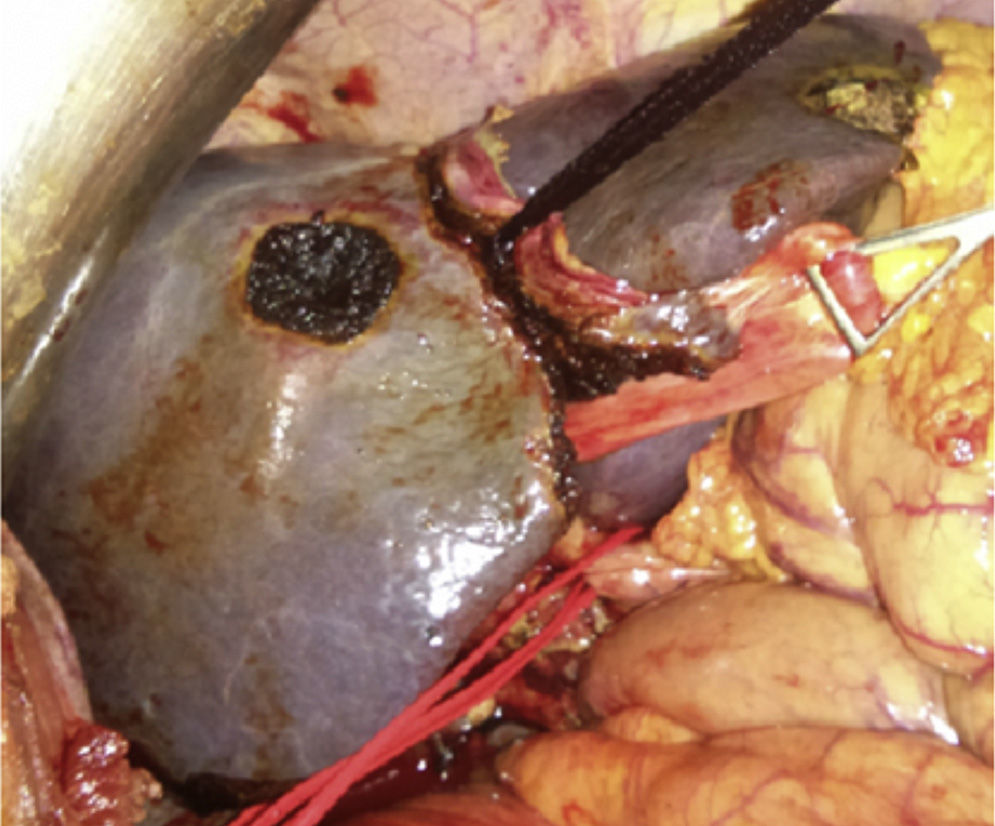
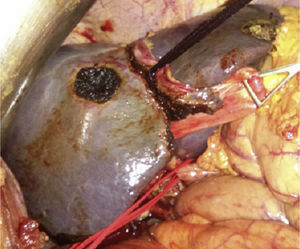
First Surgery (21/12/2012)Bilateral subcostal incision, staging liver and abdominal cavity examination to rule out tumor dissemination, without performing cholecystectomy or examining liver hilum elements. The tourniquet (Vicryl 3mm–V152–Ethicon®) was placed in the umbilical fissure running it from the left and middle suprahepatic veins, continuing through the Rex recess up to the left portal vein pedicle where it was run using the extraglissonian approach. Then, we performed a groove on the right side of the falciform ligament (umbilical fissure) and knotted it, occluding only the parenchyma and intrahepatic collateral branches (Fig. 2). Surgery time was 120min, and blood loss was minimal. In the postoperative period, the patient's prothrombin activity dropped to 80% and GPT increased to 180U/L, which normalized before the PPE.
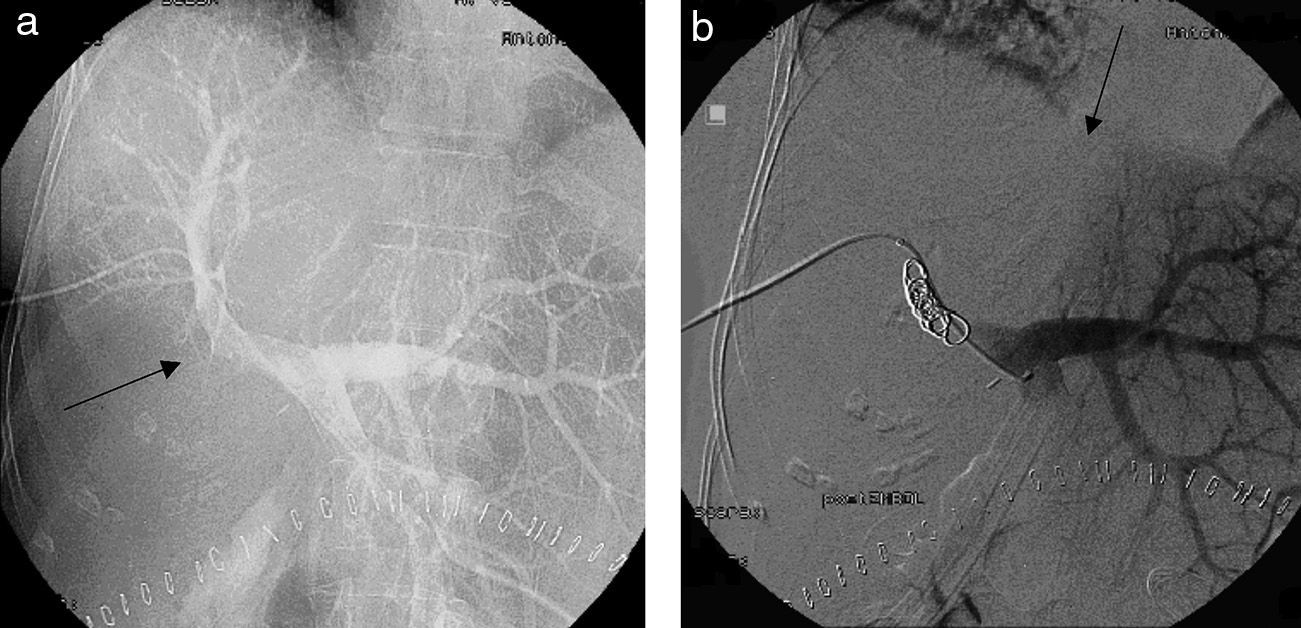
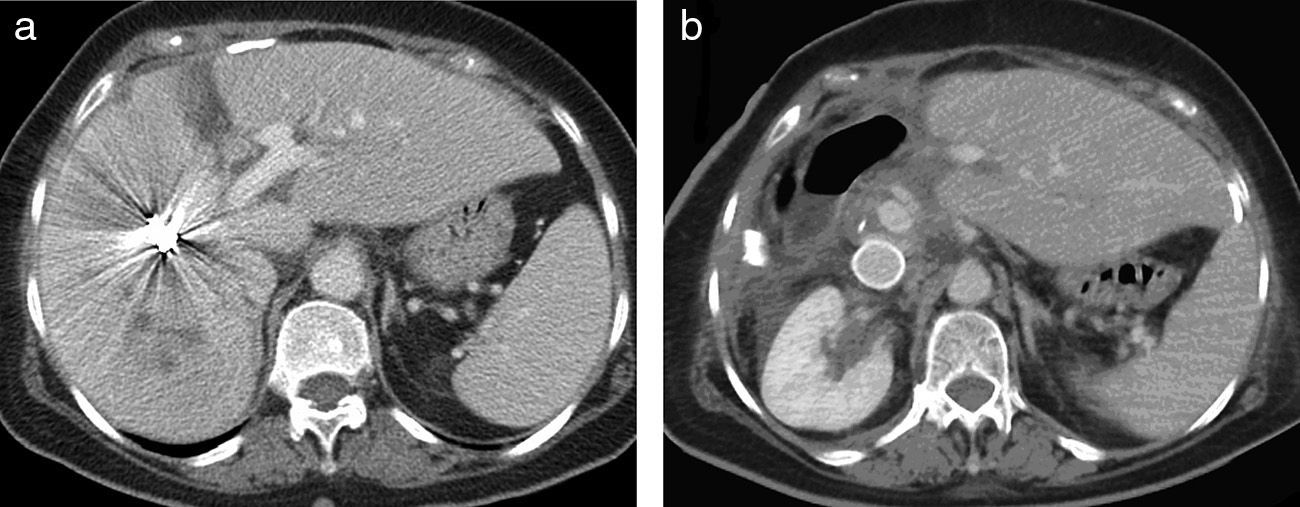
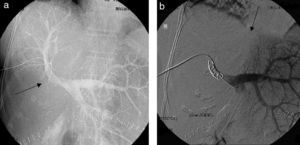
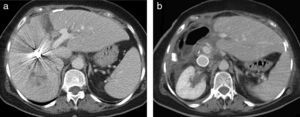
Percutaneous Portal Vein Embolization and Postoperative VolumetryOn postoperative day 4, we conducted a PPE through the anterior branch of the right portal vein; the portography showed right posterior portal vein branch thrombosis (Fig. 3a) and segment IVhypovascularity lacking irrigation from the left portal vein due to parenchyma occlusion from the tourniquet (Fig. 3b). On day 7 after PPE, a new CT was performed; FLR volumetry increased to 769ml (increase of 335ml; 77%), and coils were observed in the right portal vein anterior branch, without collateral circulation through the tourniquet (Fig. 4a).
(a) The percutaneous portal vein embolization on postoperative day 4 (through the right portal vein anterior branch) shows amputation of the portal vein's right posterior branch. (b) Right portal vein anterior branch occlusion with coils and absence of circulation from the left portal vein to the right lobe due to tourniquet's occlusion.
(a) CT on 7th right portal vein post-embolization day shows coils in the portal vein anterior branch and hypertrophy of the anatomical left liver lobe (segments II-III) (77% increase in volume). This is a view of the tourniquet print and absence of vascularization through it (arrow). (b) Control CT at 18 months after surgery shows the Gore-Tex graft in the inferior vena cava and absence of tumor relapse.
The second surgery was performed on day 12 after the first one. The IVC clamping test was haemodynamically tolerated. We performed a hilar lymphadenectomy and ligation of the right liver artery, right portal vein and artery branches of segment IV. Liver partition was conducted in situ through the umbilical fissure, with ligation of the middle hepatic vein, and separation of segments II-III from the right anatomical lobe. We clamped the IVC above the left kidney bifurcation and below the left suprahepatic vein, placing a 2cm diameter by 8cm length ring Gore-Tex graft. IVC occlusion time was 80min; surgery time was 300min, and blood loss was 600ml, without transfusion. During the postoperative period, Quick dropped to 60% and GPT jumped to 340U/L, with normal bilirubin. The patient had a right postoperative chylothorax which was resolved with medical treatment and pleural drainage, and was discharged on postoperative day 11; the last check was performed in May 2014 (Fig. 4b); no disease relapse was detected by CT and tumor markers were normal at 18 months after surgery.
DiscussionPPE was designed to achieve FLR hypertrophy and perform liver resection in one surgery.20 We have described 2-stage liver resection,21 either combined or not combined with intra-operative portal vein ligation. Due to the fact that PPE achieves greater hypertrophy than portal vein ligation, in 2004, Jaeck et al.22 conducted a 2-stage liver resection using PPE at day 4–7 after the initial surgery. An adverse effect of portal vein ligation and PPE is tumor progression,1–6,23 which is related to extended regeneration time. ALPPS or ALTPS procedures achieve greater and faster regeneration, and resectability increases when compared to classic procedures24; therefore, the general thought was that, with such short regeneration time, there would be no tumor progression to contraindicate the second surgery. For tumors proximal to or invading the liver hilum, it is essential to maintain the “non-touch”24,25 principle (Klatskin tumor, giant peripheral cholangiocarcinoma, hepatic carcinoma, metastasis, etc.). By using our ALTPS procedure, we did not manipulate the liver parenchyma since we only placed the tourniquet in the umbilical fissure. For these perihilar tumor cases, we considered intra-operative portal vein ligation contraindicated; therefore, we decided to postpone portal vein occlusion to perform a PPE on postoperative day 4. Postoperative PPE efficacy in 2-stage liver resections had already been demonstrated by Jaeck et al.,22 and recently in those patients where PPE failed, it has been demonstrated that a bipartition (ALPPS salvador) achieves sufficient hypertrophy to conduct the major liver resection.26,27 In a multicentre study on 170 patients with portal vein ligation and PPE, ALPPS was used in 3 patients with failed preoperative PPE, resulting in sufficient RFV hypertrophy to achieve R0 resection.27
Our new hybrid or sequential ALTPS method (tourniquet in the first surgery stage and PPE on postoperative day 4) allowed this patient to achieve sufficient hypertrophy (77%) to perform the second surgery stage at 12 days, and in compliance with the “non-touch” standard; our patient was disease-free at 18 months from surgery. This method can be applied by using the ALPPS procedure, although bipartition proximal to the liver hilum should be avoided, as it does not meet the “non-touch” standard.
Another possible advantage of this method would be achieving postoperative liver function. The classical procedures (portal vein ligation, PPE) involve left lobe congestion; however, due to intrahepatic circulation between the two lobes, no lesions exist from excessive blood flow; yet, in turn, they entail a prolonged regeneration period and less hypertrophy than ALPPS. When ALPPS or ALTPS is performed, given that the right portal vein is ligated and intrahepatic collateral circulation is occluded, excessive blood flow is conditioned toward the left lobe, which, unable to exit through collateral vessels, leads to liver congestion and intrahepatic portal vein hypertension; this has been related to postoperative liver impairment and even small-for-size syndrome.28 In fact, some ALPPS case series report patients with liver failure,10–14 which also occurred in 2 patients in our series with ALTPS.19 In our new modified ALTPS method described herein, increased vein circulation toward the left lobe is performed sequentially, which may benefit liver function. Prospective clinical studies and/or experimental studies are needed to confirm this fact.
One of the complications of the ALPPS procedure is liver segment IV necrosis10–14 due to ischemia resulting from sectioning segment IV branches in addition to the right portal vein. With the sequential or hybrid method, we had no segment IV necrosis; therefore, we considered that necrosis could be avoided with this new method since irrigation of the aforementioned segment would be kept by the right portal vein and by hilar branches from the portal vein bifurcation.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Robles Campos R, Brusadin R, López Conesa A, Parrilla Paricio P. Resección en 2 tiempos de tumores hepáticos perihiliares con torniquete en la cisura umbilical y embolización portal secuencial al cuarto día postoperatorio (ALTPS modificado). Cir Esp. 2014;92:682–686.