Paragangliomas are very uncommon, highly vascularised neuroendocrine tumours that originate in the extraadrenal chromaffin cells. A mediastinal location is rare, and they are rarely functional (catecholamine secretion).1,2 The treatment of choice is surgical resection, and the definitive diagnosis is postoperative in most cases. We present the exceptional case of a functional anterior–superior mediastinal paraganglioma (MP) treated with scheduled complete resection after a pathologic diagnosis by surgical biopsies obtained by prior mediastinoscopy without incident.
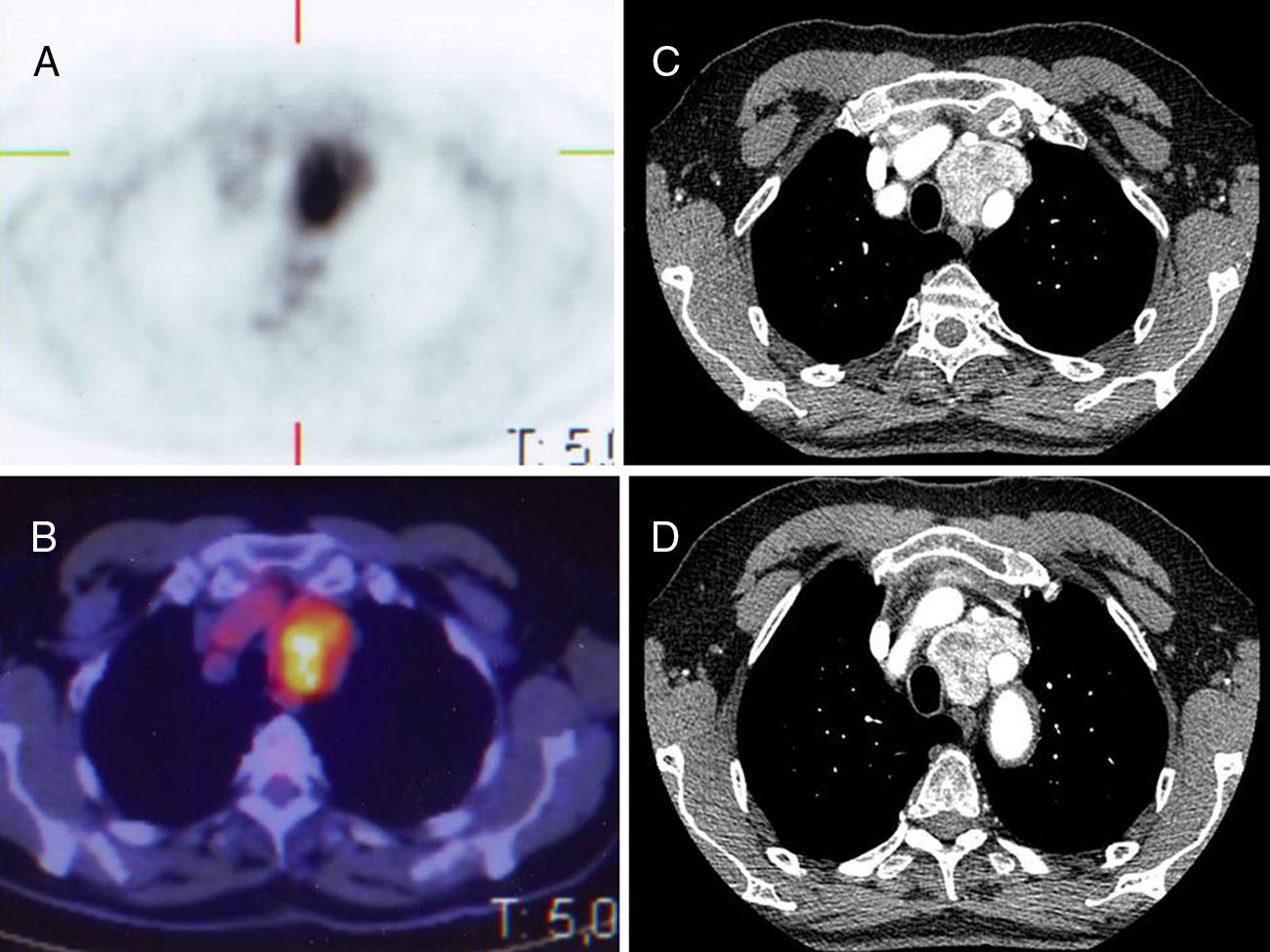
We present the case of a 74-year-old male with a history of sigmoid adenocarcinoma resection, and arterial hypertension; he was an active smoker and presented no other symptoms. Two years after surgery, a follow-up study with thoracoabdominal computed tomography (CT) detected a 45mm mass in the anterosuperior mediastinum. This incidental finding was not infiltrating neighbouring structures and was suspected to be either a teratoma, thymoma or lymphoma. Magnetic resonance imaging (MRI) provided no further information, and positron emission tomography/computed tomography (PET/CT) (Fig. 1A and B; CT Fig. 1C and D) revealed a mediastinal hypermetabolic mass.
Considering these possibilities, diagnostic video-assisted mediastinoscopy was used, during which several biopsies were taken of the mass without incident. The intraoperative result of paraganglioma was confirmed with immunohistochemistry (positive for chromogranin, synaptophysin and S-100 protein).
Endocrinology requested 123I-metaiodobenzylguanidine (123I-MIBG) scintigraphy, which showed a mediastinal focus with increased uptake. Catecholamine and metabolite studies in urine demonstrated elevated levels of metanephrine, normetanephrine, total metanephrine and vanillylmandelic acid, compatible with autonomous catecholamine secretion. With the diagnosis of functional paraganglioma, resection was considered after preoperative preparation with alpha and beta blockers.
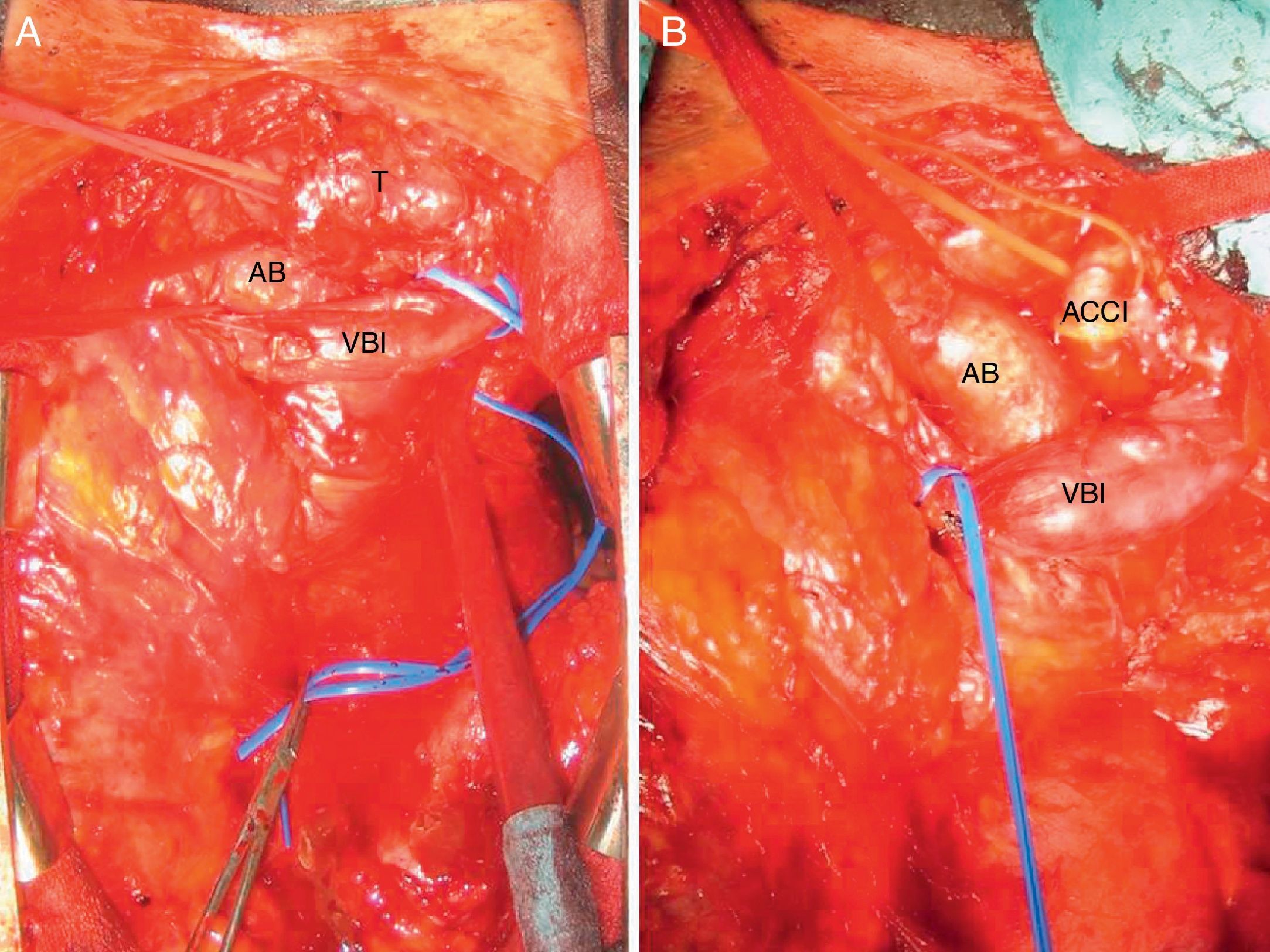
Median sternotomy was performed with complete resection of the tumour, which was elastic in consistency and situated between the innominate vein, brachiocephalic artery, left subclavian and carotid arteries, aortic arch and trachea. Dissection was meticulous in order to avoid bleeding or injury to the recurrent nerve (Fig. 2A and B); there were no haemorrhagic complications and the patient was discharged 6 days after surgery. The pathology report confirmed an encapsulated, multilobulated paraganglioma measuring 5×3.5×3cm. Two weeks after surgery, catecholamine metabolites in urine were normal. Two years later, the patient continues to be asymptomatic, tumour-free and hypertensive.
Paragangliomas are neuroendocrine tumours originating in the extraadrenal chromaffin cells. They are considered functional when there is documented catecholamine hypersecretion, which occurs in 20%.1 Only 2% of paragangliomas are mediastinal,3 usually situated in the anterosuperior mediastinum (aorticopulmonary paragangliomas) or in the posterior mediastinum (aorticosympathetic paragangliomas).2 They can be multi-centred, part of familial syndromes, associated with other neoplasms or malignant in 10%–26% of cases.1–4
The diagnosis of MP is based on symptoms, imaging tests and lab work (functional); the finding is incidental in more than 50% of cases.1,2,5 In symptomatic cases, functional MP should be suspected when there are symptoms related with the excessive production of catecholamines (hypertension, tachycardia, palpitations, syncope, headache, etc.); in non-secretory cases, symptoms are predominantly derived from the compression of adjacent structures (chest pain, dysphagia, dyspnoea, dysphonia, etc.).
For localisation, CT and MRI are used. In functional cases, I-MIBG scintigraphy is used to locate multiple paragangliomas, and PET/CT is used to investigate metastatic disease.1,2
The definitive diagnosis is almost exclusively postoperative and determined by the pathology study. Even if suspected, diagnosis by aspiration cytology is dificult4 and biopsy should be avoided due to the risk of haemorrhage.2,4
The case described was an incidental finding on imaging tests. The diagnosis was reached by surgical biopsy using mediastinoscopy (which entailed the risk of massive bleeding2) because MP had not been included in the differential diagnosis of the mediastinal mass.
The treatment of choice for MP is complete surgical resection2–6 after preoperative preparation by a multidisciplinary team. The option of embolisation may be considered to diminish perioperative bleeding, although it is more often used in paragangliomas of the neck and carotid, or voluminous or posterior MP with expected difficulties for surgical exposure.3,7,8 Imaging tests are used to define the surgical approach, which depends on the location and vascular relationships; and cardiopulmonary bypass is occasionally required.
The main risks of surgery are severe intraoperative bleeding, described in both diagnostic surgery2 and resection,3,4 as well as those related with the release into the blood of vasoactive substances due to the manipulation of the tumour.2,5
After resection, the normalisation of urine catecholamine levels should be confirmed, which usually occurs 1 or 2 weeks after surgery.1 Hypertension, however, continues in many cases.3 Long-term postoperative follow-up is essential for the early detection of metastatic disease, tumour recurrence or later appearance of multiple primary tumours.2
Prognosis after complete resection is favourable, with high long-term survival rates.3,6
In conclusion, mediastinal paragangliomas are very rare hypervascularised tumours, and even more so when functional. Nevertheless, they should be included in the differential diagnosis of mediastinal tumours to avoid haemorrhagic accidents in diagnostic or therapeutic procedures. The treatment of choice is complete resection, which provides a good prognosis when achieved.
Please cite this article as: Ruiz-Zafra J, Sevilla-López S, Bayarri-Lara C. Resección quirúrgica de paraganglioma funcionante diagnosticado por mediastinoscopia. Cir Esp. 2015;93:e97–e99.