The primary hyperparathyroidism is a frequent disease whom the surgery is the only curative treatment. The preoperative location imaging techniques could help in the surgical management. Our objective was to analyze surgical results regarding the cure rate, etiology and location of the glands responsible for the primary hyperparathyroidism in patients with negative preoperative 99mTc-sestamibi scintigraphy.
MethodsObservational study in patients with the diagnosis of primary sporadic hyperparathyroidism with negative 99mTc-sestamibi scintigraphy, operated consecutively in an endocrine surgery unit for 18 years. The cure rate, the intraoperatory PTH, the etiology and the pathological glands location were analyzed.
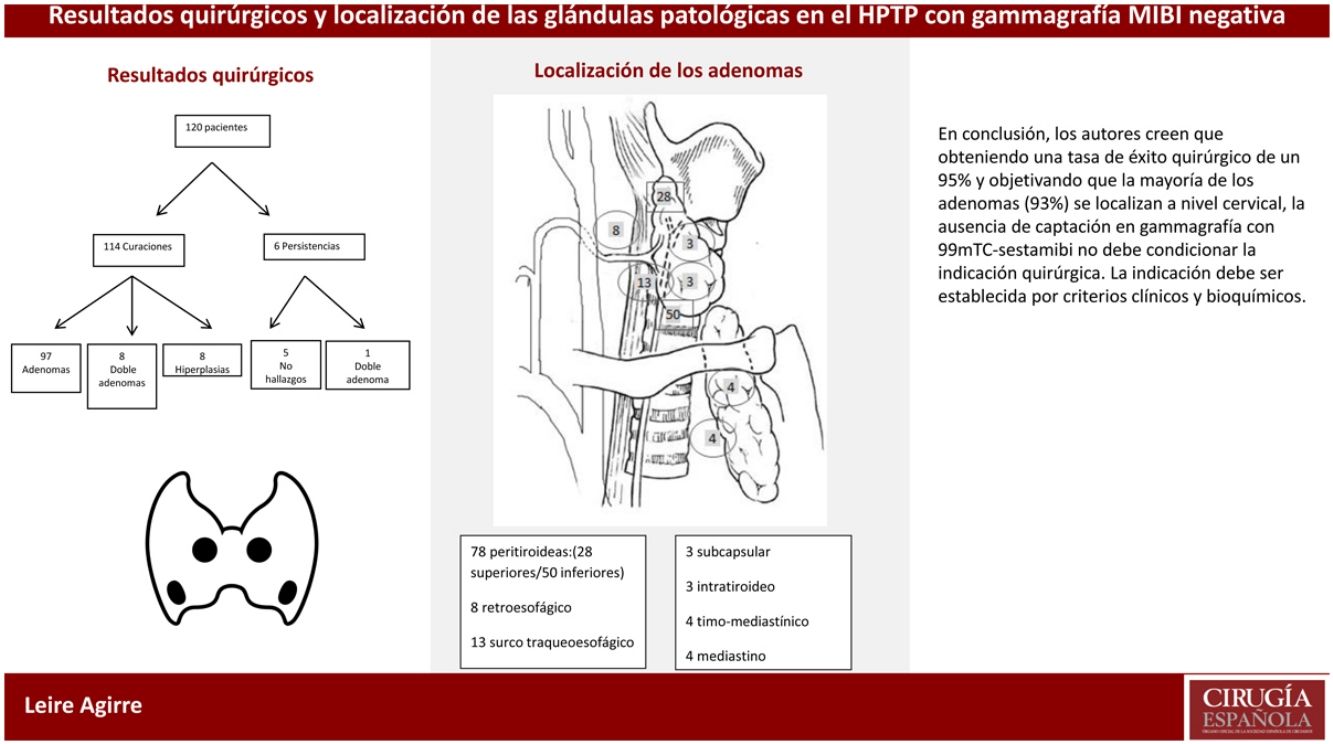
ResultsIn the study were included 120 patients. After surgery 95% of patients (n = 114) presented cure criteria of hyperparathyroidism. 14.1% presented a multigland disease. 69% of the adenomas presented a typical perithyroid location, founding a percentage of 23.9% of ectopic adenomas in cervical location and a 7.1% in mediastinum.
ConclusionsThe absence of uptake in the 99mTc-sestamibi scintigraphy should not condition the surgical indication. The success with experienced surgeons is similar to patients with positive results. The surgical indication must be established by clinical and biochemistry criteria.
El hiperparatiroidismo primario es una enfermedad endocrina frecuente siendo la cirugía el único tratamiento curativo. La técnica quirúrgica puede estar condicionada por las pruebas de localización preoperatorias. Nuestro objetivo ha sido analizar los resultados quirúrgicos en cuanto a la tasa de curación, etiología y localización de las glándulas responsables del hiperparatiroidismo primario en pacientes con gammagrafía con 99mTc-sestamibi preoperatoria negativa.
MétodosEstudio observacional en pacientes con diagnóstico de hiperparatiroidismo primario esporádico con gammagrafía 99mTc-sestamibi negativa operados de forma consecutiva en una unidad de cirugía endocrina durante 18 años. Se analizaron las tasas de curación, la PTH intraoperatoria (PTHio), etiología y la localización de las glándulas patológicas.
ResultadosEn el estudio se incluyeron 120 pacientes. Tras la cirugía el 95% (n = 114) presentaron criterios de curación de hiperparatiroidismo. El 14.1% presentaba una enfermedad multiglandular. Respecto a la localización de los adenomas el 69% presentaban una localización peritiroidea habitual, objetivando un 23.9% de ectopias que se localizan a nivel cervical y un 7.1% de localización mediastínica.
ConclusionesLa ausencia de captación en gammagrafía con 99mTc-sestamibi no debe condicionar la indicación quirúrgica, ya que en manos expertas el porcentaje de éxito es similar a los pacientes con la prueba positiva. La indicación debe ser establecida por criterios clínicos y bioquímicos.
Primary hyperparathyroidism (PHPT) is a common endocrine disease that is the third most common endocrine disorder1 after diabetes and thyroid disease. The diagnosis of this disease is established based on serum calcium and parathyroid hormone (PTH) levels2. Surgery is the only curative treatment for this disease1.
In the last two decades, thanks to the advancement of preoperative localization tests, parathyroid surgery has undergone changes that have resulted in the development of minimally invasive surgical techniques. Currently, scintigraphy continues to be one of the most frequently used tools to locate adenomas, and its sensitivity and specificity increase when performed with 99mTc-sestamibi using the SPECT technique. Unfortunately, the efficacy of this test for the diagnosis of multiglandular disease is limited, so many authors recommend combining different diagnostic methods, such as scintigraphy and ultrasound. Other imaging techniques, such as CT, 4D CT, MRI and especially PET/CT with radiotracers (11C-methionine or 18F-choline) provide good results, particularly in cases that have not been located by scintigraphy and ultrasound3,4, although not all hospitals have this technique available.
The absence of preoperative localization may raise doubts about the appropriateness of the surgical indication. However, preoperative localization is not mandatory to establish the surgical indication in this pathology since the surgical treatment of PHPT that is not located preoperatively could have a high success rate in the hands of expert surgeons.
The objective of this study is to report the surgical results, in terms of the cure rate, etiology and location of the glands responsible for primary hyperparathyroidism in patients with negative preoperative 99mTc-sestamibi scintigraphy.
MethodsThis retrospective, observational, non-randomized study was conducted by the Endocrine Surgery Unit of a tertiary level medical center. The study included patients treated surgically from September 2000 to July 2018 with a diagnosis of sporadic PHPT that had not been located preoperatively. The exclusion criteria were the following: history of thyroid or parathyroid surgery and patients with primary hyperparathyroidism in the context of multiple endocrine neoplasm (MEN). All patients underwent preoperative 99mTc-sestamibi scintigraphy and cervical ultrasound.
A descriptive analysis was conducted of the patients included in the study regarding cure rate, intraoperative PTH (ioPTH), etiology and location of the pathological glands. The quantitative variables are presented as mean value plus standard deviation, and for analytical values the range of values is presented.
Patients were followed for a minimum of 18 months. ‘Cure’ was defined as serum calcium levels within normal limits for at least six months after the intervention. ‘Persistence’ was defined as hypercalcemia being found within the first six postoperative months, and ‘recurrence’ was defined as a new elevation of serum calcium starting at least six months after surgery.
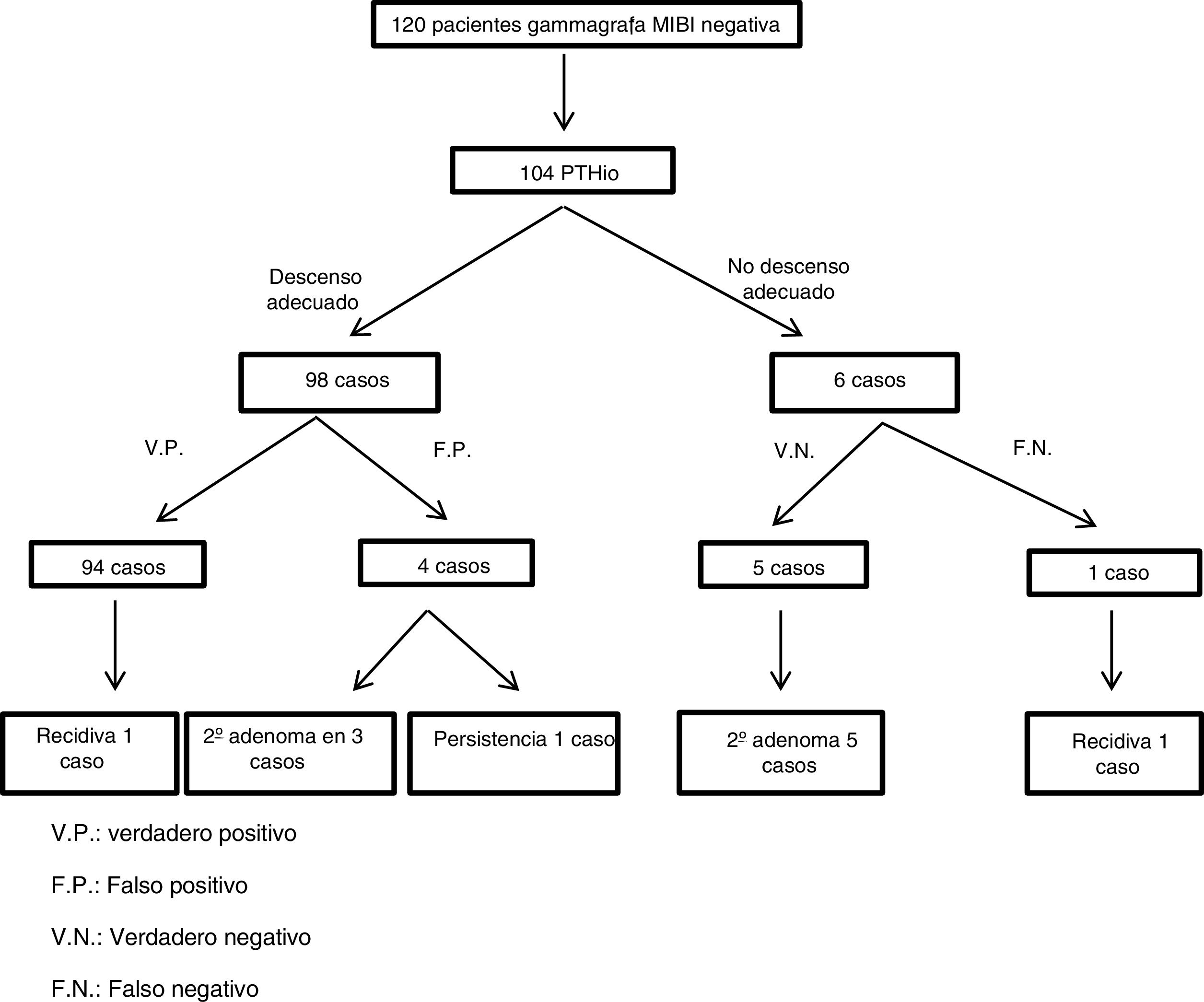
We followed the Position Statement of the European Society of Endocrine Surgeons (ESES), which recommends the use of ioPTH in patients with negative or non-concordant localization tests.5 In accordance with the Miami Criteria, ioPTH was considered curative when ioPTH decreased ≥50% 10 min after resection of the pathological gland versus the highest PTH concentration of the two samples obtained previously (baseline PTH and pre-resection). True positives were identified by a correct drop in ioPTH, and clinical cure was achieved after resection of the adenoma; false positives were identified by an adequate drop in ioPTH, although the disease persisted; false negative when ioPTH did not fall sufficiently, without observing another pathological gland, in a patient with clinical cure; and in true negatives the ioPTH did not decrease because there was multiglandular disease.
ResultsOut of the 726 patients operated on for sporadic primary hyperparathyroidism, in 123 the preoperative MIBI scintigraphy was negative, while 3 patients were excluded due to previous thyroid (2) or parathyroid (1) surgery.
In the group of patients without preoperative localization, the median age was 59 years (range 14–80 years), and they were predominantly women (74%). The patients had a preoperative median calcium level of 11.4 mg/dL (range 10.6–16.3 mg/dL) and a serum PTH of 154.5 pg/dL (range 77−1679 pg/dL).
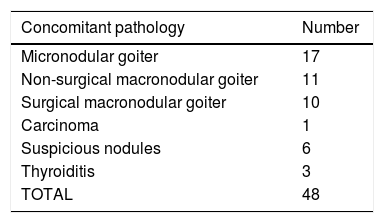
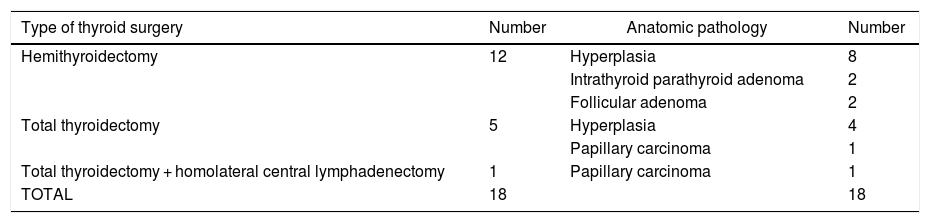
Concomitant thyroid disease was found in 40% of the cases (48 patients; Table 1), 18 of which required thyroid surgery during the same operation (Table 2).
Thyroid surgery performed and corresponding pathology result.
| Type of thyroid surgery | Number | Anatomic pathology | Number |
|---|---|---|---|
| Hemithyroidectomy | 12 | Hyperplasia | 8 |
| Intrathyroid parathyroid adenoma | 2 | ||
| Follicular adenoma | 2 | ||
| Total thyroidectomy | 5 | Hyperplasia | 4 |
| Papillary carcinoma | 1 | ||
| Total thyroidectomy + homolateral central lymphadenectomy | 1 | Papillary carcinoma | 1 |
| TOTAL | 18 | 18 |
Bilateral cervical exploration was performed in all patients, and no pathological gland was found in 5 (4.2%).
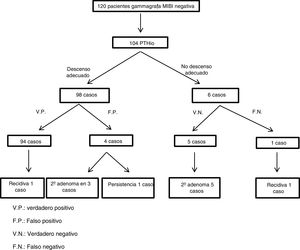
Intraoperative PTH monitoring was performed in 104 patients after removal of an adenoma, and 94 were considered true positives, although one patient had a recurrence at 29.5 months. In 4 patients, the result was false positive, since, despite the adequate decrease in ioPTH, in 3 cases a second adenoma was observed in the same operation and the 4th resulted in persistence. In 6 cases, ioPTH did not drop after removal of the adenoma; a second adenoma was found, and an adequate decrease in PTH was achieved after removal in 5 patients. In the 6th patient, a second adenoma was not observed; the patient’s calcium levels remained normal until recurrence was observed 23 months (Fig. 1). Intraoperative PTH was not performed in 16 patients; in 8 cases, this was due to observed multiglandular disease, in 5 cases because no pathological gland was found, and in 3 patients due to logistical problems.
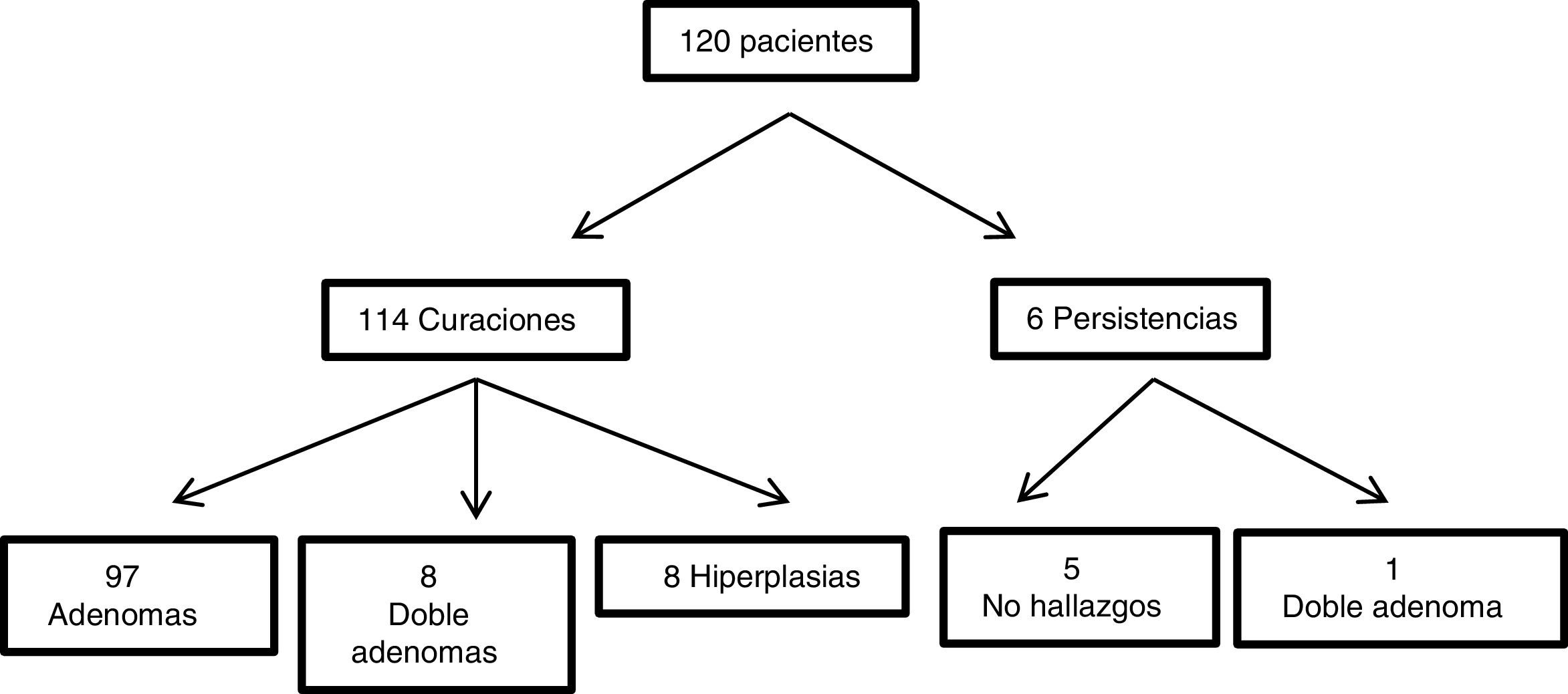
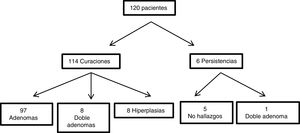
Regarding surgical success, 114 of the 120 patients were clinically cured six months after surgery (95% of cases). Persistence was observed in 6 patients; 5 were failures due to not finding pathological glands during surgery, but the 6th was a double adenoma not noticed during the first intervention. Two of the 114 patients had recurrence after 23 and 29.5 months, respectively.
When we analyzed the pathological anatomy/etiology of the PHPT that had not been located preoperatively, in the group in which a clinical cure was achieved (114 patients), 97 cases were single adenomas, 8 double adenomas, 8 hyperplasia and one carcinoma. Regarding the 6 cases with persistence, one case was due to a double adenoma that was successfully reoperated, and out of the 5 in which no pathology was found in the first surgery, in one a single intrathyroid adenoma was removed 4 years later and in another a mediastinal adenoma in the aortopulmonary window seven years later; the remainder have not been located or reoperated. A total of 10 normal parathyroid glands were removed (Fig. 2).
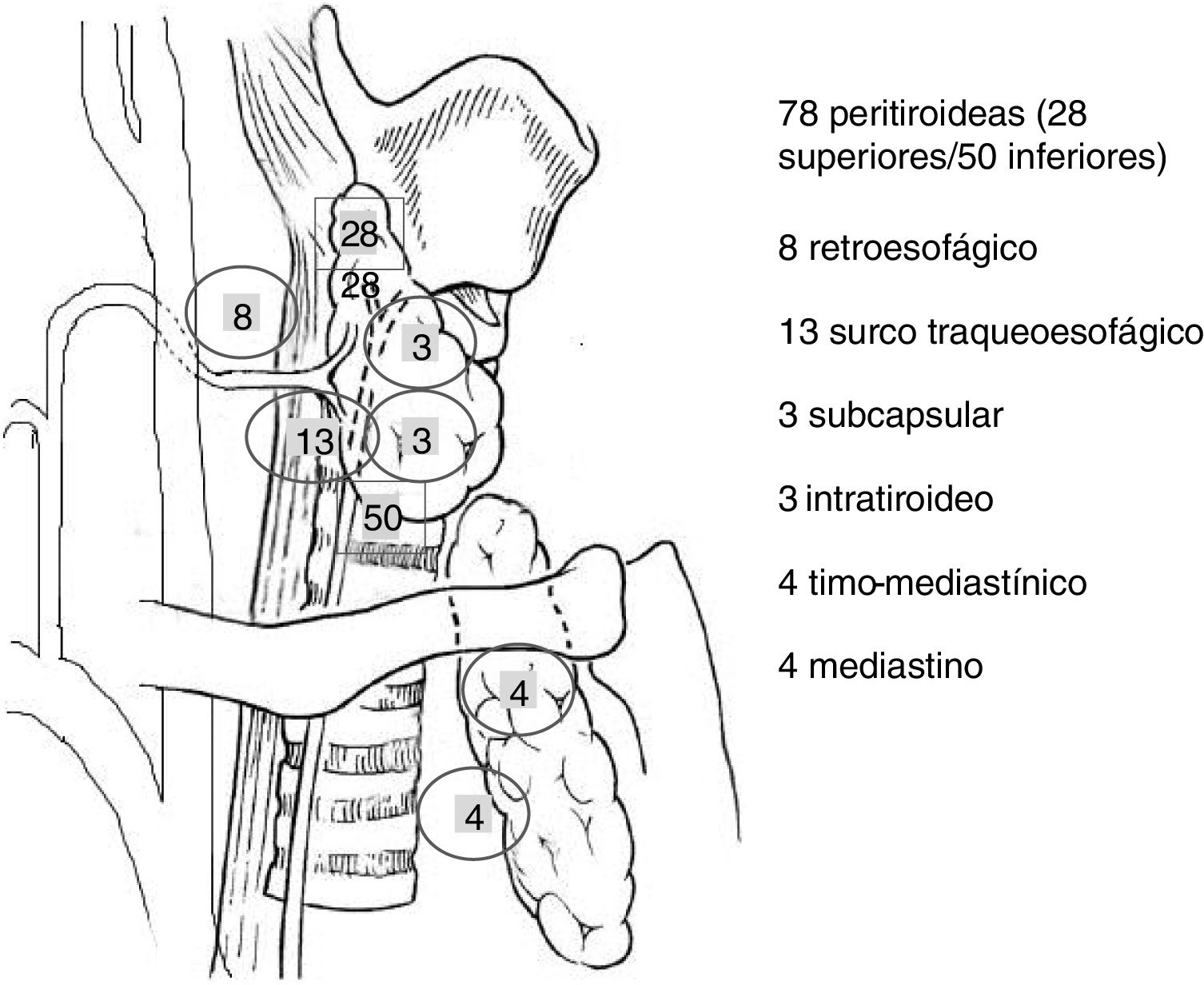
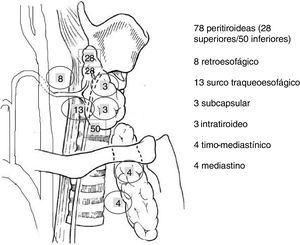
When we examined the location of the single and double adenomas in this study (113), we observed that the majority (78 cases; 69%), had a perithyroid location. When we analyzed the ectopias (31% of the cases), most (23.9%) were located at the cervical level (13 cases tracheoesophageal groove, 8 retroesophageal, 3 intrathyroid and 3 subcapsular) and only 7.1% in the mediastinum (four cases in the mediastinal thymus and four in the superior mediastinum). All of them were able to be resected cervically (Fig. 3).
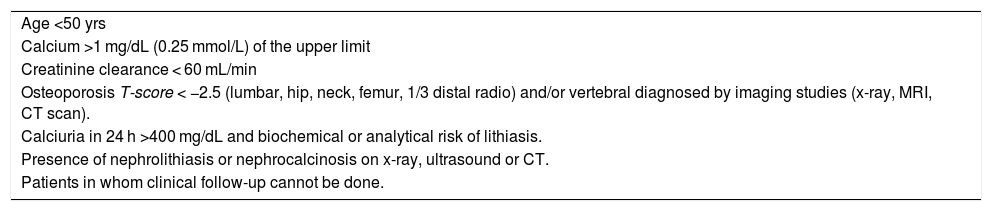
DiscussionThe surgical indication for PHPT is established by symptoms, as well as in asymptomatic patients when certain criteria are met6,7 (Table 3).
Criteria for surgical indication in asymptomatic patients.
| Age <50 yrs |
| Calcium >1 mg/dL (0.25 mmol/L) of the upper limit |
| Creatinine clearance < 60 mL/min |
| Osteoporosis T-score < −2.5 (lumbar, hip, neck, femur, 1/3 distal radio) and/or vertebral diagnosed by imaging studies (x-ray, MRI, CT scan). |
| Calciuria in 24 h >400 mg/dL and biochemical or analytical risk of lithiasis. |
| Presence of nephrolithiasis or nephrocalcinosis on x-ray, ultrasound or CT. |
| Patients in whom clinical follow-up cannot be done. |
Therefore, preoperative localization tests should not be considered a criterion to indicate surgical intervention, although they do facilitate the performance of minimally invasive surgical techniques, reducing the morbidity associated with bilateral cervical exploration.
However, the reality is that the result of the parathyroid scintigraphy can influence the management of these patients. The Susana Wu et al. study8 found that negative sestamibi influences decision-making in the treatment of patients with primary hyperparathyroidism. According to this study, endocrinologists referred fewer patients to surgeons, and surgeons were less inclined to perform parathyroidectomy on these patients.
Parathyroid scintigraphy has a localization rate that ranges from 80%–100% in the literature, which becomes higher when combined with single-photon emission computed tomography (SPECT; 85%–95%) than with conventional planar projection (75%–85%)9–11. For this reason, until now, 99mTc-MIBI SPECT was considered the gold standard as a preoperative localization test. Several factors are responsible for the negative result of sestamibi: the nature of the parathyroid gland itself, histology shows a predominance of the main cells, multiglandular disease or ectopic glands, the smaller size of the adenoma and the presence of concomitant thyroid nodules12–14. Patient-dependent factors, such as obesity, may also contribute to this result14.
In recent years, different PET/CT studies with 18F-fluorocholine have shown higher levels of detection of parathyroid adenomas compared to 99mTc-MIBI SPECT, reducing the need for bilateral cervical explorations. However, not all hospitals have this technique available. Some authors recommend its use in those patients in whom it has not been possible to locate the hyperfunctioning adenoma with conventional screening tests, thus increasing the number of patients who could benefit from minimally invasive surgery4,15,16.
Historically, before the introduction of the preoperative imaging techniques described, the cure rate after parathyroidectomy was 95%17. However, in the literature this figure may vary among the different studies.
In the United States, most patients with endocrine pathology are operated on by surgeons who treat a small volume of patients. Stavrakis et al.18 found that 65% of surgeons who perform thyroid, parathyroid, or adrenal gland surgery in New York or Florida perform one to 3 procedures per year. This could explain the variability of the cure rates among the different studies. For this reason, we should emphasize, as John Doppman did at the Consensus Development Conference in 1990, that “…the only localization that a patient needs who has primary hyperparathyroidism is the localization of an experienced surgeon”17,19,20.
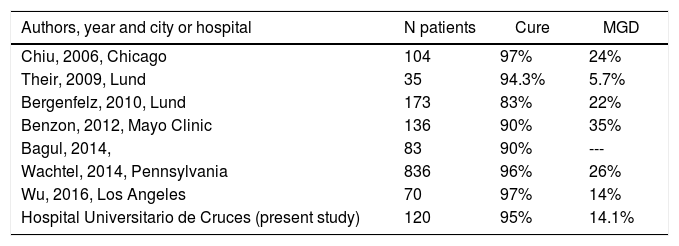
In this study, the cure rate after the first surgical intervention was 95%. In the literature, there are studies with variable results regarding surgical success in patients with PHPT that are not located preoperatively, ranging from 83% to 97% (Table 4)1,8,19,21–24. Despite the differences between the various studies, cure rates remain high.
Cure rates and multiglandular disease rates according by publications.
| Authors, year and city or hospital | N patients | Cure | MGD |
|---|---|---|---|
| Chiu, 2006, Chicago | 104 | 97% | 24% |
| Their, 2009, Lund | 35 | 94.3% | 5.7% |
| Bergenfelz, 2010, Lund | 173 | 83% | 22% |
| Benzon, 2012, Mayo Clinic | 136 | 90% | 35% |
| Bagul, 2014, | 83 | 90% | --- |
| Wachtel, 2014, Pennsylvania | 836 | 96% | 26% |
| Wu, 2016, Los Angeles | 70 | 97% | 14% |
| Hospital Universitario de Cruces (present study) | 120 | 95% | 14.1% |
MGD: multiglandular disease.
In PHPT, multiglandular disease can vary between 3% and 24% depending on the series25–28. In patients with negative sestamibi, this percentage is higher (between 5.7% and 35%) (Table 4)8,19,21–24. In this study, the results are in range compared to the literature: 84.3% single adenomas and 14.7% multiglandular disease.
The authors believe that this variability regarding the incidence of multiglandular disease may be due to the resection of histologically normal parathyroid glands, which could appear pathological when observed macroscopically during surgery. In this series, 10 parathyroid glands were removed, which were defined as multiglandular disease in the surgical protocol but were reclassified after the pathological analysis as single adenomas with inadequate resection of normal glands. We have not found this datum reported in the literature.
According to the meta-analysis by Dominik Taterra et al.29 that included 7005 patients, the parathyroid glands present an ectopic location in 15.9%, 11.6% of which are located in the neck and 4.3% in the mediastinum. The authors have not found in the literature any reference to the anatomical location of adenomas, with negative preoperative localization tests.
Given that the majority of the adenomas in this study (93%) were located cervically, the authors considered it beneficial to operate on these patients due to the high success rate in the hands of expert surgeons. Another argument in favor of surgery is that pharmacological treatment has few benefits and is less cost-effective than surgery30,31. Early surgery can prevent the long-term sequelae caused by hyperparathyroidism, which is the strategy recommended by the American Association of Clinical Endocrinologists and the American Association of Endocrine Surgeons, with an acceptable percentage of complications32. In the only prospective longitudinal study of conservatively treated PHPT, almost 40% of asymptomatic patients developed a surgical criterion over a 15-year period33.
Given what has been discussed above, the authors agree with Sitges-Serra34 that patients with PHPT without a clear preoperative location should be operated on by specialized surgeons, since parathyroidectomy is the only curative treatment for this pathology, and a high cure rate is obtained by expert hands. We should bear in mind, as indicated in the International Workshop Guidelines13, that “negative or discordant imaging tests should not be an impediment to refer patients to a surgeon experienced in parathyroid surgery.”
In conclusion, the authors believe that obtaining a surgical success rate of 95% and observing that the majority of adenomas (93%) are located at the cervical level, the absence of uptake of 99mTc-sestamibi on scintigraphy should not influence the surgical indication. The indication should be established by clinical and biochemical criteria.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Agirre L, de la Quintana A, Martínez G, Arana A, Servide MJ, Larrea J. Resultados quirúrgicos y localización de las glándulas patológicas en el tratamiento del hiperparatiroidismo primario esporádico con gammagrafía 99mTc-sestamibi negativa. Cir Esp. 2022;100:18–24.