The Fontan procedure (FP) plays a palliative role in complex congenital heart disease with the presence of a functioning single ventricle. FP creates an anastomosis between the systemic venous return and the pulmonary artery to transmit blood to the single ventricular chamber. Currently, and although FP offers a 20-year survival rate over 80%1, hemodynamic changes cause multiple complications as a result of increased systemic venous pressure, which can affect all organs2. Liver disease related to FP is constant and time-dependent; in advanced stages, complications appear as a result of portal hypertension (PHT), hepatocellular carcinoma (HCC) or hepatic encephalopathy.
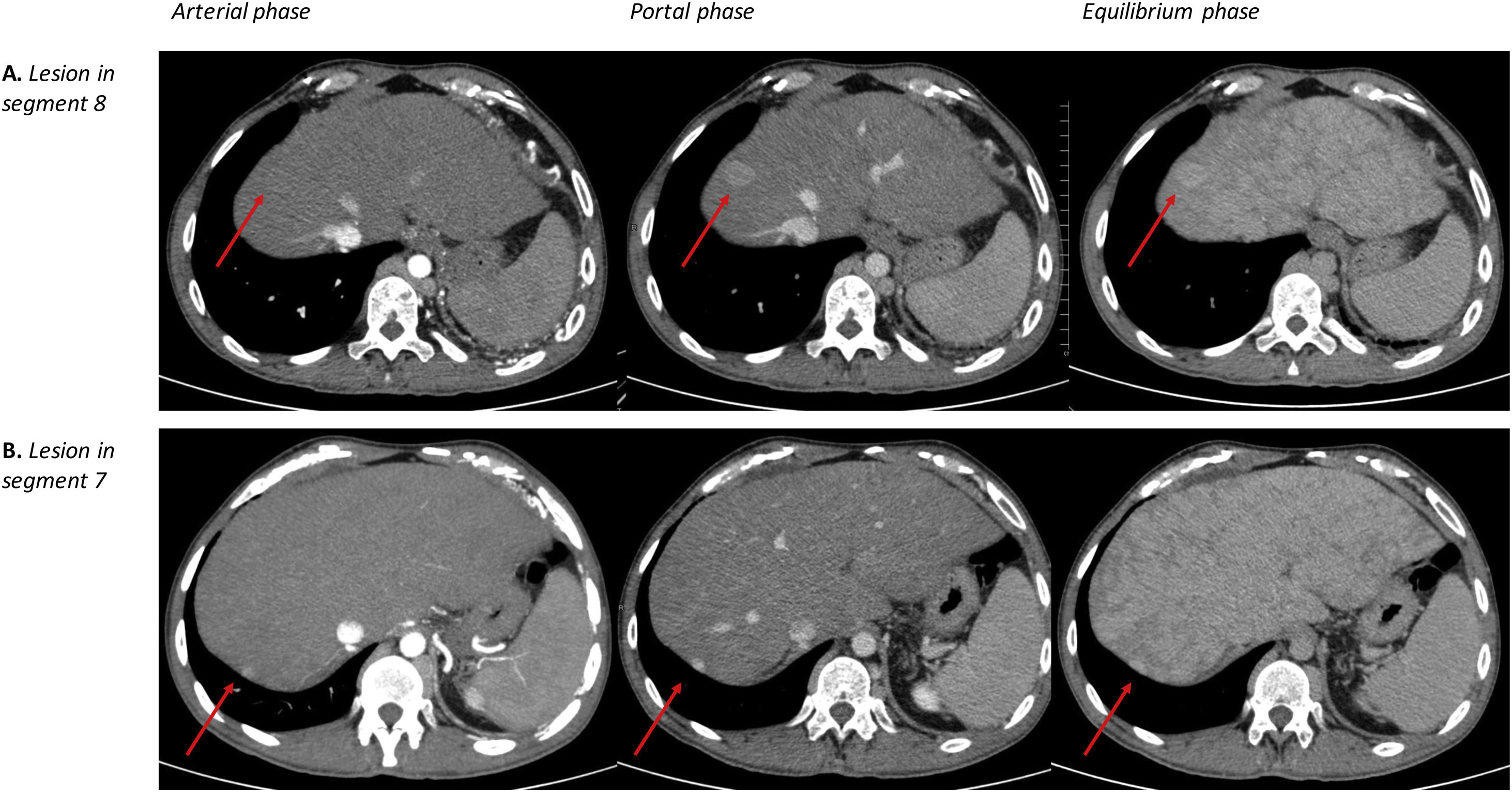
We present the case of a 32-year-old man diagnosed at birth with a congenital heart malformation, consisting of a tricuspid malformation with right ventricular hypoplasia. FP (bicavopulmonary anastomosis with fenestrated atrial conduit) was performed when he was 3 years of age, with subsequent placement of an epicardial pacemaker due to episodes of atrioventricular block. Some 23 years after the FP, an HCC screening program was started by the Gastroenterology Department with ultrasound scans every 6 months, which showed no suspicious liver nodules initially. After 5 years of follow-up, due to a slight increase in alpha-fetoprotein (from 3.74 IU/mL to 7.20 IU/mL), a multiphase Computerized Tomography (CT) scan was conducted, which identified a 30-mm focal lesion in segment (S) 8 that was not clearly hypervascular, hyperdense in the portal phase and isodense in the equilibrium phase. In addition, another 15 mm subcapsular lesion in was observed in S 7, which was hyperdense in the arterial and portal phases and isodense in the equilibrium phase (Fig. 1).
Given the uncertain diagnosis, needle aspiration of both lesions was requested. The pathological study of the S 8 lesion reported well-differentiated hepatocarcinoma, and the S 7 lesion demonstrated liver cirrhosis with no evidence of malignancy. The case was presented to a multidisciplinary committee: hepato-cardiac transplantation was ruled out due to left pulmonary hypoplasia, and percutaneous treatments were also ruled out due to technical impossibility, so surgical resection was proposed. The extension study was completed with cranial CT and bone scintigraphy, finding no distant disease. A hepatic hemodynamic study was performed, which showed a wedged hepatic venous pressure of 24 mmHg and a free pressure of 23 mmHg, reflecting posthepatic portal hypertension. Elastography showed grade F4 fibrosis, and gastroscopy revealed small esophageal varices. The preoperative MELD index was 13 and corresponded to a Child Pugh stage B7. The surgery was planned and performed in a multidisciplinary manner, with the participation of the General Surgery and Digestive System, Cardiac Surgery, Pediatric Cardiology and Anesthesiology departments. Initially, the Cardiac Surgery unit repositioned the epicardial pacemaker located in the right subcostal region, with intra-surgical verification of the electrodes by Pediatric Cardiology. Subsequently, using a right subcostal laparotomy, and after intraoperative ultrasound, we conducted a subsegmental resection of the lesions in S 7 and S 8 with verification of the resection margins and fulguration of the bed with diathermy, resulting in intraoperative bleeding of less than 100cc. The patient was discharged on the 10th postoperative day, presenting mild decompensation of heart failure with good response to diuretic treatment.
The result of the pathological study of both nodules was moderately differentiated HCC, with no vascular invasion, and free margins. The non-tumorous parenchyma showed a markedly congestive cirrhotic pattern. After 12 months of follow-up, the patient continues to be asymptomatic, and no new suspicious lesions have been observed.
Most liver diseases are due to inflammatory damage caused in the periportal areas of the hepatic lobule. In patients with FP, the damage is caused by hepatic congestion that, as in other chronic liver diseases, leads to advanced fibrosis with the complications of portal hypertension, liver failure, and increased risk of HCC. These complications are time-dependent3,4.
Regenerative nodules, as in other congestive liver diseases, are very common in these patients. They are generally large, hypervascular, and located in the hepatic periphery. Some of these features are common to HCC. For this reason, the diagnosis of HCC in patients treated with FP requires biopsy for histological confirmation in most cases5–8.
There are few publications about the management of HCC in patients with FP, and most show a preference of non-surgical approaches (radioembolization, transcatheter arterial chemoembolization, or percutaneous ablation). Surgical resection is proposed as a feasible but limited alternative on many occasions, because of both the cardiac and hepatic functionality6,9. Definitive treatment could involve liver or heart-liver transplantation, which is contraindicated in pulmonary hypoplasia, as in this case.
Specialized patient follow-up is essential, along with the implementation of an HCC screening program after FP. Although the time to initiate screening has not been defined, most tumors appear at least 10 years after FP6. At our hospital, screening is indicated 10 years after FP, which includes a hepatic ultrasound every 6 months.
In cases where percutaneous procedures cannot be performed, surgical resection is a feasible, and potentially curative, alternative (Table 1).
Surgical resection in HCC after FP.
| Main author | Year | Age | Sex | Complications of PHTCirrhosis | Time since FP (years) | Image | AFP | Stage (BCLC, Milan) | Treatment | Survival |
|---|---|---|---|---|---|---|---|---|---|---|
| Payno | 2022 | 32 | M | Complications of PHT: NOCirrhosis: Yes | 28 | 30 mm and 15 mm | 7 ng/mL | BCLC A | Surgical resection | Alive after 12 months |
| Yokota10 | 2020 | 18 | M | Complications of PHT: NOCirrhosis: Yes | 12 | NR | 3 ng/mL | BCLC AMilan: Yes | Laparoscopic resection | Alive after 12 months |
| Nemoto11 | 2020 | 37 | F | Complications of PHT: NOCirrhosis: Yes | 31 | 80 mm | 81.663 ng/mL | BCLC: AMilan: NO | Left hepatectomy | Alive after 16 months |
| Angelico, Int J Surg Case Rep. 59:144−147. | 2019 | 33 | F | Complications of PHT: NOCirrhosis: Yes | 27 | 45 mm | 3.005 ng/mL | BCLC: AMilan: YES | Laparoscopic resection. Recurrence: TACE + Sorafenib | Alive after 7 months |
| Lo,Transl Gastroenterol Hepatol. 3:51. | 2018 | 24 | M | Complications of PHT: NOCirrhosis: Yes | 23 | 68 mm and 27 mm | 50.000 ng/mL | BCLC: BMilan: NO | Left hepatectomy.Recurrence: TACE + Sorafenib | Exitus por cáncer a los 6 months |
| Takuma,Intern Med. 55(22):3265−3272. | 2016 | 29 | F | Complications of PHT: AscitisCirrhosis: Yes | 19 | 18 mm and 15 mm | 117 ng/mL | BCLC: AMilan: YES | Surgical resection | Alive after 12 months |
| Jitta, Int J Cardiol. 206:21−26. | 2016 | 42 | F | Complications of PHT: NOCirrhosis: Yes | 32 | NR | 2.996 ng/mL | BCLC: AMilan: NO | Surgical resection | Alive after 12 months |
| Dorsey, J Cardiothorac Vasc Anesth. 30(2):452−454. | 2016 | 32 | M | Complications of PHT: NOCirrhosis: Yes | 23 | 40 mm | 13 ng/mL | BCLC: AMilan: YES | Surgical resection | Alive after 12 months |
| Maeda, Reg Anesth Pain Med. 40(6):718−719. | 2015 | 12 | M | Complications of PHT: NOCirrhosis: NR | 10 | 12 mm | NR | BCLC: AMilan: YES | Surgical resection | NR |
| Weyker, A A Case Rep. 2(8):99−101. | 2014 | 23 | M | Complications of PHT: NRCirrhosis: NR | 22 | 148 mm | NR | BCLC: CMilan: NO | Surgical resection | NR |
M: male; F: female; PHT: portal hypertension; FP: Fontan procedure; AFP: alfafetoprotein; NR: not reported; TACE: transarterial chemoembolization.
Table modified by Rodriguez-Santiago E, Téllez L, Guerrero A, Albillos A. Hepatocellular carcinoma after Fontan surgery: A systematic review. Hepatol Res. 20216.