Surgery of the biliary tract is complex, and its volume has increased with iatrogenic injuries and living donor transplantation. The aim of this study was to analyze if the common duct can be temporarily replaced. We used nine 18–20kg pigs. They were operated on, and their bile duct was replaced by a 100% silicone tube. All pigs underwent laboratory tests, magnetic resonance imaging, intraoperative ultrasound, cholangiography and biliar manometry with pathological biopsy examination within 60 days from the initial surgery.
All pigs survived the first surgery over 60 days without laboratory evidence of evident cholestasis. Nine pigs were re-operated on at day 60 showing dilated common bile duct and hepatic ducts doubling its original size without dilating the intrahepatic bile ducts. There were no clinical, relevant laboratory or biopsy signs showing cholestasis.
This experience represents the initial intention to find an optimal situation and prosthesis for replacement of the thin biliary tract, in surgical emergencies or palliative situations. The silicon tube is a positive answer that remains permeable. A non-fibrotic reaction was found that allows a posterior definitive procedure, maintaining a good nutritional status.
Las lesiones quirúrgicas de la vía biliar fina, continúan siendo un dilema. Los procedimientos no invasivos requieren la continuidad de la vía biliar para poder colocarse. En este trabajo intentamos comprobar si el reemplazo de la vía biliar por un tubo de silicona, es posible.
A 9 cerdos de 18–20kg se les reemplazó la vía biliar principal por un tubo de 100% silicona. Se les realizó análisis de laboratorio, colangiorresonancia, ecografía, colangiografía y manometría intraoperatorias con examen de anatomía patológica a 60 días de la cirugía inicial.
Los 9 cerdos sobrevivieron a la cirugía de reemplazo de la vía biliar por un tubo de silicona más de 60 días sin evidencia de colestasis significativa por laboratorio. Todos los cerdos fueron reintervenidos, y mostraron dilatación del colédoco y conductos hepáticos duplicando o triplicando por lo menos, su tamaño inicial sin dilatarse el resto de la vía biliar intrahepática, ni presentar signos ni laboratorio significativo de colestasis.
Nuestro estudio puede entenderse como una intención inicial de encontrar la prótesis y la situación ideal para poder reemplazar la vía biliar extrahepática fina, en situación quirúrgica de emergencia o paliativa sin posibilidad de stent. El reemplazo por el tubo de silicona en nuestra experiencia resultó positivo con esta intención, manteniéndose permeable, sin generar fibrosis permitiendo una posterior cirugía definitiva, sin perjudicar el estado nutricional.
The growing volume of bile duct surgeries, which is one of the more complex type of surgery, has resulted in an increasing number of patients with iatrogenesis and living donor transplantation. This increase in bile duct injuries is often attributed to the learning curve involved in laparoscopic surgery. As surgeons, this is a problem that we should be interested in resolving.1–3
Currently, bile duct injuries can only be treated in high-level hospitals by experienced surgeons, with methods that can be either endoscopic or surgical. Neither of these situations are free of complications, however, and most cases require several interventions. Non-invasive endoscopic procedures like dilatation and stent placement can cause unsatisfactory results, such as stent obstruction, cholangitis or recurrent stenosis, and they of course require continuity of the bile duct for placement.1,4 Invasive procedures such as Kehr's T-tube or biliodigestive anastomoses are likewise associated with major perioperative complications and require a larger bile duct to be able to work; in the long term, manipulation of the sphincter of Oddi entails a risk of more enteric reflux toward the bile duct.4 Surgical injury to the thin bile ducts continues to be a dilemma, which is what motivated our research.
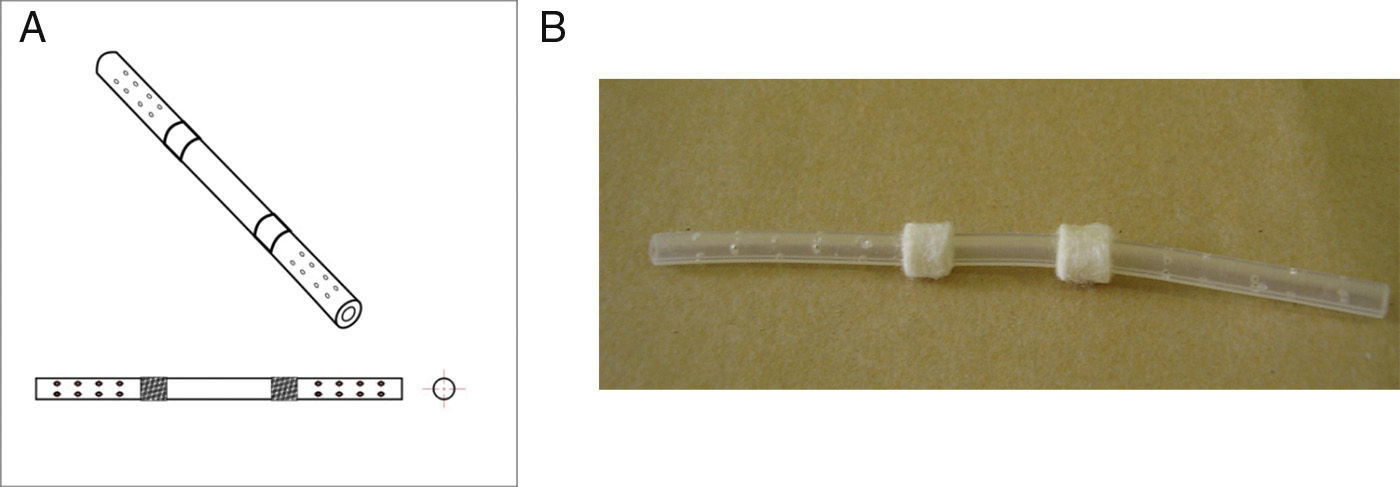
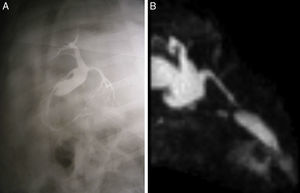
The objective of this experimental study was to determine whether substituting a porcine bile duct (Fig. 1) with a silicone tube (Fig. 2) would lead to perioperative complications and whether their use is a possible option in cases of bile duct obstruction, stenosis or injury.
There have been reports of previous attempts with PTFE tubes,5,6 gallbladder flaps,7 grafts of vascular structures8 and even intestinal mucosa.9 Nonetheless, these reports have shown incomplete or unsatisfactory results, and these techniques have therefore not been integrated into daily practice.
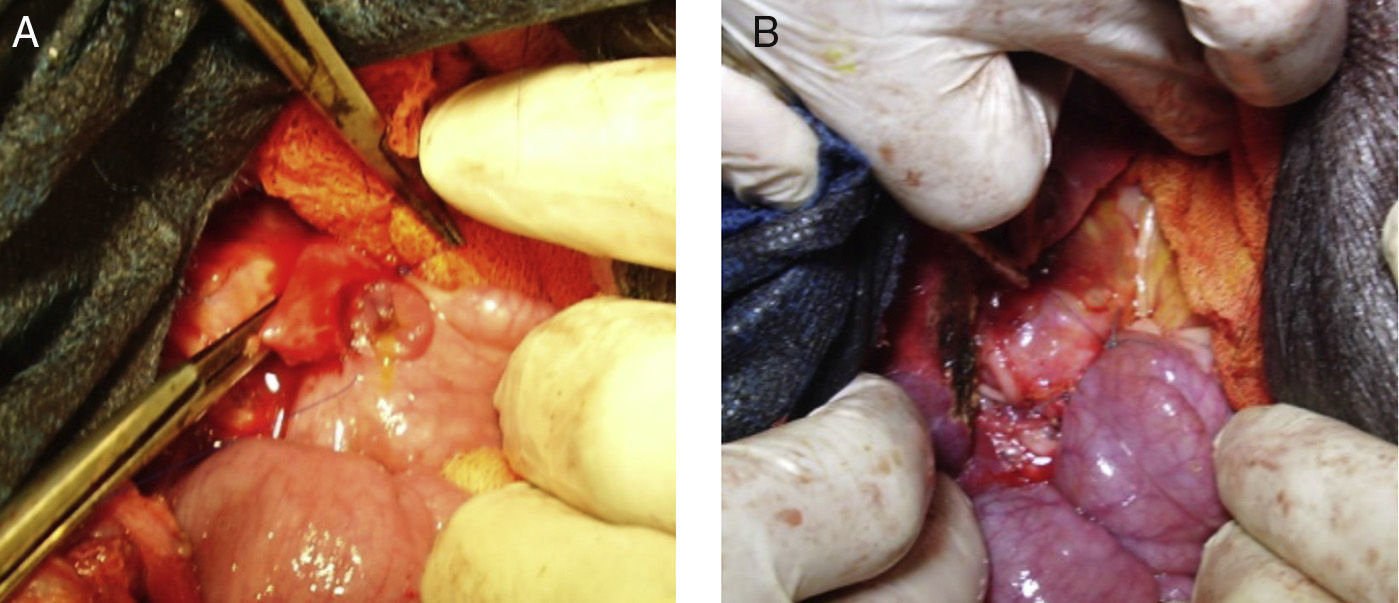
Materials and MethodsAnimal ExperimentThe experiment was done with Yorkshire pigs and in accordance with the laboratory animal protocol of the Medical School at the Universidad Católica de Córdoba, under the supervision of the veterinarian. Nine Yorkshire pigs between the ages of 2 and 4 months of age, whose weight was 18–20kg, were used for the study. Preoperative fasting was 12h; after premedication with intramuscular ketamine hydrochloride (10mg/kg), the airway was controlled with an endotracheal tube through tracheotomy, and venous flow was controlled peripherally with phlebotomy. Intravenous enrofloxacin was administered as antibiotic prophylaxis. The abdominal procedure involved cutting the common bile duct crosswise at the middle third under the cystic duct (n=9); 10mm were resected, and the silicone tube was sutured proximally and distally; the edges of the common bile duct were attached to the Dacron sleeves with continuous polypropylene 4-0 sutures (Fig. 3). The exposed length of the silicone tube was 20mm, which was the distance between the Dacron sleeves. A T-tube was not inserted, nor was the bile drained externally.
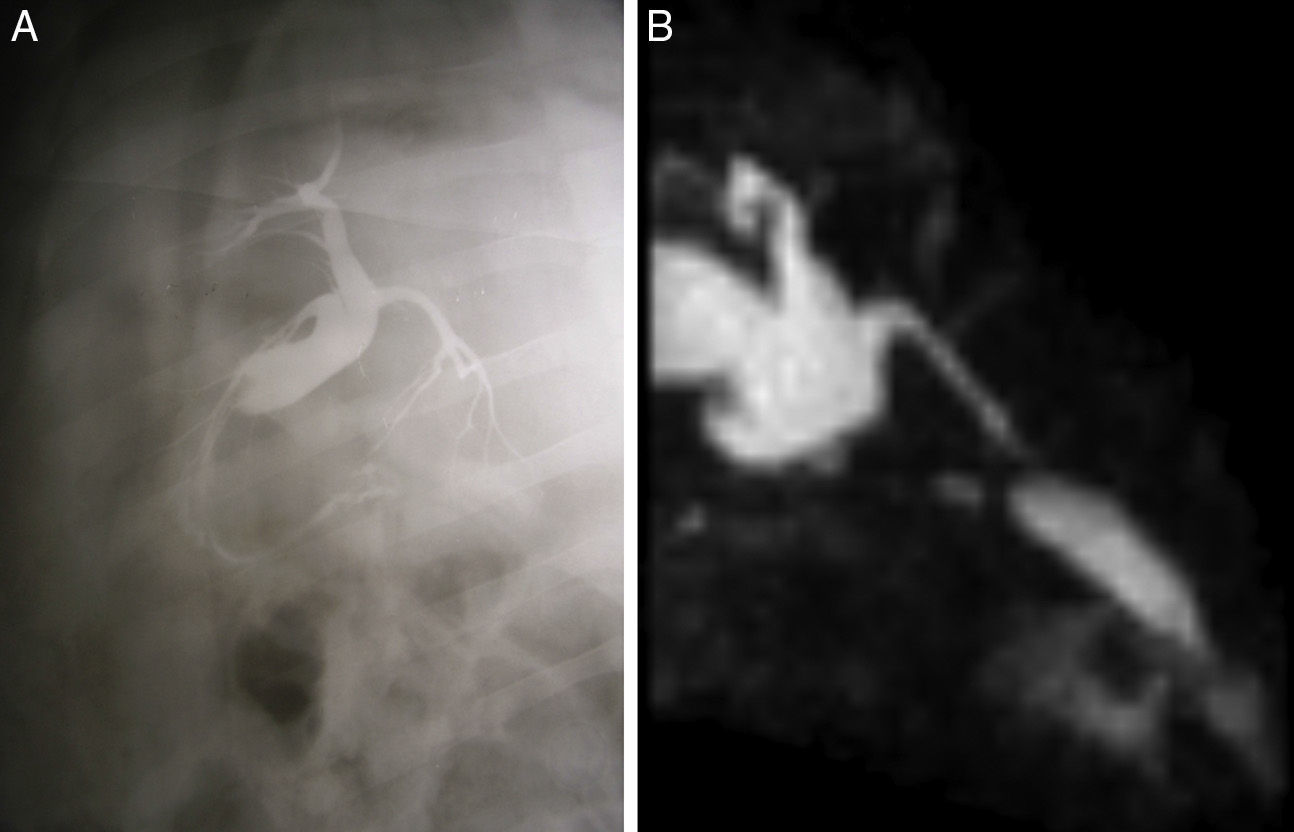
Twelve hours after surgery, the animals were provided access to water; after 24h, they were given the same diet that they had been fed preoperatively. They were monitored daily; antibiotic therapy was administered for 7 days (intramuscular enrofloxacin, every 24h) and analgesia for 3 days (intramuscular diclofenac, every 24h). Post-operative abdominal ultrasound was done 7 days post-op (n=9) and lab work was done at 15 days (n=9) and 60 days (n=9) post-op. The second surgery took place after 60 days. Prior to the second surgery, abdominal ultrasound (n=9) and magnetic resonance cholangiography (n=3) were performed (Fig. 4). Surgery involved perfusion manometry with puncture of the main bile duct using a catheter (n=5), and intraoperative cholangiography (n=9). We extracted the bile duct with the tube (differentiating the portions of the bile duct centimeter by centimeter according to whether they had been in contact with the tube), the hilar plate, distant hepatic biopsies and the second portion of the duodenum adjacent to the bile duct (n=9). The samples obtained were fixed in 10% formaldehyde solution, cut transversally, embedded in paraffin wax and divided into 6μm sections for microscopy studies with hematoxylin and eosin. The hepatobiliary serum enzymes (aspartate transaminase or GOT, gamma-glutamyl transpeptidase, phosphatase alkaline) and total bilirubin were measured before the implantation, 15 days afterwards, and before the second surgery for comparison (60 days).
MethodologyExperimental Design: Preclinical Testing.Subtype: sequential controls
Direction and focus: prospective, longitudinal
Male Yorkshire pigs that had been clinically evaluated by a veterinarian and declared suitable for the study.
Exclusion CriteriaPigs that had not reached a weight of 18–20kg by the age of 2 months or those that were sick and not declared suitable by the veterinarian.
Pigs that were of breeds other than Yorkshire.
Pigs that had been previously operated on, had suffered trauma, or presented deep or superficial wounds.
Absence of bilomas, collections or local/systemic sepsis.
Permeability of the graft throughout the duration of the experiment.
Absence of defined cholestasis, jaundice, and complications of organs in shock.
Absence of failure criteria.
Dehiscence of the proximal or distal anastomosis.
Biloma, collections, abscess, and death.
Local or systemic sepsis.
Graft rejection.
Irreversible alteration of liver function tests.
Biopsies that show cholestasis, fibrosis or hepatic necrosis.
Bile duct fibrosis.
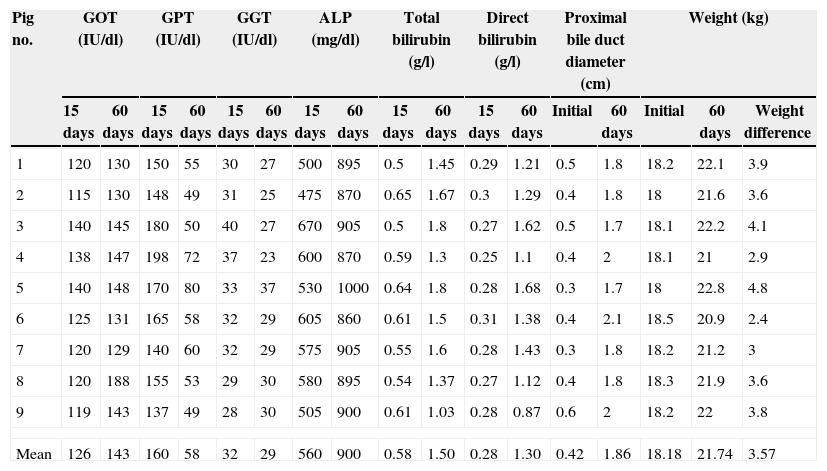
All the pigs survived the first surgery without perioperative complications or events until they were sacrificed after the second surgery (n=9). Weight gain was normal for the age and breed of the animals and oral intake was standard in all cases. There were no fistulas or collections in any of the cases. Physical examination and feces/urine showed no sign of cholestasis. Average weight at the time of surgery was 18.1kg, and mean weight gain before the second surgery was 3.5kg (over 60 days). Laboratory values were altered but did not represent a health risk for the animals (Table 1).
Laboratory Data, Bile Duct Diameter and Weight of the Pigs Studied, Comparing Days 15 and 60 Post-op.
| Pig no. | GOT (IU/dl) | GPT (IU/dl) | GGT (IU/dl) | ALP (mg/dl) | Total bilirubin (g/l) | Direct bilirubin (g/l) | Proximal bile duct diameter (cm) | Weight (kg) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 15 days | 60 days | 15 days | 60 days | 15 days | 60 days | 15 days | 60 days | 15 days | 60 days | 15 days | 60 days | Initial | 60 days | Initial | 60 days | Weight difference | |
| 1 | 120 | 130 | 150 | 55 | 30 | 27 | 500 | 895 | 0.5 | 1.45 | 0.29 | 1.21 | 0.5 | 1.8 | 18.2 | 22.1 | 3.9 |
| 2 | 115 | 130 | 148 | 49 | 31 | 25 | 475 | 870 | 0.65 | 1.67 | 0.3 | 1.29 | 0.4 | 1.8 | 18 | 21.6 | 3.6 |
| 3 | 140 | 145 | 180 | 50 | 40 | 27 | 670 | 905 | 0.5 | 1.8 | 0.27 | 1.62 | 0.5 | 1.7 | 18.1 | 22.2 | 4.1 |
| 4 | 138 | 147 | 198 | 72 | 37 | 23 | 600 | 870 | 0.59 | 1.3 | 0.25 | 1.1 | 0.4 | 2 | 18.1 | 21 | 2.9 |
| 5 | 140 | 148 | 170 | 80 | 33 | 37 | 530 | 1000 | 0.64 | 1.8 | 0.28 | 1.68 | 0.3 | 1.7 | 18 | 22.8 | 4.8 |
| 6 | 125 | 131 | 165 | 58 | 32 | 29 | 605 | 860 | 0.61 | 1.5 | 0.31 | 1.38 | 0.4 | 2.1 | 18.5 | 20.9 | 2.4 |
| 7 | 120 | 129 | 140 | 60 | 32 | 29 | 575 | 905 | 0.55 | 1.6 | 0.28 | 1.43 | 0.3 | 1.8 | 18.2 | 21.2 | 3 |
| 8 | 120 | 188 | 155 | 53 | 29 | 30 | 580 | 895 | 0.54 | 1.37 | 0.27 | 1.12 | 0.4 | 1.8 | 18.3 | 21.9 | 3.6 |
| 9 | 119 | 143 | 137 | 49 | 28 | 30 | 505 | 900 | 0.61 | 1.03 | 0.28 | 0.87 | 0.6 | 2 | 18.2 | 22 | 3.8 |
| Mean | 126 | 143 | 160 | 58 | 32 | 29 | 560 | 900 | 0.58 | 1.50 | 0.28 | 1.30 | 0.42 | 1.86 | 18.18 | 21.74 | 3.57 |
The ultrasound tests showed that the livers had no dilatation of the intrahepatic bile duct, dilatation of the extrahepatic bile duct and permeability of the tube. The liver enzymes were elevated after 15 and 60 days, with no clinical repercussions.
Magnetic resonance cholangiography showed evidence of bile duct dilatation at the common hepatic ducts and the proximal common bile duct of almost 20mm. There was no evidence of intrahepatic dilatation and the prostheses showed permeability. This was corroborated with intraoperative cholangiography, which showed the same characteristics (Fig. 4).
During the second intervention, dissection was simple; we found adherences of the omentum around the site of the implant placement, but this did not compromise the exposed part of the tube, which was free. The duct remained permeable, with no obstruction or local complications. There were no filtrations, bilomas or abscesses in any of the cases, nor were there any deaths. The extrahepatic bile duct proximal to the liver was dilated to a mean of 1.86cm, which was 340%–500% of the initial measurement, depending on the case (Table 1). Intraoperative biliary manometry (using puncture of the common bile duct) demonstrated normal levels (8–10mmHg) and there was no biliary hypertension in any of the cases.
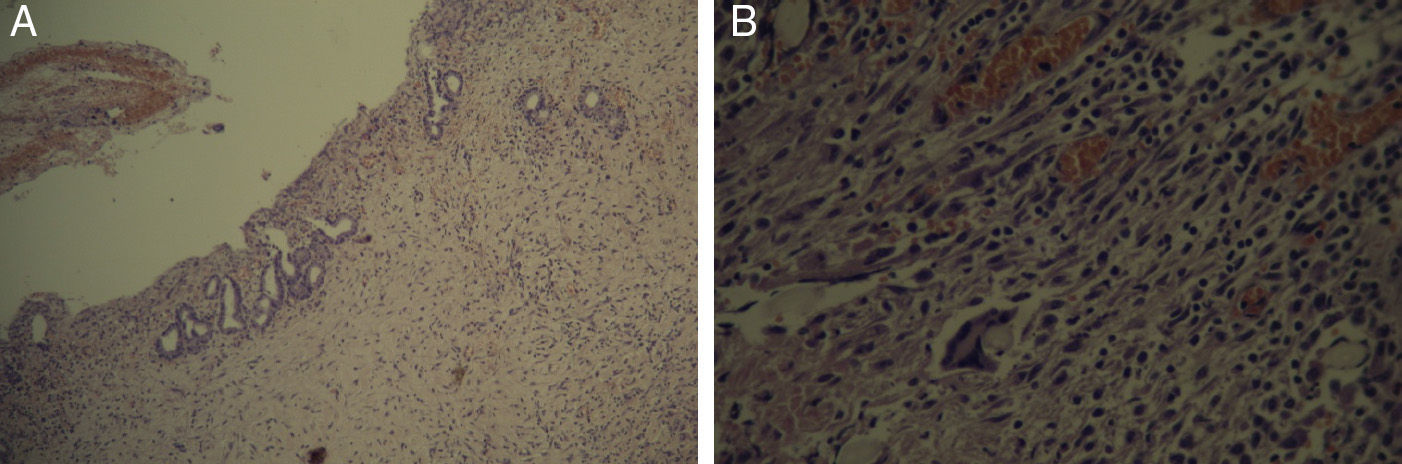
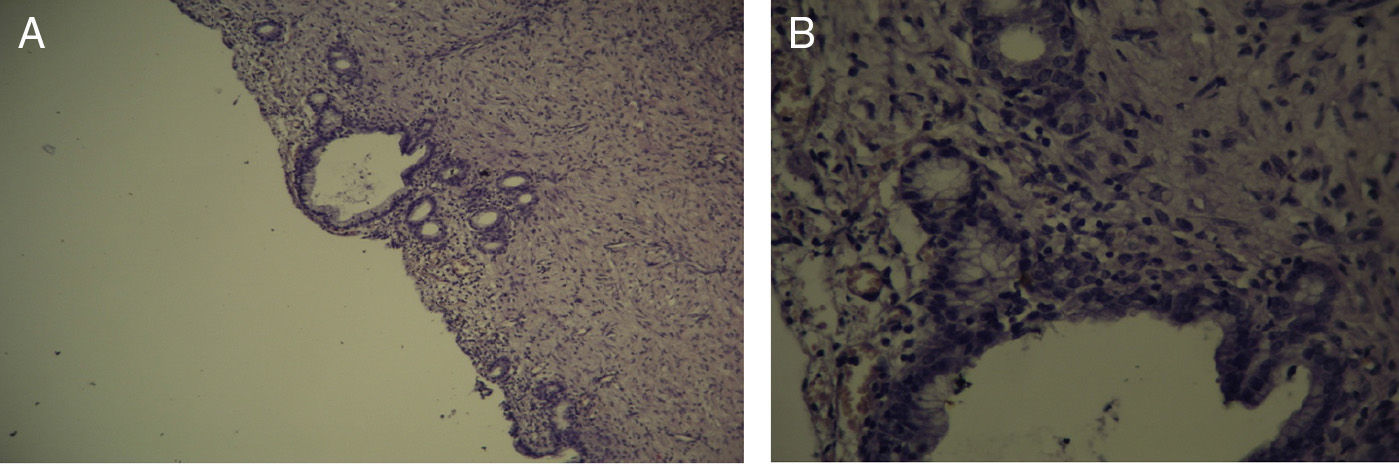
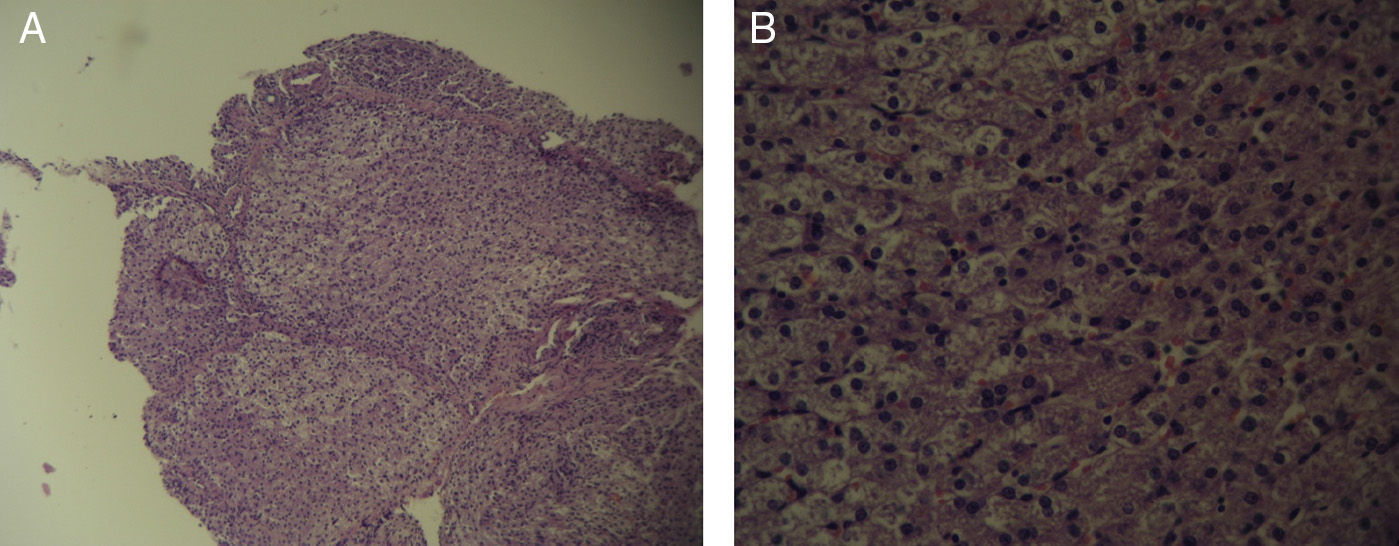
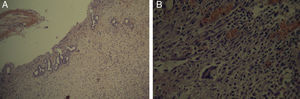
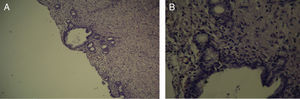
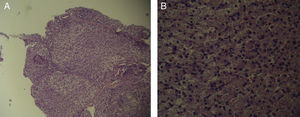
The pathology samples taken from the bile duct showed: from the first centimeter sutured (which remained in contact with the silicone tube for 60 days), there were no signs of fibrosis (Fig. 5); the second centimeter of the bile duct (which did not have contact with the silicone tube) did not present fibrosis (Fig. 6), nor did the distal centimeter of the bile duct. The liver samples after 60 days were normal and had no evidence of cholestasis, fibrosis or sinusoidal dilatation (Fig. 7). The result of the biopsies was similar in the 9 cases (Fig. 8).
Once removed, we examined the prosthesis for colonization (Maki's technique); the colony-forming unit calculation did not surpass 15 units and was therefore negative.
Surgical time was not a study variable, although it did not exceed 1h in any of the cases.
DiscussionThe first surgery involved cutting the main bile duct, which measured mere millimeters in diameter, therefore causing conventional repair to be extremely complicated. In this study, the use of prostheses made the procedures significantly easier, simple, and able to be performed by surgeons with no experience in bile duct surgery.
This study demonstrates that the implantation of silicone tubes in the bile duct does not cause perioperative complications, morbidity or mortality. This new surgical technique could be useful to study cases of iatrogenic injuries to the undilated bile duct (e.g.: during scheduled cholecystectomy), periampullary tumors with cholestasis in inoperable patients that could not be palliated with endoscopic methods, or perhaps biliary stenosis in a transplantation situation, where there still is no ideal solution.10,11
It can be inferred that the pigs used in this present study were low in weight, although we did not find this to be an impediment for analysis. Instead, this created a challenge due to the anatomical variation caused by growth. Surely, larger animals would have downplayed the variation in hepatic volume due to growth and would have allowed us to use tubes with larger diameters and internal lumen, accompanied by expected lower or perhaps no proximal dilatation. In theory, we consider that the dilatation of the extrahepatic bile duct without dilatation of the intrahepatic duct could be explained by the short period of time that the tube remained, which evidently narrowed the diameter of the bile duct.
We believe that maintaining the sphincter of Oddi helped avoid reflux and diminished the possibility for cholangitis, which was not seen in any of the cases and correlates with the negative microbiological findings of the tubes after extraction.
Our findings demonstrate that, in spite of there being a small number of animals studied, 100% cases had no perioperative complications with the substitution of the bile duct for a silicon tube. The size of the small intrahepatic bile ducts did not change during the 60 days; the common hepatic ducts and the common bile duct remnant were dilated in 100% of cases, which later provided for easier biliodigestive anastomosis without the setbacks of intrahepatic cholestasis. Laboratory results were favorable, although there were mild modifications. The pathology results of the bile duct were transcendental because, once it was demonstrated that there were no hepatic repercussions in the time transpired, the objective was not to injure the bile duct tissue. When we examined the bile duct centimeter by centimeter, its relationship with the tube did not cause any damage that would impede any type of future anastomosis or even the placement of another larger-sized silicone tube.
When our technique is compared with recent publications in the literature,5–14 almost all have few study elements and their results do not completely satisfy the proposed objectives. The most important difference with these studies is that our research is an effective temporary repair, with no alteration of the tissues and without leading to subsequent surgeries of the biliary tree.
The use of structures that are not prepared for the low volume and pressure of the biliary tree, such as vein grafts or vascular prostheses, leads to narrowing due to fibrosis and a reduction in diameter. Some authors try to resolve this situation with stent placement. Several cases have been reported with therapeutic success,12,13 but even so this technique requires later stent extraction when it is not absorbable, and there is also the risk of stent migration with later narrowing. This situation becomes even more complicated, as expressed in experimental studies.8 As these techniques are definitive, long-term results would have to be studied with regards to bile duct diameter and surrounding fibrosis. Later surgeries would be necessary when the technique fails.
There have been very interesting experimental-phase studies with polymer implants also done in pigs. However, they leave some questions unanswered, such as the posterior dilatation of the implants over the long term in spite of good tissue acceptance. Other research articles criticize the lack of assessment of the production of perilesional fibrosis, which would lead to later conventional biliodigestive repair if the implant failed.13,14
Repairs with gallbladder flaps7 and jejunal tubes interposed between the bile duct and the duodenum9 are very complex surgical constructions comparable to the biliodigestive anastomoses in the small diameter bile ducts, with associated risk for later necrosis and stenosis.
What is original about this experimental study is that it is the first attempt at replacing the bile duct by suturing a tube of this material and with such a design, while following the concept of a temporary repair. The tube did not become occluded, its diameter did not diminish, there was no torsion, nor was there evidence of infection or displacement. It is evident that it causes elevated enzymes (Table 1), but the elevation is mild and, according to the Schweizer classification,15 we can say that the result is good. We suspect that if we compared it to a plastic stent in the bile duct, the values would be altered to the same extent (but, there are no studies that assess enzyme elevation by placing a stent in a normal bile duct).
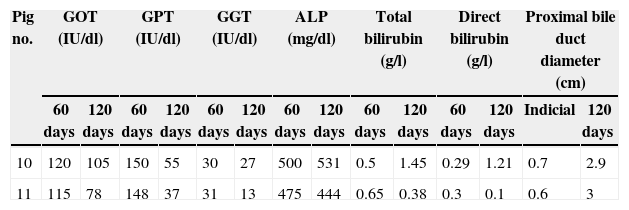
In order to confirm the feasibility of later anastomosis due to the absence of fibrosis, we followed the same procedure in 2 more pigs, and 120 days after placing the silicone tube the lab work showed a decrease in hepatic enzyme levels and bilirubin compared with the levels from the first 60 days (Table 2). When reoperation was performed, the tubes were withdrawn, biopsies were taken in accordance with the protocol, and biliodigestive anastomoses were successfully created (Braun's hepaticojejunal omega loop anastomosis+cholecystectomy) in both cases. The two pigs have lived normal lives and have shown no complications during one year of follow-up.
Lab Data, Diameter of the Bile Duct and Weight of the Pigs Studied, Compared 60 and 120 Days Post-op.
| Pig no. | GOT (IU/dl) | GPT (IU/dl) | GGT (IU/dl) | ALP (mg/dl) | Total bilirubin (g/l) | Direct bilirubin (g/l) | Proximal bile duct diameter (cm) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 60 days | 120 days | 60 days | 120 days | 60 days | 120 days | 60 days | 120 days | 60 days | 120 days | 60 days | 120 days | Indicial | 120 days | |
| 10 | 120 | 105 | 150 | 55 | 30 | 27 | 500 | 531 | 0.5 | 1.45 | 0.29 | 1.21 | 0.7 | 2.9 |
| 11 | 115 | 78 | 148 | 37 | 31 | 13 | 475 | 444 | 0.65 | 0.38 | 0.3 | 0.1 | 0.6 | 3 |
This is a procedure that merits further research. It is potentially valuable in emergency situations because, although it is not a definitive solution, it is a feasible, economic and efficient way for the bile to reach the intestine with a solution that provides continuity to the bile duct. As it does not cause fibrosis, it does not interfere with a future definitive reconstruction, allowing the patient to maintain an acceptable quality of life and proper nutritional status with no external biliary drainage and without causing sepsis.
Conflict of InterestThe authors declare having no conflict of interests.
Please cite this article as: Napolitano DA, Rodríguez Bertola X, Sambuelli GM, Vial LH, Torrecillas DA. Reemplazo temporal del colédoco por tubo de silicona como reparación urgente de la lesión de vía biliar. Estudio experimental en cerdos. Cir Esp. 2015;93:187–193.