Incisional hernia (IH) after colorectal surgery is highly prevalent. The objective of this study is to assess the utility of an algorithm to decide on mesh augmentation after a midline laparotomy for colorectal resection to prevent IH in high-risk patients.
MethodsA prospective study was conducted including all patients undergoing a midline laparotomy for colorectal resection between January 2011 and June 2014, after the implementation of a decision algorithm for prophylactic mesh augmentation in selected high-risk patients. Intention-to-treat analyses were conducted between patients in which the algorithm was correctly applied and those in which it was not.
ResultsFrom the 235 patients analyzed, the algorithm was followed in 166 patients, the resting 69 cases were used as a control group. From an initial adherence to the algorithm of 40% in the first semester, a 90.3% adherence was achieved in the seventh semester. The incidence of IH decreased as the adherence to the algorithm increased (from 28 to 0%) with a time-related correlation (R2=0.781). A statistically significant reduction in IH incidence was demonstrated in high-risk groups in which the algorithm was correctly applied (10.2 vs 46.3%; P=.0001; OR: 7.58; 95% CI: 3.8–15). Survival analysis showed that the differences remained constant during follow-up.
ConclusionThe implementation of the algorithm reduces the incidence of IH in high-risk patients. The adherence to the algorithm also correlates with a decrease in the incidence of IH.
Existe una alta incidencia de hernia incisional (HI) tras cirugía de colon. El objetivo de este estudio fue analizar la utilidad de un algoritmo de decisión para la colocación de malla profiláctica tras laparotomía media por cáncer colorrectal en pacientes de riesgo.
MétodosSe planteó un estudio prospectivo que incluyera a los pacientes intervenidos de cáncer colorrectal por laparotomía media entre enero de 2011 y junio de 2014, tras la implementación de un algoritmo de decisión para la colocación de malla profiláctica en pacientes seleccionados de alto riesgo. Se realizó análisis por intención de tratar entre los pacientes en los que se siguió correctamente el algoritmo y en los que no.
ResultadosDe los 235 pacientes analizados, el algoritmo se siguió correctamente en 166 pacientes, los 69 restantes se usaron como grupo control. Partiendo de una adherencia inicial del 40% en el primer semestre del estudio, se logró llegar a un cumplimiento del 90,3% en el último semestre. La incidencia de HI disminuyó progresivamente a medida que aumentaba la adherencia (de 28 a 0%), con una correlación tiempo-dependiente (R2=0,781). Se logró una disminución estadísticamente significativa de HI en los grupos en los que el algoritmo se aplicó correctamente (10,2 vs 46,3%; p=0,0001; OR 7,58;95% IC: 3,8-15). El análisis de supervivencia demostró que las diferencias se mantuvieron constantes durante el seguimiento.
ConclusionesLa implementación del algoritmo redujo la incidencia de HI en pacientes de riesgo. La adherencia al algoritmo se correlaciona con el descenso en la incidencia de HI.
One of the most frequent complications after abdominal surgery is incisional hernia (IH), especially after midline laparotomy.1 Treatment of this complication consumes many resources, as it often requires surgical repair, either due to complication of the IH or to alleviate symptoms that considerably affect the quality of life of our patients.2
In spite of the advances made in surgical techniques and materials in recent decades, the prevalence of IH remains at excessively high levels; furthermore, there are wide differences between publications, with rates from 3 to 20%, depending on the series.3,4 In patient groups at high risk for IH, the incidence sky-rockets to an alarming 40%.1,5
To avoid complications related with IH, several prevention strategies have been proposed.4 Initially, most studies focused on optimizing closure of the laparotomy to avoid appearance of IH, introducing improvements in the suture material and technical innovations (such as the use of continuous sutures and “total stitches”),6–8 but all have been insufficient. More recently, a new focus has been introduced in the strategy for IH prevention: the use of synthetic prophylactic mesh. Until now, there have only been a few widely accepted indications for the placement of prophylactic mesh, all reserved for specific subgroups like surgery for abdominal aortic aneurysm, bariatric surgery, or the creation of stomas.9–11 However, more recent studies indicate that the use of prophylactic mesh in the closure of midline laparotomies12 could become an excellent tool for the prevention of IH in patients at risk, without increasing morbidity.3,13,14
There are numerous risk factors that have been identified for IH: advanced age, smoking, male sex, previous abdominal surgery, obesity and comorbidities such as malnutrition, chronic kidney disease, diabetes mellitus, immunosuppression and chronic obstructive pulmonary disease.1,15–17 Among these, obesity continues to be the most closely related with IH.18,19
There have also been reports of correlations of the incidence of IH with blood loss and the degree of contamination during surgery.15,20 It is known that contaminated surgeries, such as colorectal resection, present a high prevalence of complications related with the surgical wound, including infection, evisceration and IH.15,19 Nonetheless, in these high-risk cases, the use of prophylactic mesh has not been standardized for the closure of the abdominal wall.
A study done at our hospital in 2013 detected an incidence of IH of 39.9% in a retrospective series of 338 patients treated with colorectal resection for neoplasm. Two groups of patients were identified with increased risk for IH: patients with obesity and non-obese patients who presented a combination of several known risk factors for IH.1 In light of these worrisome results, it was imperative to conceive measures for improvement in order to reduce the incidence of IH and thereby improve the quality of our medical care.
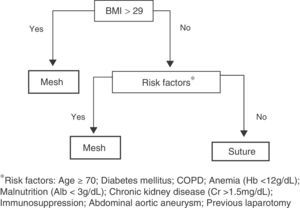
We designed a management algorithm based on the results of the previous study to help our surgeons decide before surgery which patients should be treated with prophylactic mesh.
The objective of this study as to determine whether the use of a decision-making algorithm based on previously identified risk factors for IH can reduce wound complications after colorectal surgery, such as evisceration and IH, as well as to evaluate whether compliance with said algorithm correlates with a reduction in the incidence of IH.
MethodsA prospective, observational study was proposed by the Colorectal Surgery Unit of the General and Gastrointestinal Surgery Department at our university hospital. Included in the study were all those consecutive patients who met the criterion of having undergone elective surgery for colon cancer with curative intent by means of midline laparotomy between 2011 and 2014. Excluded from the study were patients who had been treated by laparoscopy, patients with ventral hernia at the time of the surgery, and patients who had previously been treated surgically for this condition. The creation of a colostomy was not a cause for exclusion.
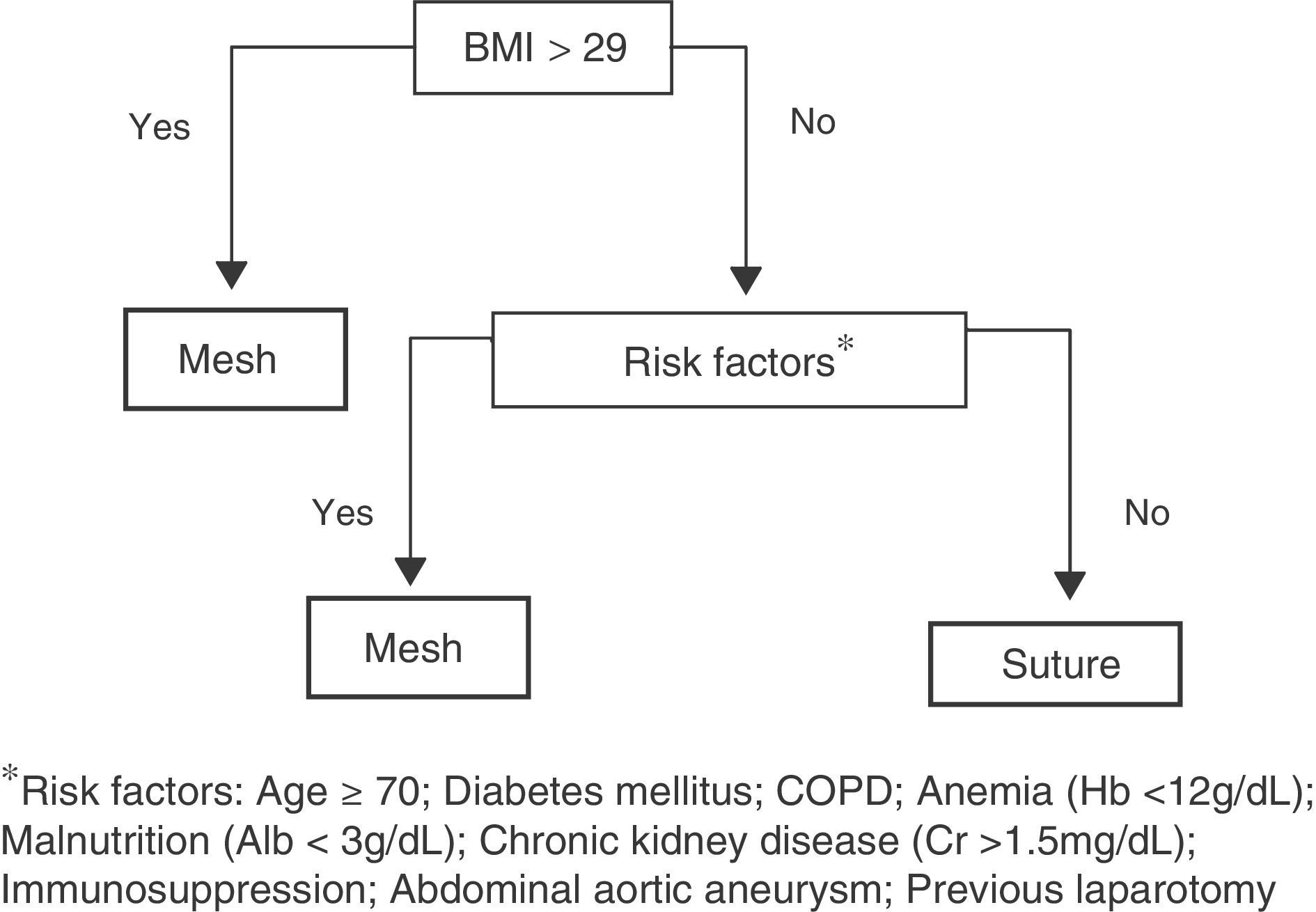
We designed an algorithm (Fig. 1) according to which all patients with a body mass index (BMI) higher than 29 (mean BMI of patients affected by IH in our previous study,1 which we will call group 1), as well as patients with BMI below 29 but with 2 or more risk factors for developing IH (group 2) would be candidates for receiving prophylactic mesh. The remaining patients, who were considered low-risk, underwent laparotomic closure with simple suture (group 3).
The following variables were considered risk factors for IH: BMI >29 (kg/m2), age >70 yrs, chronic kidney disease (serum creatinine >15mg/dL), anemia (hemoglobin <12g/dL), malnutrition (serum albumin <3mg/dL), COPD, diabetes mellitus, previous immunosuppressant treatment with corticosteroids or radio/chemotherapy, aneurysm of the abdominal aorta and previous laparotomy.
The algorithm was presented at the Colorectal Surgery Unit in 2011 and proposed as a treatment guideline. In each specific case, the final decision about mesh placement depended on the operating surgeon. All the surgeons involved had been trained in the prophylactic mesh placement technique. In all cases, the linea alba was closed with continuous suture of slow-absorbing thread (PDS 1® Ethicon, NJ, USA), following the general recommendations for length of thread, distance between stitches and depth.6,7 The subcutaneous plane was closed with interrupted polyglactin 3/0 stitches. The skin was closed with staples. In patients with mesh placement, the material was placed on the supra-aponeurotic plane (onlay) after subcutaneous dissection of 3cm on both sides of the incision. The mesh used was partially absorbable, lightweight and large-pore (Ultrapro®, Ethicon, NJ, USA), which was adapted in each case to the length of the incision and with a minimal width of 5cm, then attached with a double crown of fascia staples (DFS® Autosuture, Covidien, MA, USA). Two subcutaneous suction drains were inserted in all patients with mesh, which were later withdrawn when the discharge fell below 30cc.
All the patients received antithrombotic prophylaxis with low molecular weight heparin and antibiotic prophylaxis with gentamicin and metronidazole, in accordance with the hospital protocol.
Postoperative complications were recorded according to the Clavien-Dindo classification,21 paying special attention to any surgical wound complications, such as evisceration, wound infection and seroma. Minimum follow-up was set at 365 days. The patients were followed in accordance with the protocol established at our hospital for colon cancer: office visit after one month, trimestral follow-up appointments during the first year and annually thereafter in the absence of complications.
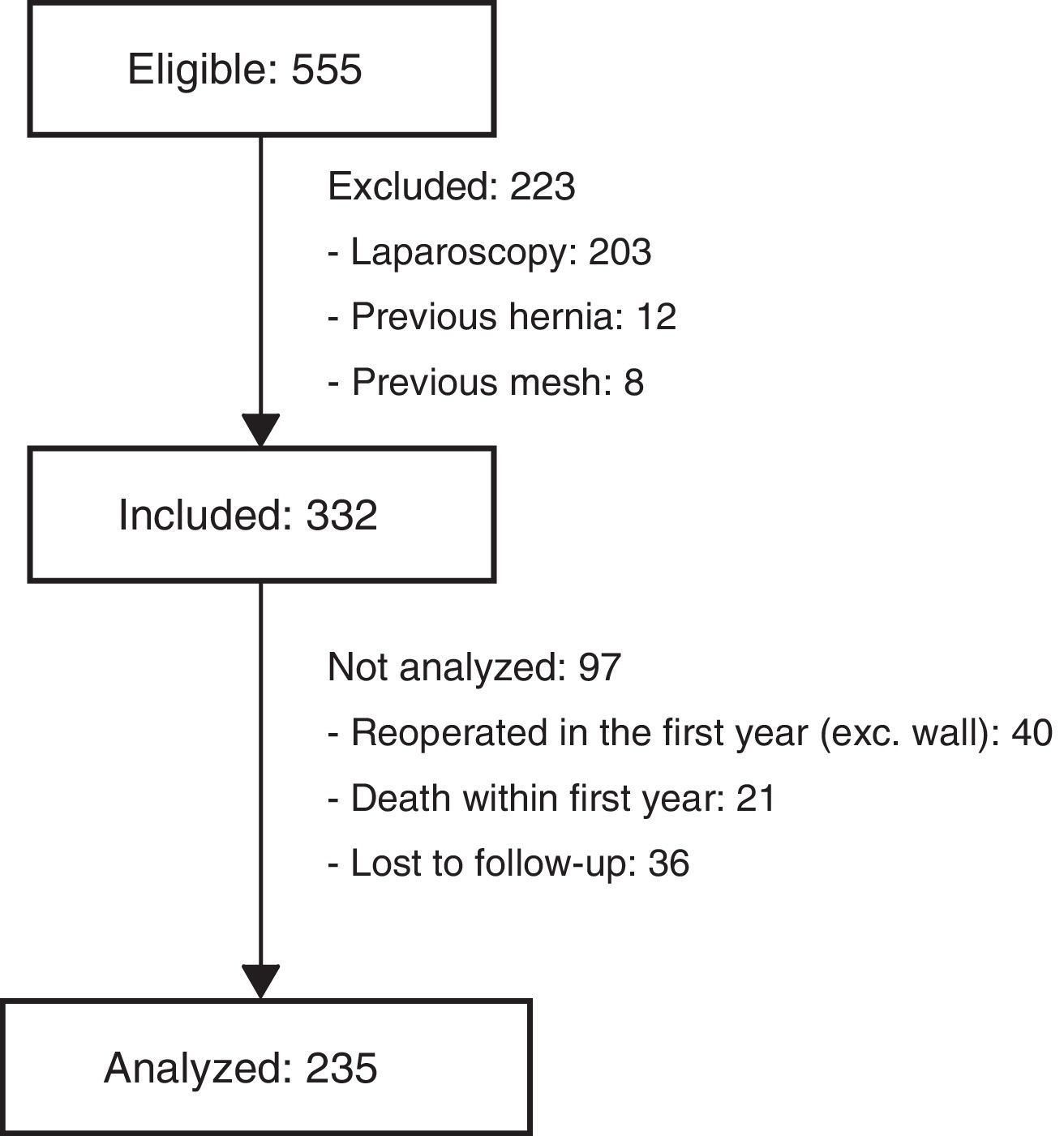
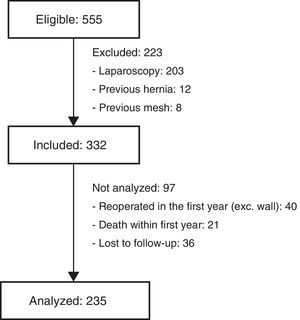
Excluded from the final analysis were those patients who had died during the first year of follow-up, those who had been reoperated with midline laparotomy (for reasons other than an incisional hernia) or those lost to follow-up during this period (Fig. 2). The diagnostic criteria for IH were: clinical diagnosis by a specialized surgeon, IH intervention during the follow-up period or detection of IH by computed tomography done 12 months after surgery, within the follow-up protocol for colon cancer.
The results obtained from the study cohort were analyzed according to the treatment intention, using those cases in which the protocol was not followed (the lead surgeon did not correctly apply the algorithm) as a control group.
The statistical analysis was completed with SPSS v.20 software (IBM Inc. Rochester, MN, USA). The quantitative variables are expressed as mean±standard deviation and the qualitative variables as proportions. To analyze the association between qualitative variables, the chi-squared or Fisher's exact tests were used as necessary; the Student's t or the Mann–Whitney tests were used for the quantitative variables. Normal distribution of the quantitative variables was verified with the Kolmogorov–Smirnov test. Statistical significance was established at P<.05. The correlation was established with the Pearson's linear correlation coefficient. The odds rate for occurrence of IH was calculated for each risk group.
The capability for predicting incisional hernia of each of the variables and their independence from the other predictive variables was analyzed with a binomial logistic regression model by sequentially introducing the variables with an F-to-enter of 0.5.
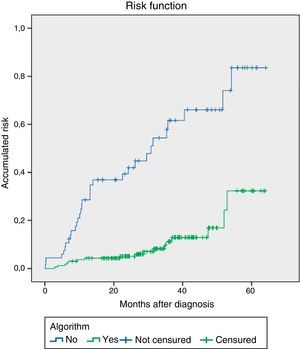
The risk of incisional hernia over time was calculated both for the entire population as well as for subgroups derived from a predictive variable using the Kaplan–Meier non-parametric estimator, considering the survival function as the proportion of patients with no abdominal wall incisional hernia. The correlation of the different predictive variables with the time of the IH was analyzed with the proportional risk model (Cox regression). The risk for presenting IH over time is presented by accumulated risk charts.
Approval of the Ethics Committee was obtained from the hospital. The study was developed following international clinical research standards and guidelines for clinical research (ethics code and Declaration de Helsinki) and in accordance with legal regulations for confidentiality and personal data. The patients included in the study were informed of the risks and benefits of the implantation of prophylactic mesh and have their written informed consent.
ResultsDuring the study period, 555 patients were treated surgically for colorectal cancer, 332 of which met the inclusion criteria; in the end, 235 patients were analyzed. The median follow-up period was 31.2 months (SD 15.3). The reasons for exclusion are shown in Fig. 2.
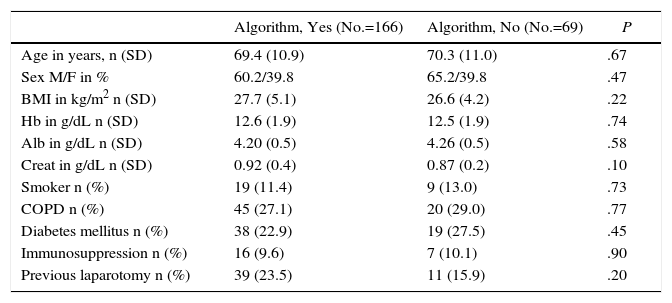
Throughout the study period, the algorithm was correctly applied in 166 patients (70.6%); in the remaining 69 cases, the surgeons applied their criteria for the closure technique, without following the proposed protocol. Compliance with the algorithm, assessed each semester, progressively increased in a notable manner from 40.5% at the start of the study (2011) to 90.5% in the last semester of 2014. The incidence of IH correlated inversely with the progressive compliance with the algorithm, decreasing from 28 to 0% (Pearson's linear regression: y=−0.426x+44.77; R2=0.781). Table 1 shows a comparison for the demographic characteristics and the risk factors in the study groups (algorithm/no algorithm). The groups are comparable, with no significant differences in the relevant preoperative parameters.
Comparison of the Demographic Characteristics and Risk Factors Among the Study Groups (No.=235).
| Algorithm, Yes (No.=166) | Algorithm, No (No.=69) | P | |
|---|---|---|---|
| Age in years, n (SD) | 69.4 (10.9) | 70.3 (11.0) | .67 |
| Sex M/F in % | 60.2/39.8 | 65.2/39.8 | .47 |
| BMI in kg/m2 n (SD) | 27.7 (5.1) | 26.6 (4.2) | .22 |
| Hb in g/dL n (SD) | 12.6 (1.9) | 12.5 (1.9) | .74 |
| Alb in g/dL n (SD) | 4.20 (0.5) | 4.26 (0.5) | .58 |
| Creat in g/dL n (SD) | 0.92 (0.4) | 0.87 (0.2) | .10 |
| Smoker n (%) | 19 (11.4) | 9 (13.0) | .73 |
| COPD n (%) | 45 (27.1) | 20 (29.0) | .77 |
| Diabetes mellitus n (%) | 38 (22.9) | 19 (27.5) | .45 |
| Immunosuppression n (%) | 16 (9.6) | 7 (10.1) | .90 |
| Previous laparotomy n (%) | 39 (23.5) | 11 (15.9) | .20 |
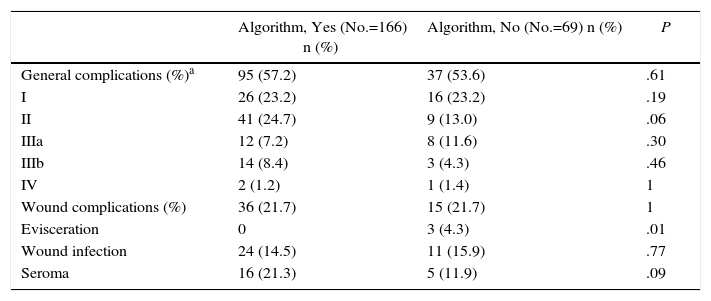
Both groups presented a similar overall incidence of postoperative complications. As for the complications related with the surgical wound, 3 patients presented evisceration, all of whom belonged to the group in which the algorithm had not been followed (4.6 vs 0%; P=.03). The patients who were treated according to the algorithm presented a higher incidence of seroma (21.3 vs 11.9%; P=.09). Both groups presented similar wound infection percentages (Table 2). In no case was it necessary to remove the mesh due to infection or intolerance.
Postoperative Results in Both Groups (No.=235).
| Algorithm, Yes (No.=166) n (%) | Algorithm, No (No.=69) n (%) | P | |
|---|---|---|---|
| General complications (%)a | 95 (57.2) | 37 (53.6) | .61 |
| I | 26 (23.2) | 16 (23.2) | .19 |
| II | 41 (24.7) | 9 (13.0) | .06 |
| IIIa | 12 (7.2) | 8 (11.6) | .30 |
| IIIb | 14 (8.4) | 3 (4.3) | .46 |
| IV | 2 (1.2) | 1 (1.4) | 1 |
| Wound complications (%) | 36 (21.7) | 15 (21.7) | 1 |
| Evisceration | 0 | 3 (4.3) | .01 |
| Wound infection | 24 (14.5) | 11 (15.9) | .77 |
| Seroma | 16 (21.3) | 5 (11.9) | .09 |
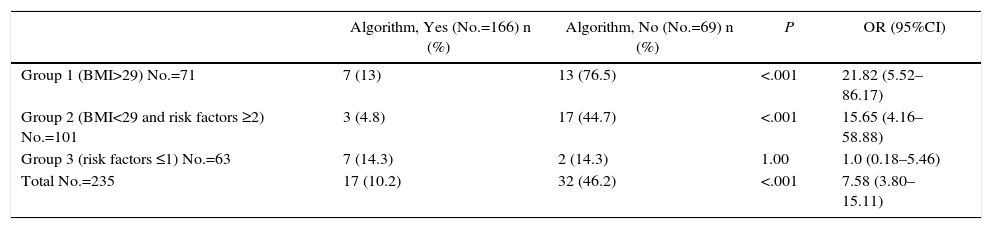
During follow-up, a total of 49 IH were diagnosed, 23 of which were symptomatic, with surgical indication. The high-risk patients (groups 1 and 2) presented an elevated incidence of IH when the algorithm was not correctly followed (no prophylactic mesh was used) (60.6 vs 8.9%; P<.01; OR 18.7; 95%CI: 4.8-72.5). These differences were maintained in the analysis by subgroups: group 1 (76.5% without mesh vs 13% with mesh; P<.01; OR 21.8; 95%CI: 5.5–86.2) and group 2 (44.7% without mesh vs 4.8% with mesh; P<.01; OR=15.7; 95%CI: 4.2–58.8). In contrast, in patients at low risk who only required suture (group 3), no statistically significant differences were found between those who were overtreated (unnecessarily implanted mesh) and those that had been closed with continuous suture alone, following the recommendation of the algorithm (Table 3).
Comparison of the Incisional Hernia Rate and Adherence to the Algorithm Between the Risk Groups (No.=235).
| Algorithm, Yes (No.=166) n (%) | Algorithm, No (No.=69) n (%) | P | OR (95%CI) | |
|---|---|---|---|---|
| Group 1 (BMI>29) No.=71 | 7 (13) | 13 (76.5) | <.001 | 21.82 (5.52–86.17) |
| Group 2 (BMI<29 and risk factors ≥2) No.=101 | 3 (4.8) | 17 (44.7) | <.001 | 15.65 (4.16–58.88) |
| Group 3 (risk factors ≤1) No.=63 | 7 (14.3) | 2 (14.3) | 1.00 | 1.0 (0.18–5.46) |
| Total No.=235 | 17 (10.2) | 32 (46.2) | <.001 | 7.58 (3.80–15.11) |
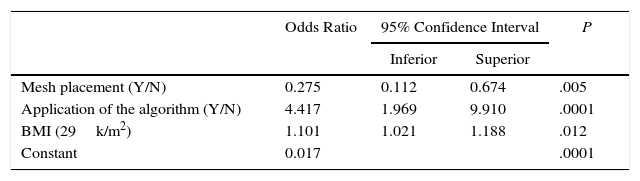
All variables that were potentially associated with the occurrence of IH were considered independent in the binomial logistic regression analysis. The dichotomic variables “algorithm applied” and “mesh placement” as well as “BMI” as a continuous quantitative variable were identified as independent variables for predicting the absence of IH during follow-up (Table 4).
Independent Predictive Variables for the Absence of IH in the Multivariate Analysis (No.=235).a
| Odds Ratio | 95% Confidence Interval | P | ||
|---|---|---|---|---|
| Inferior | Superior | |||
| Mesh placement (Y/N) | 0.275 | 0.112 | 0.674 | .005 |
| Application of the algorithm (Y/N) | 4.417 | 1.969 | 9.910 | .0001 |
| BMI (29k/m2) | 1.101 | 1.021 | 1.188 | .012 |
| Constant | 0.017 | .0001 | ||
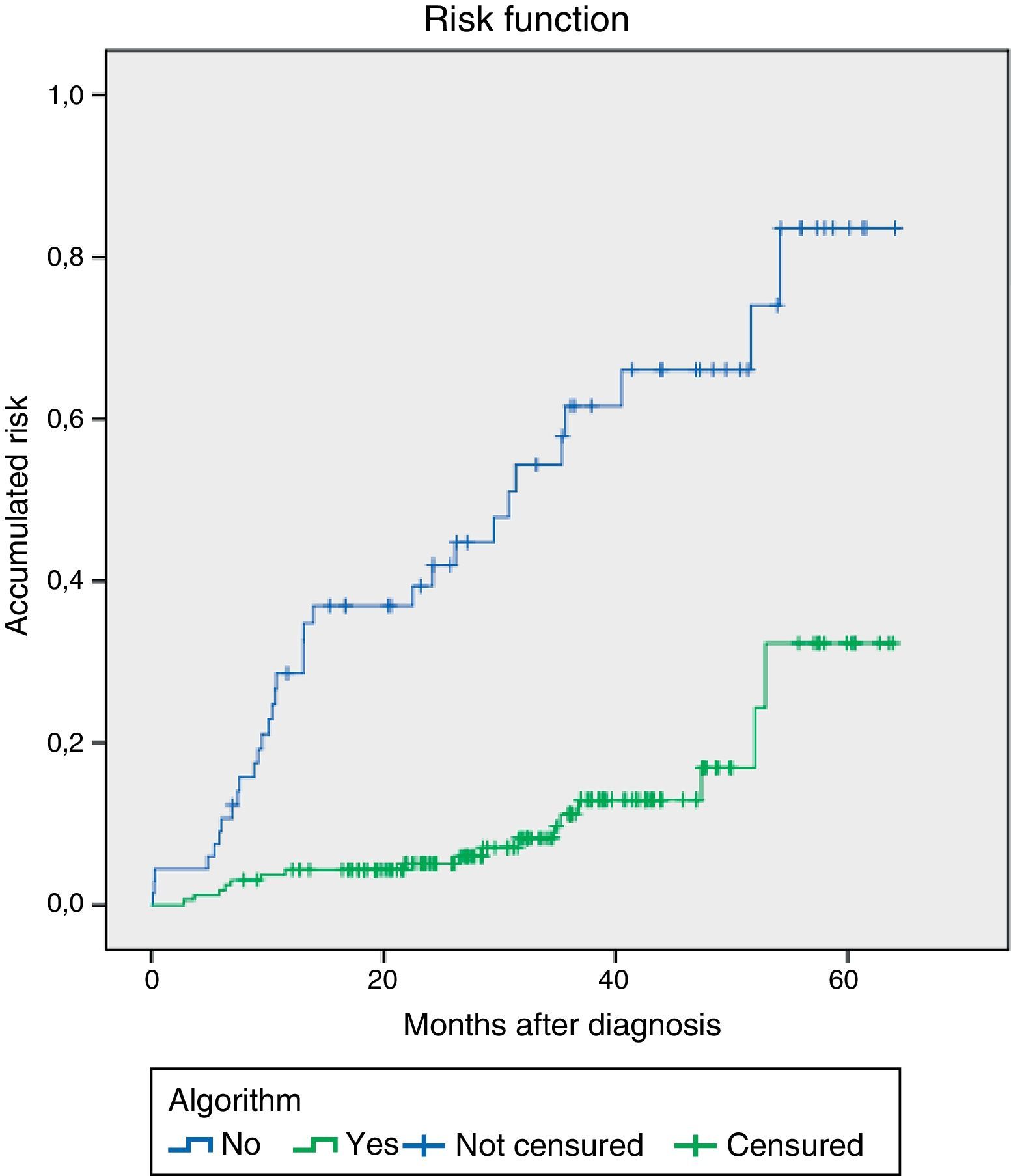
When we applied the survival analysis to the indemnity of the abdominal wall using Kaplan–Meier, significant differences were observed (log rank test) between the groups according to whether the algorithm was applied (Fig. 3). Likewise, the model based on the Cox regression analysis for the variable “algorithm applied” estimated the hazard ratio at 4.8 (95%CI: 2.6–8.6; P=.001) for the prevention of incisional hernias. Thus, the patients in whom the recommendations of the algorithm were followed experienced a lower rate of IH since the start of follow-up, with a distance that was almost constant at 12 months after the intervention until the end of follow-up.
DiscussionThe results of the study indicate that the placement of prophylactic mesh is an effective measure for the prevention of IH in patients treated with laparotomy for colorectal resection, without increasing morbidity. Our results are consistent with those previously reported in randomized prospective studies that included all types of laparotomies.3,5
The implementation of the algorithm has been beneficial, as it has achieved an overall reduction in IH incidence of 20.8%, which in this group of patients can be considered acceptable. In fact, this reduction could have been more defined with greater surgeon compliance: when the algorithm was correctly applied, the incidence of IH fell to 10.2%. This initial lack of adherence is one of the limitations of our study, as the algorithm was correctly followed in only 70.2% of cases. This is probably due to the natural resistance of surgeons in our setting to changing their standard procedures or to the lack of diffusion of current prophylactic measures among experienced specialized surgeons. In fact, when we analyze the compliance data throughout the study period, we observed that, in the first year, only 48.4% (No.=128) of the patients were treated according to the protocol, while in the following months the algorithm was complied with in 69% (No.=158) and reached 90.3% (No.=21) in the last semester of the study period. This datum demonstrates growing confidence toward the measures proposed and also demonstrates a clear correlation between compliance with the algorithm and a progressive reduction in the incidence of IH.
The use of the algorithm as a therapeutic decision-making tool has been shown to be useful in all the patient groups. In obese patients, there is sufficient evidence to recommend the placement of prophylactic mesh as a prevention measure for IH. Other authors have already indicated that obesity, or even excess weight in patients with lower BMI (25–29kg/m2), is a major risk factor for IH; it has also been used as a main criterion in risk scores to guide therapeutic decision-making.18
A significant reduction was also achieved in the rate of IH in non-obese patients with associated risk factors (group 2), in whom the incidence of IH dropped from 44.7 to 4.8% when the algorithm was applied.
In low-risk patients (group 3), a significant reduction in IH to 14.3% was also observed when compared with our previous study. It is likely that the Hawthorne effect22 improved the quality of the abdominal wall closure by our surgeons. In fact, when we compared the overtreated patients, in whom mesh was used unnecessarily, with those who received only sutures, no significant differences were found. This is paradoxical and provides evidence that it is necessary to intensify the analysis of the risk factors for IH and more precisely identify which patients could benefit from the placement of prophylactic mesh.
The logistic regression analysis demonstrated that, among the independent variables, the application of the algorithm has a greater influence than prophylactic mesh in the prevention of incisional hernias. We have not identified any studies in which the application of a preventive measure of these characteristics emerged as an independent variable in a multivariate analysis for the prevention of incisional hernias.
In addition, as can be observed in the survival curve, the protective effect of the algorithm remains constant over time: the patients in whom the algorithm was correctly applied presented a lower rate of IH, which remained practically constant throughout the follow-up.
The major limitation of our study is the absence of a structured protocol in its design. Instead, the algorithm was a proposed therapeutic intervention whose aim was to improve the poor results identified in the previous study. As a mere recommendation, its application in medical practice was very lax in the first study period. In spite of this and the lack of randomization, our results, like those from previous publications,3,5 are strong and consistent enough to consider that prophylaxis with mesh could be beneficial in these patients. The algorithm probably has room for improvement, like all risk assessment tools designed to date. The short-stitch technique, which, according to recent publications, is associated with a low incidence of IH,23 was not used in our series. Currently, it has been systematically adopted by our department, following the recommendations of the European Hernia Society.6
In conclusion, we consider that the implementation of an algorithm for the application of preventive measures, such as prophylactic mesh, reduces the incidence of IH in patients treated with midline laparotomy for colorectal cancer resection. The use of prophylactic mesh reduces the incidence of IH, especially in the presence of obesity or the combination of risk factors for IH. Patients without risk factors can be closed with suture alone, resulting in acceptable IH rates.
Authorship/CollaboratorsStudy design: N. Argudo, J.A. Pereira.
Data collection: M.P. Iskra, M. Pera.
Analysis and interpretation of the results: J. A. Pereira, N. Argudo.
Article composition: J. A. Pereira, N. Argudo.
Critical review and approval of the final version: M. Pera, J. J. Sancho, Luis Grande, M. López-Cano.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Argued N, Iskra MP, Pera M, Sancho JJ, Grande L, López-Cano M, et al. Un algoritmo para la colocación de malla profiláctica en pacientes de riesgo reduce la incidencia de hernia incisional tras laparotomía por cáncer colorrectal. Cir Esp. 2017;95:222–228.
The results of this manuscript were presented at the 38th International Congress of the European Hernia Society, held in Rotterdam (Netherlands), June 5–8, 2016.