Congenital diaphragmatic hernia incidence is one in 3000 live births, Bochdalek hernia occurs through a posterolateral defect. It is very rare in adults. We present a case of late relapsed one diagnosed in an adult male. He underwent an open intervention of Bochdalek hernia at first day of life and required reintervention at seventh month due to recurrence. Now, computerized tomography scan demonstrates a right diaphragmatic defect with intrathoracic hydronephrotic kidney. Nephrectomy was performed with Video-assisted Thoracic Surgery using laparoscopic ports and material. The diaphragmatic defect was closed with a polypropylene mesh. The patient was discharged after 72 h.
La incidencia de hernia diafragmática congénita es de uno en 3000 nacidos vivos, la hernia de Bochdalek ocurre a través de un defecto diafragmático posterolateral. Es muy raro en adultos. Presentamos un caso de recidiva tardía diagnosticada en un varón adulto. Se sometió a una intervención abierta de hernia de Bochdalek el primer día de vida y requirió reintervención por recurrencia al séptimo mes. La tomografía computarizada actual demuestra un defecto diafragmático derecho con riñón hidronefrótico intratorácico. Se realizó nefrectomía mediante cirugía torácica vídeo-asistida utilizando puertos y material laparoscópicos. El defecto diafragmático se cerró con una malla de polipropileno. El paciente fue dado de alta a las 72 horas de la intervención.
The incidence of congenital diaphragmatic hernia (CDH) is one in 3000 live births. It is very rare in adults.1 Depending on the location of the herniation, they have different names: Bochdalek hernia (BH) occurs through a posterolateral diaphragmatic defect whereas Morgagni hernia appears through an anterior retrosternal or parasternal diaphragmatic defect. BH was first described by Vincenz Alexaner Bochdalek in 18482 and constitutes 80%–90% of all CDH. It follows from incomplete fusion of pleuroperitoneal folds during early fetal development.3 It is diagnosed shortly after birth in most of the cases. It remains asymptomatic in many adults and is incidentally diagnosed in 5% of cases on routine investigations for abdominal or respiratory problems. BH can include the omentum (92%), splenic flexure of the colon (58%), stomach (25%), and spleen on the left side, and liver and small intestine on the right side,2 but the presence of kidney is rare. The size of the defect can range from less than one cm to complete absence of the hemidiaphragm.
We present a case of incidentally diagnosed relapsed BH with intrathoracic right kidney in an adult male as part of diagnostic work-up for recurrent respiratory and urinary infections.
Surgical techniqueTwenty-one-year-old men presented to Emergency Department with fever and cough. Physical examination revealed decreased respiratory sounds at right hemithorax. He has clinical history of repeated respiratory infections since his childhood, and urinary tract infections for the past four years.
He underwent a subcostal laparotomy at first day of life due to sudden distress, with a chest radiograph that showed diaphragm elevation and mediastinal deviation to left side. Herniated contents were right and transverse colon, small intestine, right kidney and part of liver. A primary closure of the diaphragmatic defect with non-absorbable sutures was performed. He required another open intervention at 7th month due to recurrence though the same approach.
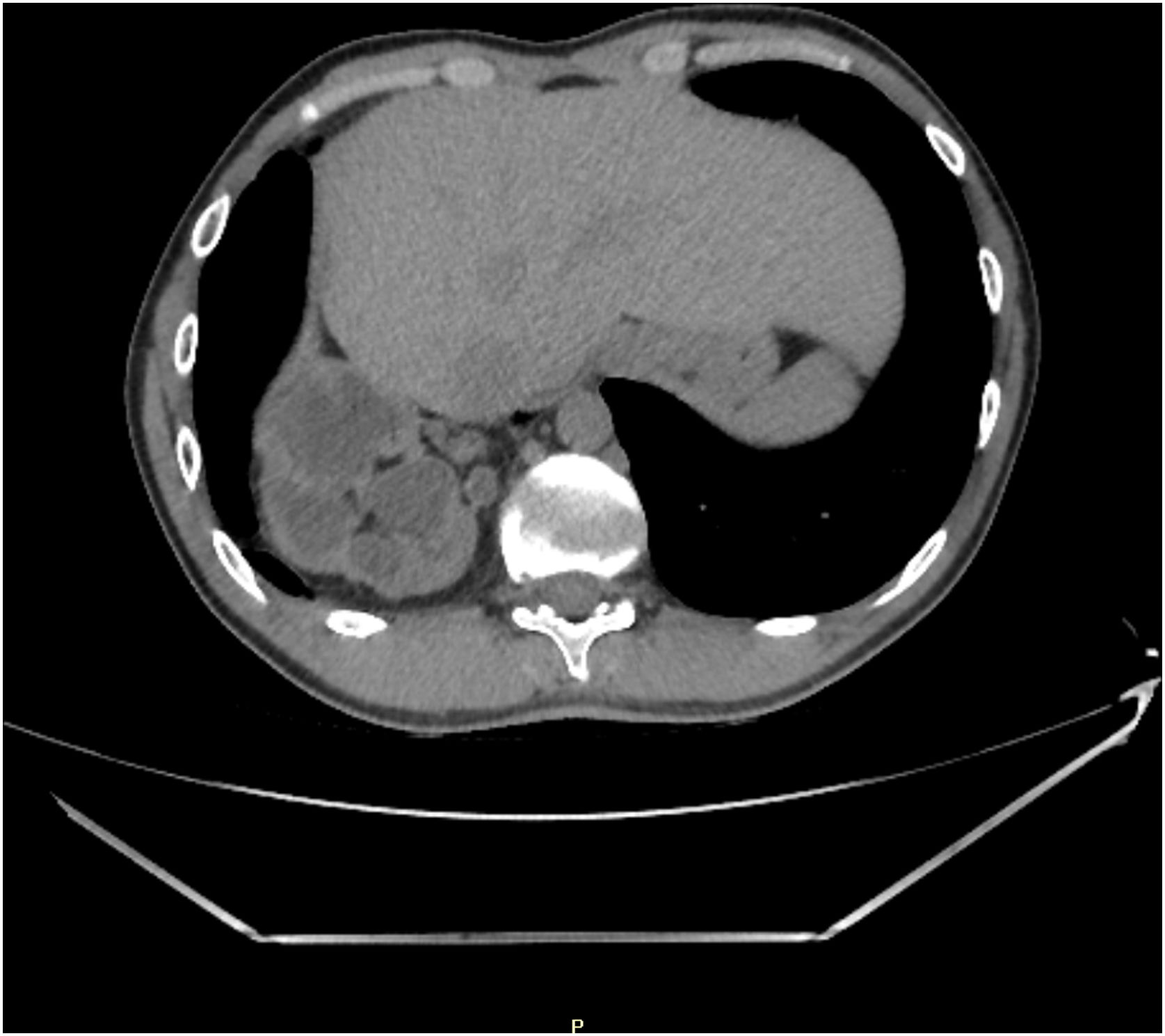
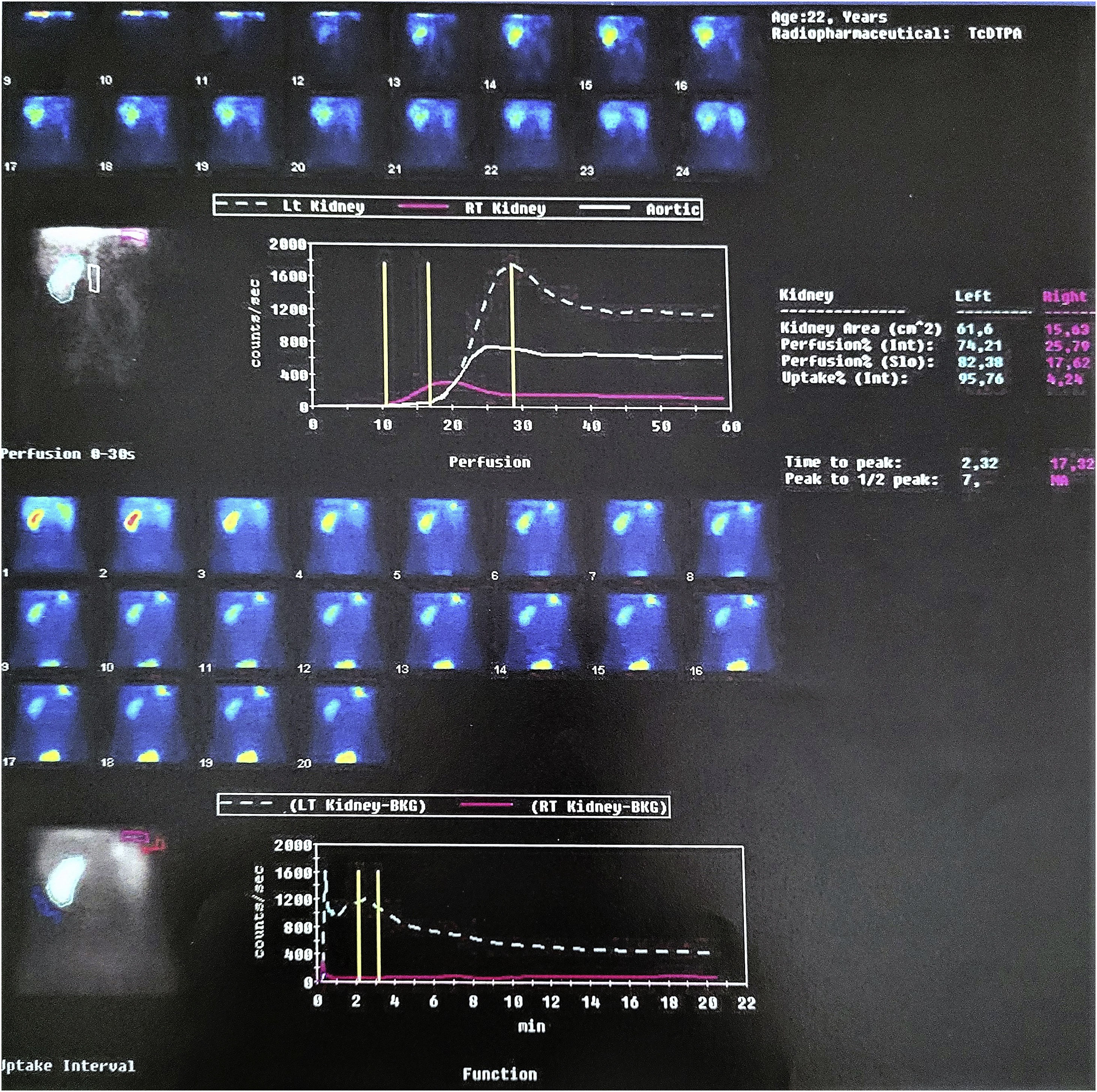
Contrast-enhanced computed tomography (CT-scan) was performed, demonstrating a right diaphragmatic defect with intrathoracic right adrenal gland and grade III–IV hydronephrotic kidney (Fig. 1). Renal scintigraphy revealed a complete functional abolition of right kidney (Fig. 2). A Magnetic Resonance (MRI) disclosed ureteral involvement at the hernial orifice (Fig. 3).
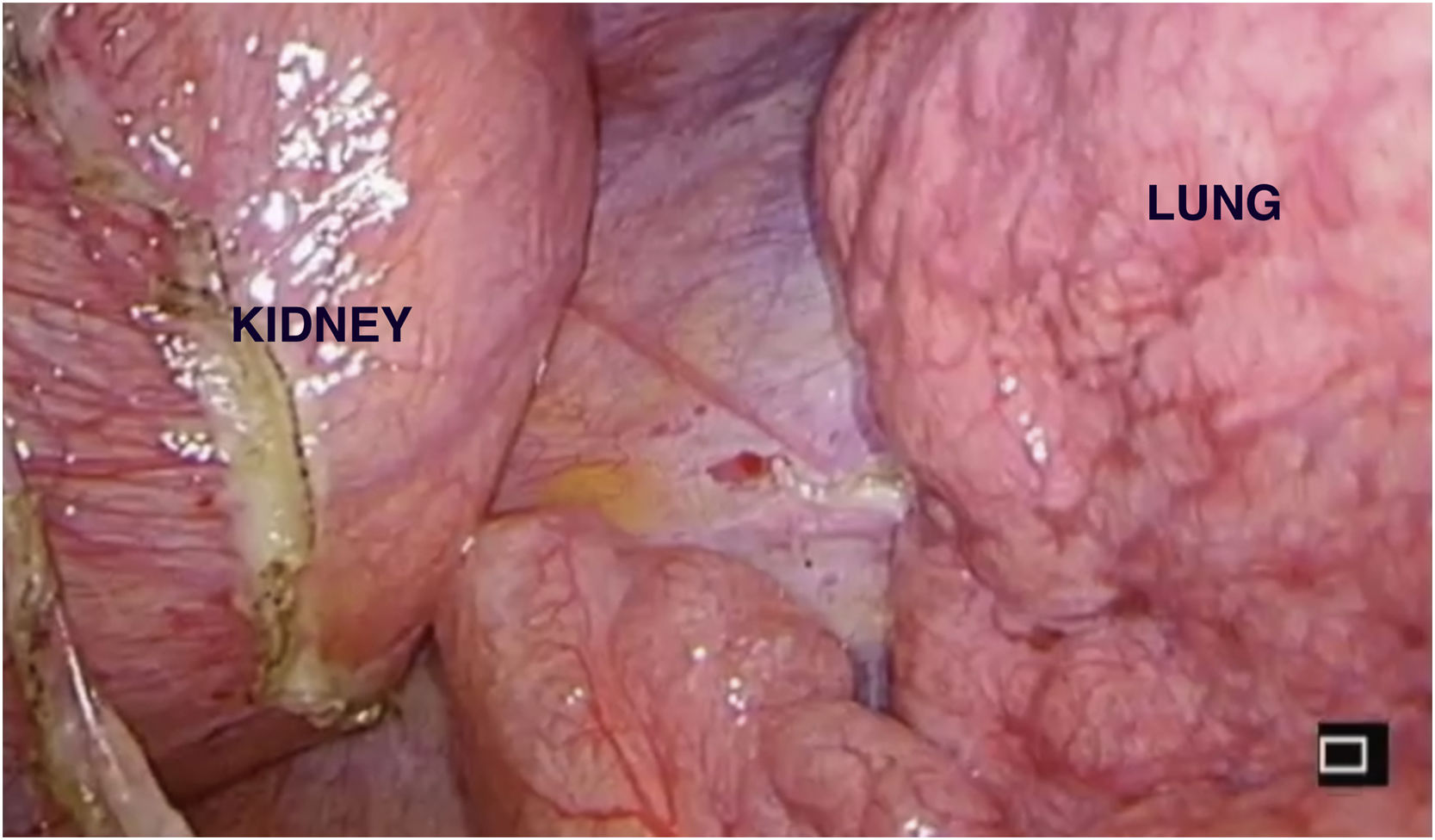
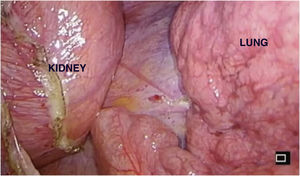
Given the findings, right nephrectomy and partial adrenalectomy were performed using Video-assisted Thoracoscopic Surgery (VATS) approach, under general anesthesia with double-lumen endotracheal intubation and contralateral one-lung ventilation. The patient was placed in left lateral decubitus position. Right-side four trocars were placed: at sixth intercostal space (ICS) at scapular line (5 mm), seventh ICS at mid-axillary line (11 mm), eighth ICS at scapular line (5 mm) and fifth ICS at anterior axillary line (11 mm) (Fig. 4). Pleuropulmonary adhesions were released. We identified the diaphragmatic defect, on which a mass was lodged in contact with the posterior thoracic wall, corresponding to the atrophic right kidney (Fig. 5). Right kidney pedicle was dissected and clipped with hem-o-loks®. The surgical specimen was extracted, after morcellation, through the 11 mm trocar orifice. The diaphragmatic defect, of approximately 6 cm, was closed with loose stitches of Surgidac™ with Endo Stitch™ device, and trans-parietal stitches with Endo-Close™ Auto Suture device. Also, a polypropylene mesh fixed with AbsorbaTack™ and a 28 Fr drainage connected to Pleur-Evac™ were place. The operating time was 360 min and intraoperative blood loss 100 ml. Urologists, thoracic and general surgeons were involved in the surgery. The drainage was removed after 48 h and patient was discharged at 72 h.
DiscussionCDH is a rare condition with an incidence of 0.08−0.45 per 1000 births.1 BH it is the most common one. This alteration is produced by an absence of closure of the pleuroperitoneal duct between weeks eight and ten of intrauterine life.3 Most BH present as neonatal respiratory distress or gastrointestinal obstruction and are immediately repaired, which has a morbidity rate up to 50%, so it rarely progresses to adulthood.4 Nevertheless, in adults, asymptomatic patients typically are female with right-sided defects, whereas symptomatic patients tend to have left-sided defects.5 Due to the liver’s location and early embryonic fusion of right-sided pleuroperitoneal folds, up to 90% of BH occur on the left.5,6 In 1% of cases, kidney herniation can occur either from direct migration of the kidney through the defect during a patient’s lifetime (acquired), or less often during embryogenesis (intrathoracic renal ectopia).
Chest radiograph can be useful in the diagnostics but thoracic CT-scan is the preferred investigation.2
Though previously regarded as a benign entity, recent studies,7 suggests an appreciable risk of symptoms, complications, and a risk to kidney function. Thus, close biochemical and imaging surveillance are recommended of affected patients, with low threshold for intervention in those with renovascular stenosis, reflux, or hydronephrosis.
Traditional open approaches for diaphragmatic hernias have largely been replaced by laparoscopic or thoracoscopic repairs, as minimally invasive approaches have decreased average hospital length of stay (4 vs. 14 days), complication rates (five vs. 17%), and 30-day morbidity rates (0 vs. 3%) compared to open repairs.5 Left-sided and anterior defects are typically approached transabdominally; however, the optimal surgical approach for right-sided defects is controversial.
The recurrence rate after any types of surgical repair is low,8 although our case suffered from two recurrences.
In conclusion, a right-sided diaphragmatic hernia containing an intrathoracic kidney is a rare entity. Thoracoscopic diaphragmatic hernia repair appears to be a safe and feasible procedure. It is a good option even with large diaphragmatic defects and herniation of retro-peritoneal organs, allowing even nephrectomy of atrophic kidney and mesh placement. We describe a right-sided VATS using laparoscopic ports and material. This approach was not previously reported in the literature for this indication. Its advantages include improved visualization of the posterolateral defect and triangulation capacity for pedicle dissection and intracorporeal suturing during mesh placement. Its use is limited by the experience of the surgeon. Large studies are required to further investigate its utility and outcomes in the management of diaphragmatic hernias.
Funding and conflict of interestAuthors declare that they have no conflicts of interest nor financial support to disclose. All authors have approved the final version of the manuscript, which is not under consideration for publication elsewhere.