Short bowel syndrome (SBS) affects patients who have lost part of their intestine, either anatomically or functionally. In adults, the main cause is primary or secondary bowel ischemia, although less frequently it may be the result of inflammatory bowel disease or radiation enteritis.1 Mid-term mortality is high, mainly due to bacterial overgrowth, catheter sepsis2 or liver failure associated with parenteral nutrition (PN).3 Previously, the only solutions in cases of extreme SBS were intestinal transplantation or permanent PN. Since then, several surgical techniques have been developed to try to avoid these solutions, which result in poor quality of life and limited survival. One of these techniques is the so-called serial transverse enteroplasty (STEP) method proposed by Kim et al.4 using the serial application of a GIA stapler to the small bowel loops, providing lengthening of some 50%. Between 2010 and 2014, 3 patients with SBS underwent elective intestinal lengthening using the STEP procedure:
Case 1: A 52-year-old male patient underwent emergency surgery at another hospital for massive intestinal thrombosis secondary to a large stromal tumor. The entire small intestine was resected except for 35cm of the proximal jejunum; terminal jejunostomy, and cecostomy were conducted, conserving practically all of the colon without the ileocecal valve. The lengthening of the jejunum using the STEP method was performed by applying 10 blue cartridges of 45mm linear staples (Endo GIA™, Covidien-Medtronic, Minneapolis, MN, USA) alternately at the mesenteric and anti-mesenteric margins, separated by 3cm, taking special care to preserve the vascularization (Fig. 1). With this, the jejunum was lengthened to about 80cm. A neovalve was created in the distal end using eversion of the loop as in the Brooke ileostomy,5 which was anastomosed by an intussusception in the cecum.
Case 2: A 30-year-old female patient presented with catastrophic antiphospholipid syndrome6 requiring massive bowel resection due to ischemia at some 45cm from the angle of Treitz and about 7cm from the terminal ileum with valve, so a double ostomy was performed. After 2 months, STEP was applied using 12 cartridges, elongating the small intestine up to 95cm and performing a manual end-to-end jejunoileostomy.
Case 3: A 45-year-old male underwent emergency surgery at another hospital for intestinal ischemia, involving right hemicolectomy, extensive bowel resection with 80cm of jejunum and 2 ostomies: terminal jejunostomy and mucosal fistula. Fourteen 45-mm cartridges were applied (creating 130cm of small intestine) and a neovalve was created that was anastomosed to the transverse colon. The patients did not present important postoperative complications; they received PN, enteral nutrition (EN) as well as vitamin supplements, pancreatic enzymes, minerals, oligoelements, codeine and loperamide, as needed. Two to 3 months after reconstruction, the patients no longer required PN and in the mid-term not even EN, after which they followed the dietary recommendations of our nutritionists. After a minimum follow-up of 3 years, the 3 patients are living normal lives with adapted oral intake and 2–3 stools per day, with loperamide and codeine occasionally.
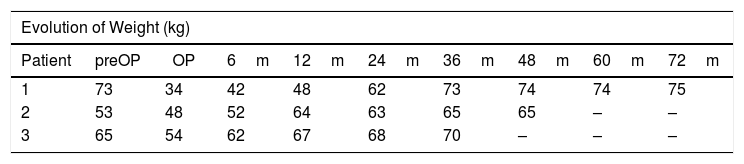
Table 1 shows the weight curve of the patients: prior to SBS, at the time of reconstruction and the evolution over the following months. The STEP technique allows the small intestine to be lengthened in a simple and effective manner, while at the same time resolving the problems caused by dilated loops. In addition, it is possible to repeat the procedure if the bowel is not adapted in an initial intervention. Our group has performed the method in these patients with a technical variation: application of the endostaples on the mesenteric and antimesenteric borders of the intestine, instead of applying them laterally, which provides greater control for stapling and division, while avoiding any gathering in the intestinal loop In the 2 cases in which there were no ileocecal valves, neovalves were created to slow the intestinal transit. In patients with no colon, this neovalve can be affixed to the abdominal wall with some technical modifications, or an enterostomy can also be performed with an inverted loop.
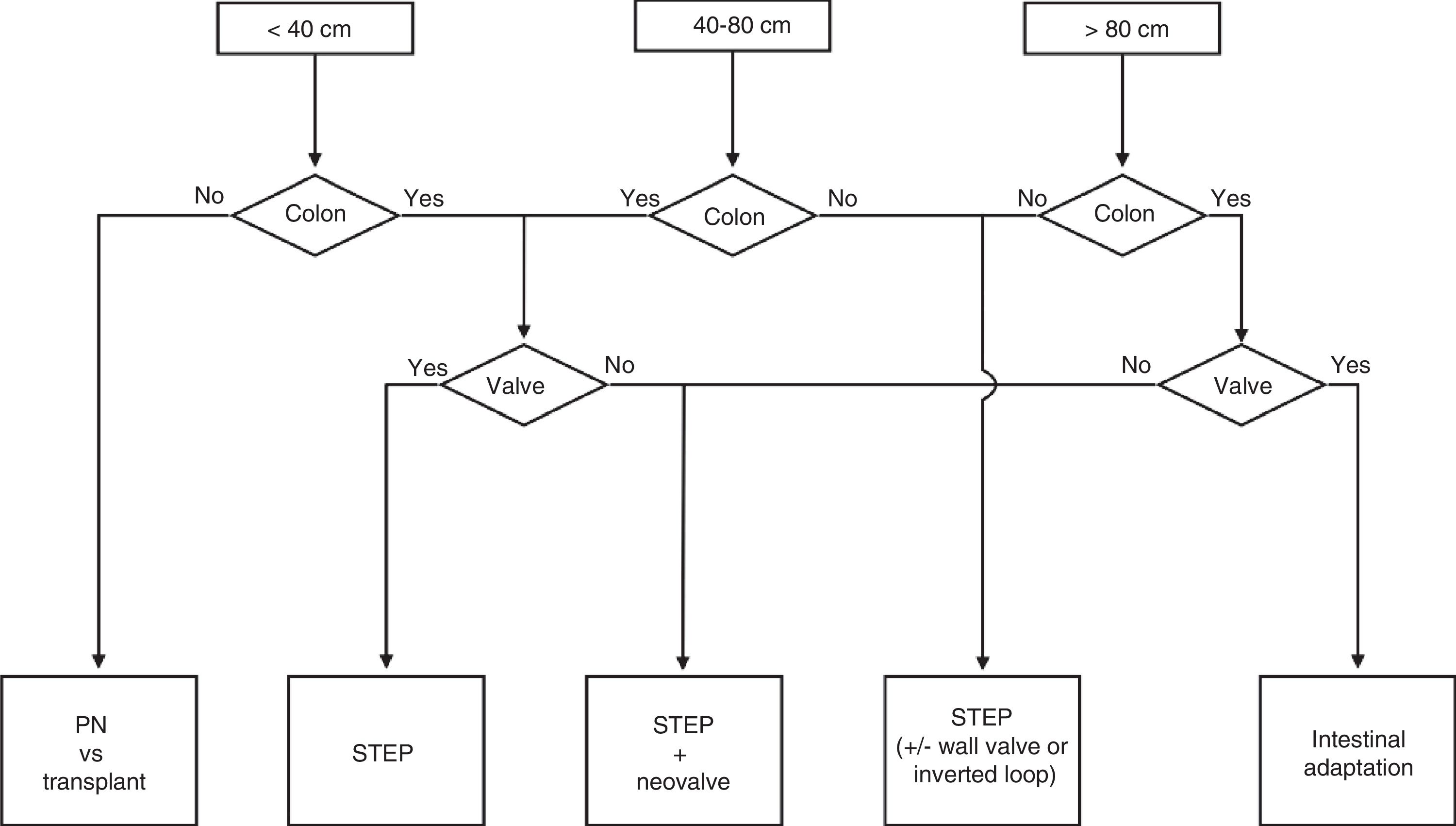
Prophylactic cholecystectomies were also performed in all 3 cases due to the high probability of developing cholelithiasis and its complications in patients with SBS.7 Based on the literature8 and our experience, we propose a technical decision-making algorithm (Fig. 2) depending on the length of the residual intestine and the presence or absence of ileocecal valve and/or colon. The extreme cases would be: (a) a residual intestine of less than 40cm with no colon, where permanent PN or intestinal transplantation will probably be required9 and (b) a residual intestine longer than 80cm with valve and colon, where the intestinal adaptation will surely be achieved without surgery. In the opinion of the authors, the STEP procedure and the eventual creation of a neovalve can achieve enough intestinal adaptation so that the majority of patients with SBS no longer depend on PN. Reducing the number of current candidates for intestinal transplantation and patients requiring permanent/definitive home PN programs has enormous advantages, both economic and medical, especially in terms of survival and quality of life.
Please cite this article as: Alastrué A, Moreno P, Tarascó J, Vela S, Martínez E. Tres casos extremos de síndrome de intestino corto. STEP y neoválvulas. Algoritmo de actuación. Cir Esp. 2018;96:523–525.