Familial adenomatous polyposis is an autosomal dominant hereditary disease characterized by the existence of multiple polyps distributed throughout the intestine, predominantly in the large intestine.1 Outside the colon, they can be located in the duodenum, especially in the ampullary region, requiring large surgeries in cases when their removal is necessary, which has not been possible endoscopically. We present the case of a 47-year-old woman with a history of known classic familial adenomatous polyposis and a previous colectomy with reservoir and terminal ileostomy. The patient was referred to us from the gastroenterology unit for surgical resection of duodenal polyposis that could not be resected endoscopically.
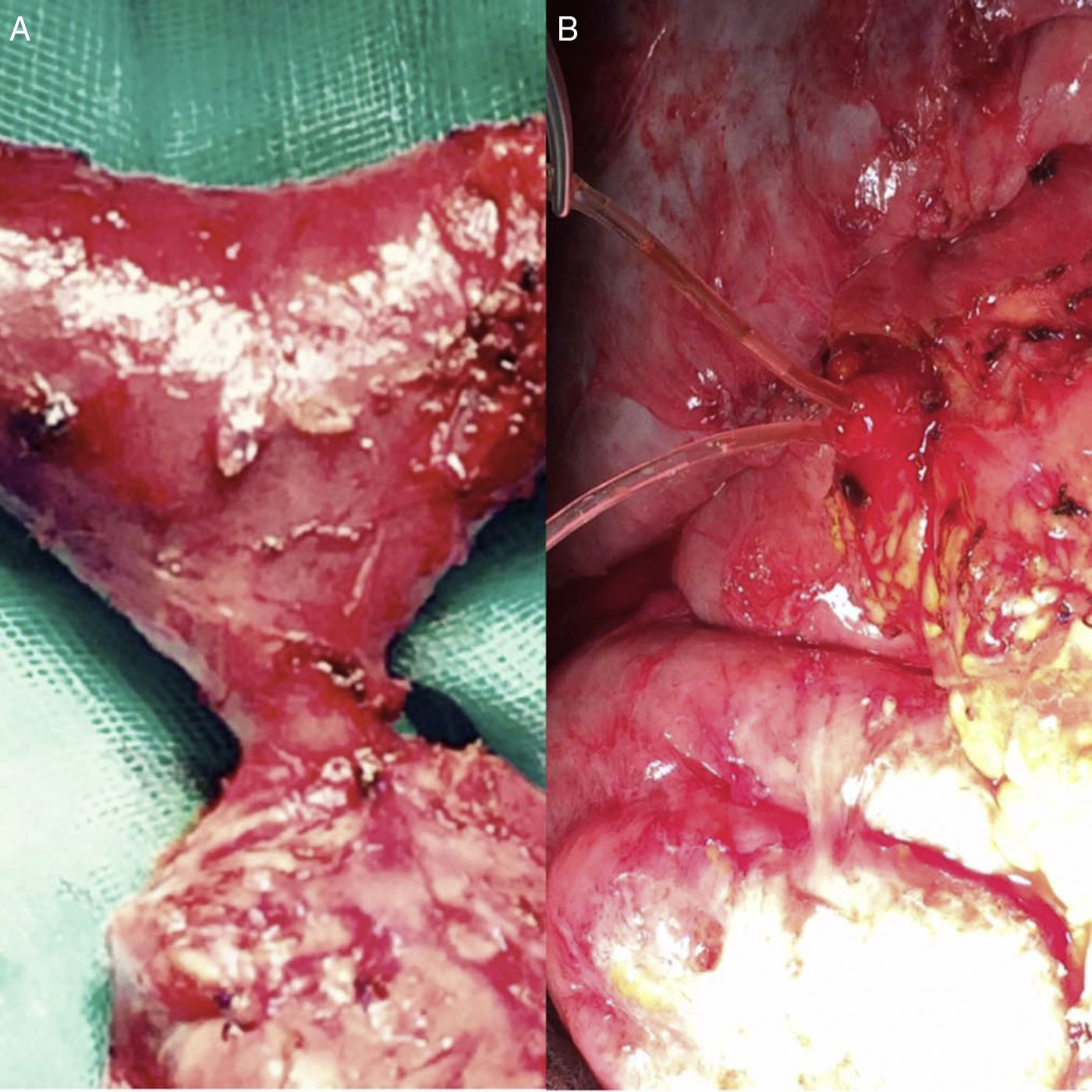
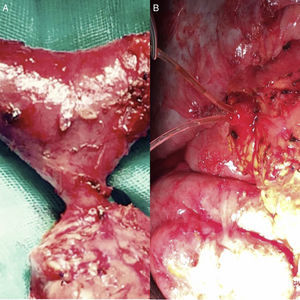
Pancreas-preserving total duodenectomy was performed together with antrectomy and cholecystectomy. During the dissection of the piece, the papilla was individualized (Figure 1) and resected at the base (just below the sphincter), individualizing the pancreatic and biliary ducts, which would remain tutored for weeks (Figure 1B). The reconstruction was done in 2 loops: biliary and pancreatic anastomoses with the first jejunal loop, which ascended behind the mesenteric vessels, end-to-side duct-mucosa, with PDS, tutoring both ducts independently. A jejunal loop was defunctionalized in Roux-en Y-for transmesocolic gastrojejunostomy. The objective of this technique was to isolate the potentially most problematic anastomosis of the digestive tract. The surgical piece from the antroduodenectomy was removed while preserving the pancreatic region (Figure 2).
We ruled out the possibility of performing a duodenectomy with pyloric preservation because with this technique a small portion of the duodenal mucosa is maintained next to the pylorus; the duodenal mucosa should be removed in its entirety, due to the risk of new adenomas (9%). Therefore, we decided that antrectomy was the minimum non-ulcerogenic gastric resection to be performed when the decision was made not to preserve the pylorus.
The pathology diagnosis was tubular adenomas with low-grade dysplasia and low-grade mucosal neoplasm. The postoperative period was uncomplicated and the patient has been asymptomatic during follow-up.
The appearance of extracolonic manifestations throughout the course of this polyposic disease of these patients is frequent, especially in the upper digestive tract and also after resection surgery of the rectum and colon.2 They present an accumulated risk of nearly 90% of developing adenomas in the duodenum, and some 10% of these will develop a duodenal adenocarcinoma3 at the ampullary level.
When endoscopic excision is not possible, radical surgery is necessary4 and, given the location, these patients are classically candidates for extensive resection surgeries, which include the pancreatic head and resection of the distal bile duct, increasing the associated morbidity. Pancreas-preserving duodenectomy is proposed as a surgery with lower morbidity by preserving the head of the pancreas,5 and, therefore, the distal bile duct and the pancreatic duct, thereby decreasing the complications associated with this type of surgeries. It is a complex technique but it offers an alternative to large resections in selected patients.6 Regarding its complications,7 we found delayed gastric emptying, fistulae of the gastrojejunal, pancreaticojejunal and hepatojejunal anastomoses, intra-abdominal abscess and infection of the surgical wound, acute pancreatitis and recurrence (at the level of the post-pyloric cuff or papilla, if the pylorus or papilla are preserved) in 9% of cases. The global complication rate is 60% (25% minor and 35% major) in the few published cases, which is similar to the Whipple technique.8
Given the possibility of a malignant result in the definitive pathology diagnosis, an unlikely event in our case due to the numerous previous biopsies taken endoscopically, we would have been facing a duodenal adenocarcinoma; therefore, pancreatic head resection would have been completed with regional lymphadenectomy if it were an infiltrating adenocarcinoma. In cases of carcinoma in situ, duodenectomy is considered an adequate procedure.9
Please cite this article as: Jiménez Cubedo E, Giménez Alvira L, Jimenez Garrido M, Sánchez Turrión V. Duodenectomía total con preservación pancreática como tratamiento de la poliposis duodenal. Cir Esp. 2018;96:178–180.