More than 10% of patients with unresectable gastric adenocarcinoma present gastrointestinal bleeding either at the time of diagnosis or afterwards.1,2 The resulting symptoms are variable, from progressive anemia due to evident or hidden chronic hemorrhage to hemodynamic shock.1 In any case, the morbidity of these hemorrhages notably worsens the patient’ quality of life. Endoscopic techniques have been seen to be effective for the control of bleeding secondary to gastric cancer and are the first line of treatment. Nonetheless, the incidence of recurrent bleeding reaches 29%–80%, and in many cases there are lesions that are not susceptible to endoscopic control, such as extensive mucous membrane lesions with capillary bleeding, deep ulcers with vessels larger than 2mm, very vascularized tumors with arterial infiltration or lesions that are not accessible endoscopically.2,3 Traditionally, surgery has been the treatment of choice in these cases as it improves the efficacy to control bleeding, although it involves elevated morbidity and mortality.2,4–6 Interventional radiology can be an effective alternative for patients with recurring or persistent hemorrhage after endoscopy.2,3,7
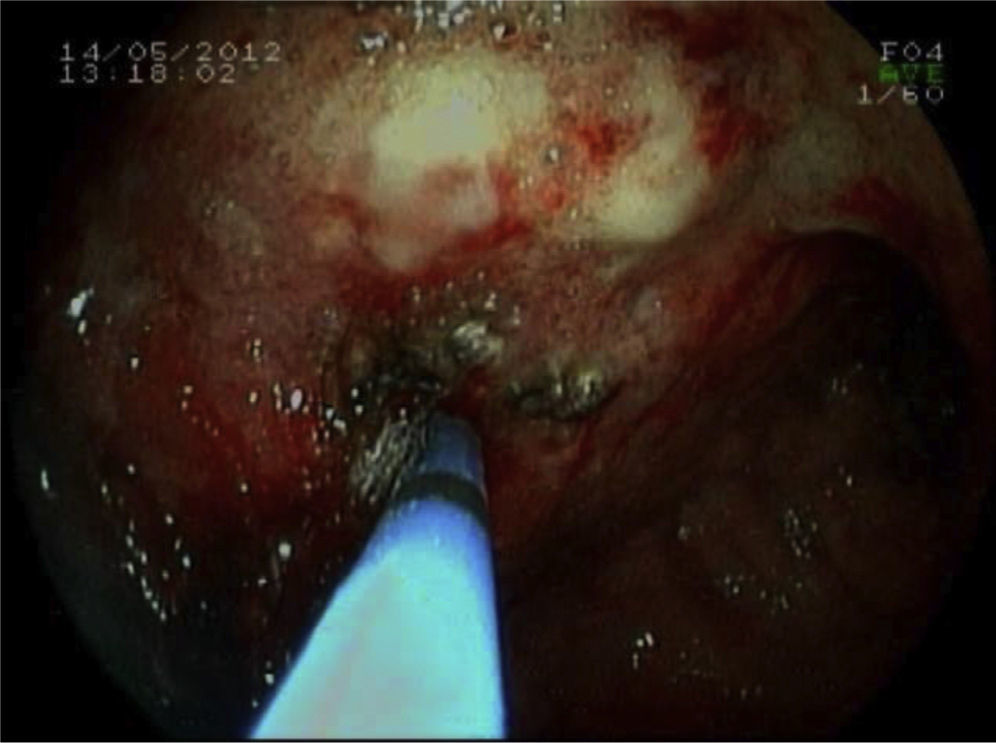
We present the case of a 64-year-old woman diagnosed in April 2012 with locally-advanced gastric adenocarcinoma (body-fundus) cT3N2M0. Neoadjuvant chemotherapy was decided upon. On May 12th, she came to the Emergency Department due to upper gastrointestinal bleeding (UGIB) in the form of melenas, with hemodynamic instability and severe anemia seen on lab work (Hb: 5.9g/dl). Gastroscopy showed evidence of a mamelonated, friable mass that extended from the cardias along the lesser curvature until the incisure, with capillary bleeding (Fig. 1) that was treated with adrenalin (1:10000) and argon fulguration, but hemostasis was not achieved. We decided to perform arterial embolization (Fig. 2) using the selective catheterization of the left gastric artery with particles from 700–900μ and Spongostan™. Good results were seen on the follow-up angiography. After having controlled the hemorrhage, the patient initiated chemotherapy in accordance with the XELOX model. On the follow-up computed tomography done in July 2012, a marked decrease was observed in the wall thickness of the lesser curvature of the stomach in the area of the body and antrum, and the lymphadenopathies had also reduced in size. Nonetheless, multiple new bone metastases were found. The patient died in December 2012 due to disease progression.
Arterial embolization is a safe, effective alternative in these cases of persistent or recurrent hemorrhage, especially in critical patients or those with high risk for surgery. It is a less aggressive technique with fewer complications, and its main advantage is the avoidance of emergency surgery in these patients,4,8 which reaches very high rates of morbidity and mortality.9 In addition, most patients with hemorrhage secondary to gastric cancer are found in advanced stages of the disease, so any type of surgical treatment is usually palliative. Prognosis is poor, with a mean survival of less than a year. The control of active bleeding can improve the clinical course and immediate survival, although the prognosis is determined by tumor stage and progression.2
Even though there are several studies in favor of the use of arterial embolization to control bleeding in peptic ulcers and postoperative pseudoaneurysms with rates of technical and clinical efficacy that range from 69% to 100% and 63% to 97%, respectively, few include gastric cancer and are usually small series.2,4–6,8
The clinical efficacy of embolization for controlling bleeding secondary to gastric cancer ranges between 43% and 75%.2 It is greater in those cases that demonstrate the presence of contrast extravasation on arteriography, followed by those that show uptake of the tumor. Since the hemorrhage is often diffuse or intermittent, it is not rare for the arteriography to be negative in spite of there being active hemorrhage seen on endoscopy. In this context, Lee et al.2 and Shin et al.7 propose that “blind” embolization in these cases, guided by the endoscopic information about the possible origin of the hemorrhage, could be equally beneficial.
Although embolization is considered a safe technique above the ligament of Treitz due to the rich collateral circulation of the stomach and duodenum, the main risk is ischemia and necrosis. There have been case reports of acute ischemia post-embolization. The majority, however, are late-onset and present as duodenal stenosis due to embolization of the gastroduodenal artery,5,6 with a higher risk in patients with a history of radiotherapy or previous gastric surgery.7
Recent studies based on small series have also demonstrated the benefit of radiotherapy as treatment for bleeding in gastric cancer, although there are no studies comparing its efficacy with endoscopic techniques and embolization. Therapy regimes have been used with dose fractions from 30Gy in 10 sessions to 54Gy in 30 sessions, achieving control of the hemorrhage in 55%–75% of the patients who complete the treatment.10 The duration of the hemostatic effect can be approximately 11–12 months and is even greater than that achieved with endoscopic techniques in cases of diffuse hemorrhage. Nonetheless, radiotherapy has limitations in the control of serious acute bleeding (accompanied by hemodynamic instability), given the need for urgent treatment. On the other hand, it can potentially cause gastritis, ulcer and hypochlorhydria (if a significant volume of parietal cells are irradiated). In addition, these consequences can exacerbate nausea, vomiting, dyspepsia, pain and can induce hemorrhage that is not related with the tumor. In this manner, radiotherapy has its role mainly in cases of chronic hemorrhage, where it has been shown to reduce the need for transfusions and improve the quality of life of these patients.
In conclusion, in patients with bleeding gastric cancer that is either unresectable or involves high surgical risk, transcatheter arterial embolization can be a safe and effective technique to control bleeding. Prospective studies are necessary to establish its routine use as an alternative to surgery in the management of these patients when endoscopic techniques have failed.
Please cite this article as: Romera Barba E, Castañer Ramón-Llín J, Sánchez Pérez A, García Marcilla JA, Vázquez Rojas JL. Embolización arterial percutánea en el tratamiento de la hemorragia digestiva secundaria a cáncer gástrico avanzado. Cir Esp. 2014;92:492–494.
Presented as an informational poster at the 23rd National Meeting of ISDE, San Sebastián (Spain) from May 2–3, 2013.