The treatment of anal fistula with the OTSC® (over-the-scope-clip) proctology device involves the placement of an elastic alloy clip called Nitinol on the internal fistula opening to achieve fistula healing. The aim of this study was to analyze preliminary results of this technique in a case series.
MethodsThis was a retrospective analysis of patients who underwent OTSC® clip placement for fistula-in-ano treatment between June 2015 and March 2017 at a specialized colorectal unit. Patients with simple and complex fistulae, either previously treated or not, were included in the study. Both cryptoglandular and stable Crohn's disease fistulae were considered for this approach. Technique failure was determined by the re-appearance of anorectal suppuration or in clip-related complications.
ResultsTen patients were treated surgically for anal fistula with a median age of 54 years (range: 41–70 years). The etiology of the fistulae was mainly cryptoglandular. Three patients had simple fistulae, whereas seven had complex disease. 80% of the patients had already undergone previous fistula surgery. No events occurred during the procedure. The success rate for healing was 60%, with a median follow-up of 15 months (range: 6–26 months). Three patients developed suppuration relapse and one patient required clip extraction due to invalidating anal pain. No fecal incontinence was recorded after the procedure.
ConclusionsThe treatment of anal fistulae with the OTSC® device is a safe sphincter-saving technique in the short term.
El tratamiento de la fístula anal con el dispositivo OTSC®(over-the-scope-clip) consiste en la inserción de un clip de una aleación elástica denominado Nitinol que ejerce una presión constante sobre el orificio fistuloso interno y facilita el cierre de la fístula. El objetivo de este estudio es analizar los resultados a corto plazo de esta técnica en una serie de casos.
MétodosAnálisis retrospectivo de una serie de casos intervenidos de cierre de fístula anal entre junio de 2015 y marzo de 2017 tratados en una unidad especializada con el dispositivo OTSC®. Se incluyeron pacientes con fístulas anales simples y complejas, tratadas previamente o sin tratamientos previos, de origen criptoglandular o por enfermedad de Crohn estable. Se consideró fracaso de la técnica a la supuración anal o complicaciones relacionadas con la inserción del clip.
ResultadosSe intervino a 10 pacientes con fístula anal con una mediana de edad de 54años (rango: 41-70años). Nueve fístulas fueron de origen criptoglandular y una por enfermedad de Crohn controlada. Tres pacientes presentaron fístulas simples y siete, complejas. El 80% de los pacientes habían presentado cirugías anales previas. La tasa de curación de la fístula fue del 60% con un seguimiento mediano de 15meses (rango: 6-26meses). Tres pacientes presentaron recidiva clínica y un paciente requirió extracción del clip por dolor invalidante. No hubo aparición de incontinencia fecal.
ConclusionesEl tratamiento de la fístula anal con el dispositivo OTSC® es una técnica conservadora de esfínteres segura con resultados satisfactorios a corto plazo.
The treatment of fistula-in-ano is a challenge for surgeons. The most effective surgical procedure is fistulotomy. However, in the specific case of complex fistulae, the high risk of fecal incontinence renders this technique inappropriate.1 The therapeutic management of anal fistulae includes the healing of suppuration while preserving sphincter function. Rectal advancement flap has been the most indicated treatment for complex fistulae, with a success rate between 60% and 90% depending on the thickness of the flap and the series, although with a certain degree of residual incontinence.2,3
In recent years, different techniques have been reported focused on treating the fistula orifice or tract without altering the structure of the sphincter apparatus, such as ligation of the intersphincteric fistula tract (LIFT), placement of plugs, fibrin glue, etc.4 There have been recent descriptions of the use of a biocompatible alloy clip called Nitinol inserted using an OTSC® (over-the-scope clip) device, previously used for the endoscopic treatment of fistulae and gastrointestinal bleeding. This clip looks like a claw, with a diameter of 14mm, and its mechanism of action involves exerting constant pressure in the fistulous opening in order to achieve permanent closure of the fistula tract and cessation of drainage.5
The aim of this study is to evaluate the effectiveness of anal fistula treatment with the OTSC® device in a retrospective series of cases.
MethodsPatientsWe present a retrospective series of cases treated at a single hospital (Hospital Universitario Vall d’Hebron) between June 2015 and March 2017 (for a minimum follow-up of 6 months). During this period, 10 patients underwent anal fistula closure using the OTSC® device (Over-the-Scope clip, Ovesco Endoscopy AG, Tübingen, Germany). Fistulae were included in which no previous treatment had been performed as well as recurrent fistulae after other procedures. Patients with Crohn's disease were also included, provided that their baseline disease was controlled.
The fistulae were evaluated and classified by endoanal ultrasound and/or magnetic resonance imaging (MRI) according to the criteria of the treating surgeon. Typically, in complex fistulae that had not been treated previously, endoanal ultrasound was performed, while MRI was requested in cases of recurrence or multiple interventions. Included in the study were patients with complex fistulae who were not candidates for fistulotomy due to potential incontinence, including low transsphincteric fistulae in women, those involving more than 50% of the external anal sphincter, those with secondary tracts or those with more than one tract, and also suprasphincteric fistulae. In cases of complex fistulae that associated intermediate or residual collections or secondary tracts, a seton was placed to condition and redirect the inflammation of the fistulous tract, which was maintained for at least 6 weeks before the clip closure. All the patients gave their informed consent for the procedure, in accordance with hospital protocol.
TechniquePatient preparation included an enema prior to surgery and antibiotic prophylaxis according to the hospital protocol with cefuroxime 1500mg+metronidazole 500mg. The placement of the patient (lithotomy or jackknife) was decided according to the location of the fistulous orifice. In all cases, the first step was to review the fistula orifice and its tract in order to rule out intermediate collections or secondary paths not visualized in the complementary tests. Subsequently, debridement of the fistula tract was performed with a specific fistula brush and lavage.
Once the tract was cleaned, the internal fistula orifice was exposed and a 2cm excision of the anoderm was made so that the clip did not trap the sensitive fibers of the anoderm, thus preventing potential postoperative pain. After excision of the mucosa around the internal fistula orifice, we proceeded to place two sutures through the entire wall thickness that were U-shaped through the internal fistulous orifice to cause the approximation of the defect at the level of the anal sphincter. To this end, resorbable suture material was used. The threads were inserted into a guide of the OTSC® device that helps direct the clip perpendicularly toward the internal fistulous orifice when they are pulled (Fig. 1). Before firing the Nitinol clip, we confirmed that the fistula orifice and the surrounding tissue were inside the tip of the applicator that protected the clip. In other words, the entire internal fistula orifice, closed by the previous transfixion sutures, should be inside the applicator to ensure that the clip covers the entire orifice and does not cause recurrence, as described in the original technique.5
After the placement of the clip, the seal of the internal fistula orifice was tested for leaks by injecting saline solution through the external fistulous orifice. Last of all, the threads that had been previously placed were cut (Fig. 2). In order to improve postoperative drainage, tissue excision of the external fistulous orifice was performed by means of a core-out.5,6
Postoperative care followed the standards of the unit, with oral intake and rescue analgesia. Enemas or suppositories were contraindicated, but laxatives were recommended to ensure soft stools.
Follow-upPatients were monitored in outpatient clinics 10–14 days after the intervention. The correct position of the clip was corroborated with a digital rectal examination, and the state of the external orifice was examined. The appearance of symptoms, such as recurrence of suppuration, perianal discomfort and fecal incontinence, was classified in all patients using the Wexner scale. In the event of improvement, follow-up visits were scheduled for 6 months, 12 and 24 months. The reappearance of symptoms or presence of invalidating anal pain were considered a failure of the technique. In these cases, a revision under anesthesia was scheduled to corroborate the recurrence of fistula or to extract the clip. In cases of failure of the technique, the extraction of the clip was always performed with pliers through a cut in the closure.
Statistical AnalysisThe continuous variables were expressed as median range, while the categorical variables were reported in percentages.
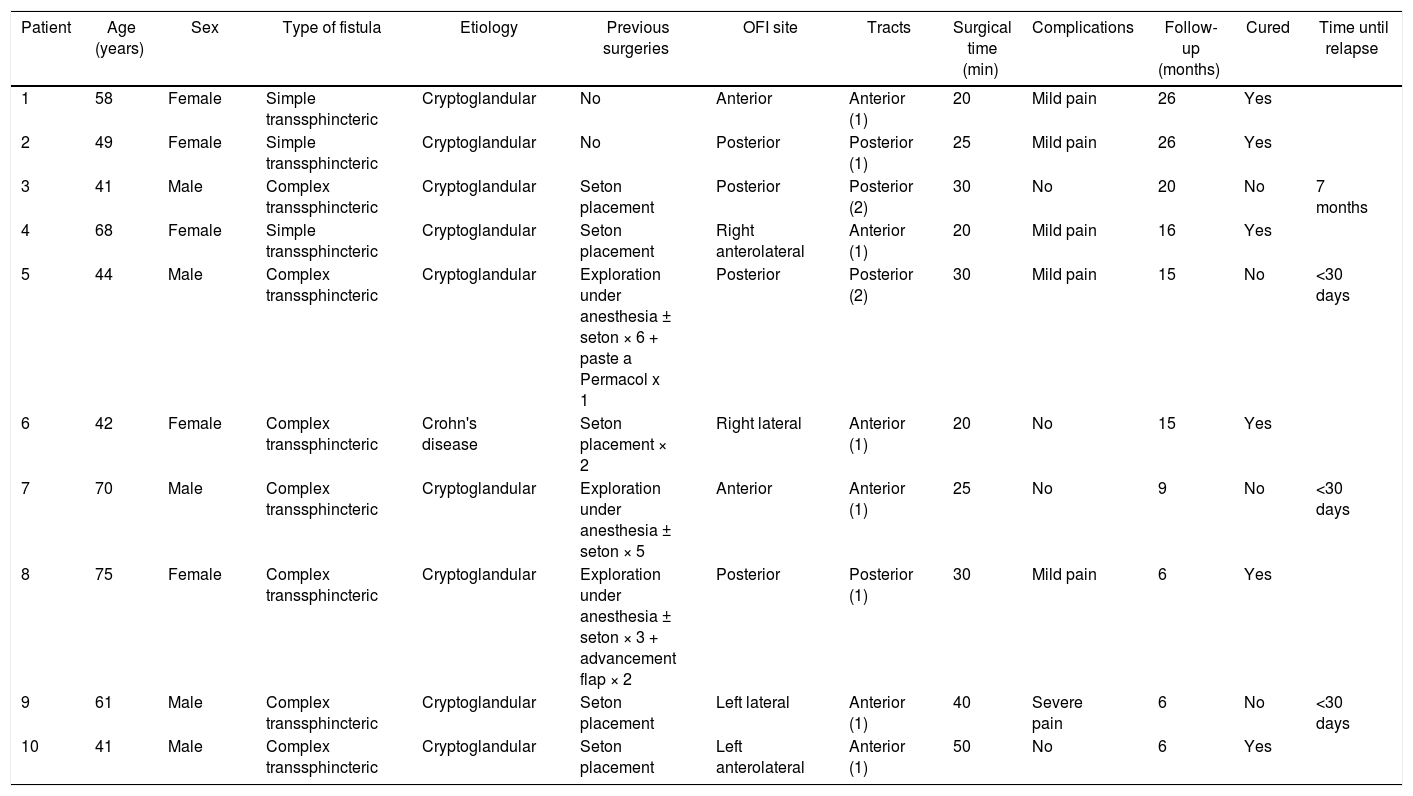
ResultsDuring the study period, 10 patients were treated (5 men and 5 women) with a median age of 54 years (range: 41–70). The most relevant patient characteristics are summarized in Table 1.
Patient Characteristics and Technique Results.
| Patient | Age (years) | Sex | Type of fistula | Etiology | Previous surgeries | OFI site | Tracts | Surgical time (min) | Complications | Follow-up (months) | Cured | Time until relapse |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 58 | Female | Simple transsphincteric | Cryptoglandular | No | Anterior | Anterior (1) | 20 | Mild pain | 26 | Yes | |
| 2 | 49 | Female | Simple transsphincteric | Cryptoglandular | No | Posterior | Posterior (1) | 25 | Mild pain | 26 | Yes | |
| 3 | 41 | Male | Complex transsphincteric | Cryptoglandular | Seton placement | Posterior | Posterior (2) | 30 | No | 20 | No | 7 months |
| 4 | 68 | Female | Simple transsphincteric | Cryptoglandular | Seton placement | Right anterolateral | Anterior (1) | 20 | Mild pain | 16 | Yes | |
| 5 | 44 | Male | Complex transsphincteric | Cryptoglandular | Exploration under anesthesia ± seton × 6 + paste a Permacol x 1 | Posterior | Posterior (2) | 30 | Mild pain | 15 | No | <30 days |
| 6 | 42 | Female | Complex transsphincteric | Crohn's disease | Seton placement × 2 | Right lateral | Anterior (1) | 20 | No | 15 | Yes | |
| 7 | 70 | Male | Complex transsphincteric | Cryptoglandular | Exploration under anesthesia ± seton × 5 | Anterior | Anterior (1) | 25 | No | 9 | No | <30 days |
| 8 | 75 | Female | Complex transsphincteric | Cryptoglandular | Exploration under anesthesia ± seton × 3 + advancement flap × 2 | Posterior | Posterior (1) | 30 | Mild pain | 6 | Yes | |
| 9 | 61 | Male | Complex transsphincteric | Cryptoglandular | Seton placement | Left lateral | Anterior (1) | 40 | Severe pain | 6 | No | <30 days |
| 10 | 41 | Male | Complex transsphincteric | Cryptoglandular | Seton placement | Left anterolateral | Anterior (1) | 50 | No | 6 | Yes |
The origin of the fistula was cryptoglandular in 9 patients. One patient had Crohn's disease controlled with thiopurines. As for fistula type, 30% of the patients presented a simple transsphincteric fistula, while in 70% of the cases the fistula was complex.
60% of the patients presented an anterior fistula and 40% posterior, all with a single tract except in two cases. Among those who presented a simple transsphincteric fistula, in two patients clip placement was indicated without requiring previous surgeries. In the rest of the patients (80%), a seton was inserted in the fistula at the moment of the clip placement. On the other hand, the five cases that presented recurrent fistula had undergone a median of three interventions (range 1–7), including: debridement of the postanal space, seton placement, advancement flaps and placement of Permacol® paste. No patients presented an extra-sphincter fistula or communication to the vagina or urethra.
All surgeries were performed without intraoperative incidents. The median operative time was 28min (range: 20–50min). Four patients were discharged on the same day of the intervention in ambulatory surgery, and the rest after 24–48h.
No patients presented immediate complications after the procedure. Five patients reported mild discomfort during the first days after surgery, which gradually disappeared. Only one patient reported uncontrollable pain from the third postoperative day, even with the prescribed analgesia, requiring early withdrawal of the clip on the tenth day, after which a new seton was placed.
Median follow-up was 15 months (range: 6–26). No patients were lost to follow-up. In addition to the patient who required removal of the clip due to uncontrollable pain, three relapses were detected due to the persistence of suppuration. Two of them were detected in the first month after the placement of the clip; the last was detected in the seventh postoperative month due to partial clip detachment. Out of the four patients in whom failure of the technique was detected, two were reoperated, with an advancement flap in one case and the placement of a plug in the other. No patients reported fecal incontinence during follow-up, regardless of the healing of the fistula.
In patients with failure of the technique, whether due to recurrence or pain, the clip was removed at the time of the next exploration in the operating room. The remaining patients kept the clip without reporting any type of symptoms except for one patient, in whom the clip was removed 2 months after surgery by the patient's choice after confirming that the fistula had healed.
DiscussionThe success rate of the OTSC® device for the treatment of fistula-in-ano in our series was 60%, with a median follow-up of 15 months and no observed complications during the procedure or appearance of fecal incontinence.
The current techniques for the treatment of anal fistula with sphincter preservation are based on the treatment of the internal fistula orifice and/or the fistula tract. The key advantage of this technique lies in constant, dynamic and sustained compression of the metal alloy containing Nitinol on the fistula orifice, keeping it from reopening and favoring the closure of the tract.6 Unlike other techniques, this clip keeps the internal orifice closed despite fibrotic changes, scarring and high anal pressures. There has been ample evidence of the use of this material in procedures with flexible endoscopy for the treatment of fistulae and gastrointestinal bleeding.7
The success rate in our series was 60%, somewhat superior to other non-invasive techniques, such as fibrin injection, plugs or stem cells.8 However, this treatment failed in four patients. In one, the persistence of anal pain led to the withdrawal of the clip. As previously detailed, this technique requires resection of the anal mucosa around the internal fistula orifice to remove all the sensory fibers of the anoderm from the area where the clip is applied. We believe that, in this patient, this resection was not complete even though the closure of the orifice was correct; therefore, it would be a technical error rather than a failure of the clip.
Two patients presented persistence of suppuration in the first 30 days after surgery. In these cases, which had been previously treated a total of seven and five occasions, respectively, the clip was an alternative and innovative plan that did not take into account the fibrotic environment on which the technique had to be performed. There was a fourth patient in whom clip failure was observed 7 months after placement. Both in this case and in the patient in whom the clip was removed due to the presence of pain after placement, the fistula was able to be resolved by other techniques. Therefore, the OTSC® device is a technique that does not prevent performing other procedures in case of failure. In addition, despite exerting constant pressure on the internal anal sphincter, fecal incontinence did not occur in any patient, regardless of the cure rate.
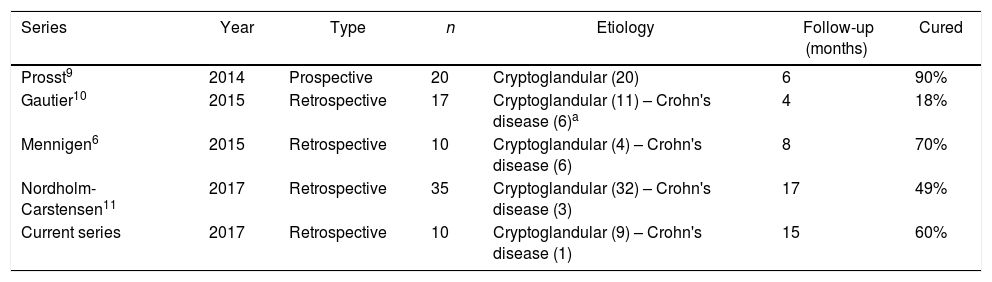
As shown in Table 2, the published evidence about the use of OTSC® is scarce and has a short follow-up. Its success rate varies from 18% to 90%.6,9–11 It should be borne in mind that the study by Gautier et al.,10 which published the worst success rate, reported a series of very unfavorable cases. Among these were seven patients with rectovaginal fistulae and one patient with recto-urethral fistula who had received prior radiotherapy were included. None of the treatments available in our therapeutic arsenal have high chances of success in such complex cases.
Summaries of Published Series About the OTSC® Proctologic Clip.
| Series | Year | Type | n | Etiology | Follow-up (months) | Cured |
|---|---|---|---|---|---|---|
| Prosst9 | 2014 | Prospective | 20 | Cryptoglandular (20) | 6 | 90% |
| Gautier10 | 2015 | Retrospective | 17 | Cryptoglandular (11) – Crohn's disease (6)a | 4 | 18% |
| Mennigen6 | 2015 | Retrospective | 10 | Cryptoglandular (4) – Crohn's disease (6) | 8 | 70% |
| Nordholm-Carstensen11 | 2017 | Retrospective | 35 | Cryptoglandular (32) – Crohn's disease (3) | 17 | 49% |
| Current series | 2017 | Retrospective | 10 | Cryptoglandular (9) – Crohn's disease (1) | 15 | 60% |
On the other hand, the first series published by Prosst et al.9 included highly selected patients with fistulae exclusively of cryptoglandular origin, with a success rate of 90%, although with a follow-up of 6 months. It is likely that the exclusion of patients with inflammatory disease, more than one orifice or fistula tract, anovaginal fistulae, or with previous surgical treatments, has contributed to the success reported by these authors. In addition, there is a possible bias as these authors are the first to propose the use of OTSC® in fistula-in-ano and actively participate in the design of anal placement material.
Due to the type of patients included, our series is more similar to those reported by Mennigen et al.6 and Nordholm-Carstensen et al.11 They included fistulae in patients with controlled Crohn's disease and patients who underwent other previous surgical treatments, and their success rate varied between 49% and 70%. In these series, no problems were reported in the adaptation to a foreign body anchored in the anal region in the form of chronic pain, incontinence or dyspareunia. However, pending further evidence, the use of this device is not recommended in low fistulae, in which case fistulotomy can be beneficial.11
All available publications, including ours, report a retrospective series of cases with differences in both patient selection and follow-up. Currently, a clinical trial in the recruitment phase will randomize patients to undergo advancement flap versus the placement of an OTSC® clip. It is expected that this study will provide a greater degree of evidence when establishing the indications of this technique.12
We are aware that our study has limitations. It is a short, retrospective series that includes heterogeneous fistulae, and some of them are unmanageable with surgical treatment. In addition, the follow-up is short, so this does not rule out that recurrences may appear in the future. Nevertheless, the available data suggest that closure of the fistula orifice with the OTSC® device is a safe sphincter-conserving technique and that it has good initial results in selected patients.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Marinello F, Kraft M, Ridaura N, Vallribera F, Espín E. Tratamiento de la fístula anal mediante clip con el dispositivo OTSC®: resultados a corto plazo. Cir Esp. 2018;96:369–374.