Presacral bleeding (PB) is a non-pulsatile haemorrhage due to the disruption of the presacral venous plexus (PVP). These haemorrhages are difficult to manage and are sometimes non-controllable with conventional surgical manoeuvres.1 The use of tamponade balloons is suggested as a feasible and effective option.
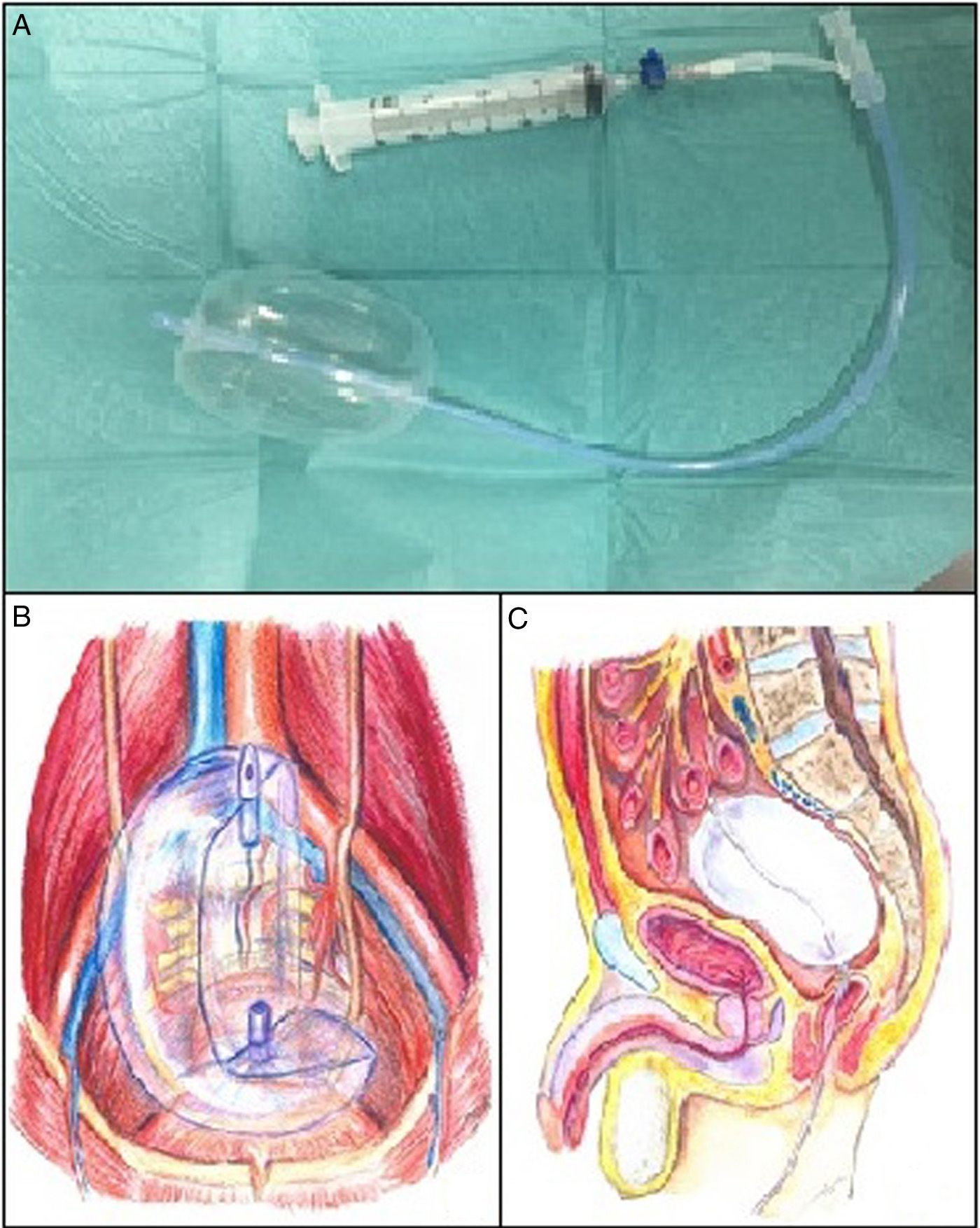
The Bakri balloon is a silicone balloon designed for the treatment of uterine bleeding in postpartum haemorrhage2 (Fig. 1). In our series, the balloons were inserted vaginally, in perineal wounds after rectal resection or anally through the open rectal stump and filled with sterile saline solution (maximum capacity 500mL).
The first patient underwent surgery for disease recurrence in the rectovaginal septum after resection for sigmoid adenocarcinoma. The operation involved hysterectomy and bilateral adnexectomy, resection of the posterior vaginal wall and resection of the rectum with a colorectal mechanical anastomosis and loop ileostomy. On the 5th day post-op, the patient was re-operated on due to anastomotic leak and the remaining colonic segment was resected up to the efferent loop of the ileostomy, presenting PB that required packing. Seven days after this reoperation, the packing material was removed but, 7 days later, the patient once again underwent surgery for suspicion of another PVP haemorrhage. The approach was vaginal, and 3 balloons were inserted vaginally.
The second patient was treated surgically for disease recurrence in the right hemipelvis after abdominoperineal resection due to rectal adenocarcinoma. Surgery involved midline laparotomy with tumour resection. During surgery, PB began that was not controllable by electrocoagulation, suture or haemostatic biological materials, so a balloon was inserted through the perineum.
The third patient, with a history of subtotal colectomy due to familial adenomatous polyposis and an ileal pouch done at another hospital (without proctectomy), presented a tubular adenoma with high-grade dysplasia in the rectal stump 5 years later. Surgery involved midline laparotomy with division of the ileum above the pouch plus resection of the rectum up to the pectinate line and associated ileostomy in the RIF. During the postoperative period, the patient presented several episodes of anal bleeding; relaparotomy was therefore performed, which identified bleeding of the PVP that did not cease with conventional surgical manoeuvres and required the placement of 2 balloons through the non-functioning anus.
The fourth patient was diagnosed with a vascular malformation in the right pelvis who reported metrorrhagia, rectal bleeding and haematuria, which required vascular embolisation. Endoscopy revealed an anal ulcer measuring 20cm, suggesting ischaemic colitis. The patient underwent hysterectomy, bilateral adnexectomy and division of the distal rectum at the pelvic floor and proximal sigmoid colon, closure of the rectal stump and terminal colostomy. On the 2nd day post-op, the patient presented haemoperitoneum and a haemorrhage was found at the PVP. Haemostasis techniques used included electrocoagulation and biologic haemostatic agents, but, given the persistent bleeding, 2 balloons were inserted anally (Table 1).
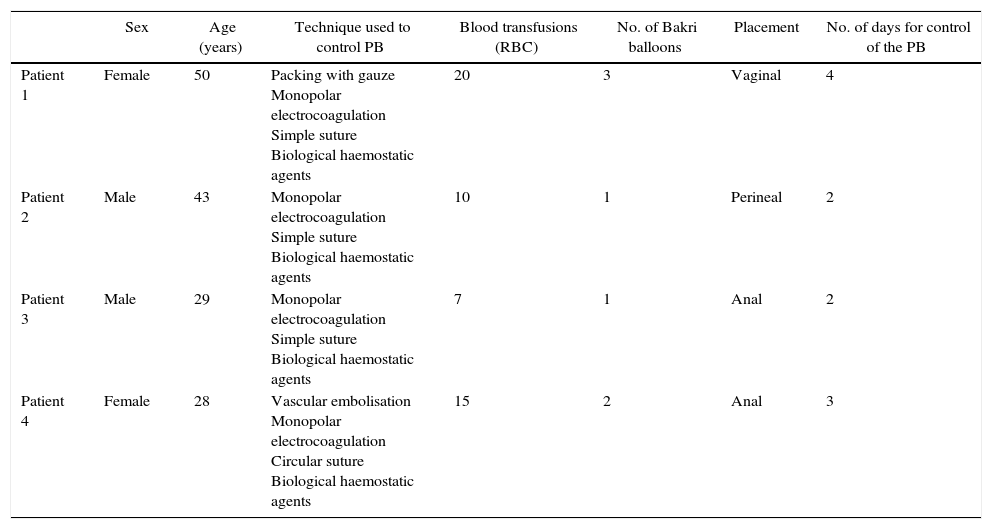
Characteristics of Patients With Presacral Venous Bleeding.
| Sex | Age (years) | Technique used to control PB | Blood transfusions (RBC) | No. of Bakri balloons | Placement | No. of days for control of the PB | |
|---|---|---|---|---|---|---|---|
| Patient 1 | Female | 50 | Packing with gauze Monopolar electrocoagulation Simple suture Biological haemostatic agents | 20 | 3 | Vaginal | 4 |
| Patient 2 | Male | 43 | Monopolar electrocoagulation Simple suture Biological haemostatic agents | 10 | 1 | Perineal | 2 |
| Patient 3 | Male | 29 | Monopolar electrocoagulation Simple suture Biological haemostatic agents | 7 | 1 | Anal | 2 |
| Patient 4 | Female | 28 | Vascular embolisation Monopolar electrocoagulation Circular suture Biological haemostatic agents | 15 | 2 | Anal | 3 |
RBC: packed red blood cells; PB: presacral bleeding.
PB is a serious complication of pelvic tumour surgery (rectal, advanced ovarian and presacral tumours), with an incidence of 3%–9% and a mortality rate of 1%–4%.3
Monopolar electrocoagulation or suture can even aggravate PVP lesions and bleeding.4 The use of surgical clips can be effective, although disadvantages include chronic pain and displacement or difficult placement due to the anatomic curvature of the sacrum.3 Compression with a fragment of anterior rectus muscle and indirect electrocoagulation with monopolar forceps can achieve haemostasis, although this is not recommended for large haemorrhages or if there is contraction of the vertebral vein endings.5 In these cases, bipolar coagulation seems more effective. Electrocauterisation through the epiploic appendices is useful when the origin is due to involvement of the basivertebral veins in a sacral nerve foramen.1 Jiang et al.6 described the circular suture of the PVP in the intact presacral fascia that surrounds the haemorrhage, although this is difficult in a narrow pelvis, previous rectal surgery or atypical anatomic pattern of the PVP. Other alternatives, such as biological haemostatic agents, are widely used but are ineffective in a massive PB.7 Traditionally, packing has been used, but the need for re-operation to remove it is a disadvantage.8
McCourteny et al.9 used a Sengstaken–Blakemore balloon to control a massive PB, with resolution of the haemorrhage 4 days later. Recently, Charoenkwan described the usefulness of the Bakri balloon for untreatable pelvic floor haemorrhage after hysterectomy or caesarean section when other techniques have failed.10
In our experience, the Bakri balloon has been shown to be a useful method in the management of PB after colorectal surgery when conventional treatment has failed. Its advantage is its easy placement and good adaptation to the presacral space while exerting greater intraluminal pressure than the pressure of the venous and capillary system. For its removal, surgical re-operation is not necessary. In fact, when poor haemorrhage control is still suspected, this technique enables us to reduce the pressure gradually and even re-fill the balloon in cases of persistent bleeding.
Please cite this article as: Lopez-Lopez V, Abrisqueta J, Lujan J, Ferreras D, Parrilla P. Tratamiento de la hemorragia presacra tras cirugía colorrectal mediante el uso del balón de Bakri. Cir Esp. 2016;94:303–305.