This article reviews the most relevant ultrasound findings associated with gallbladder cancer.
Materials and methodsA descriptive and retrospective study was made of clinical features and imaging studies in patients subjected to surgery for gallbladder neoplasm in the Reina Sofía General University Hospital (Murcia) during the time period 2000–2011.
ResultsA total of 15 cases of gallbladder cancer were found during the study period, 9 of whom were women. The mean age was 77 years (range 61–96). Pain was the principal complaint. The patients had cholelithiasis in 13 cases, smoking in 2 cases, and obesity in 3 cases. The ultrasound showed gallbladder wall thickening (>4mm) in 8 cases, intraluminal mass in 4, scleroatrophic gallbladder in 2, and mass replacing the gallbladder in one. Only in 4 cases was the suspicion of gallbladder carcinoma established preoperatively. According to the pTNM staging, 4 patients were carcinoma in situ (Tis), one case T1a, 6 cases T2, 3 cases T3 and one case T4. In 7 cases, the only evidence was the preoperative ultrasound, and in 8 the study was completed with an abdominal CT.
ConclusionEarly diagnosis of gallbladder cancer is rare. The ultrasound diagnostic approach is difficult; only a localized thickening coexisting with gallstones seems to be significant, and requires a biopsy. The image of a mass and a stone occupying the gallbladder is associated with later stages of the disease.
Revisar los hallazgos ecográficos más relevantes asociados al cáncer de vesícula biliar.
Material y métodoEstudio descriptivo y retrospectivo de las características clínicas y estudios de imagen en pacientes con neoplasia de vesícula biliar en el periodo 2000-2011 en el Hospital General Reina Sofía de Murcia.
ResultadosFueron hallados 15 casos de cáncer vesicular, de los que 9 eran mujeres. La edad media fue 77 años (rango 61-96). El dolor fue el principal motivo de consulta. Presentaban colelitiasis 13 casos, tabaquismo 2 casos y obesidad 3 casos. La ecografía comprobó engrosamiento de la pared vesicular (>4mm) en 8 casos, masa intraluminal en 4, vesícula escleroatrófica en 2 y masa que reemplaza la vesícula en uno. Solo en 4 casos hubo la sospecha preoperatoria de carcinoma vesicular. Siguiendo la estadificación pTNM, 4 pacientes presentaban un carcinoma in situ (Tis), un caso T1a, 6 casos T2, 3 casos T3 y un caso T4. En 7 casos, la única prueba radiológica preoperatoria fue la ecografía y en otros 8 se completó el estudio con una TC abdominal.
ConclusiónEl diagnóstico precoz del cáncer vesicular es raro. La orientación diagnóstica por ecografía es limitada; solo el engrosamiento parietal localizado coexistente con litiasis vesicular parece significativo en estadios tempranos. La imagen de masa y cálculo ocupando la vesícula se asocia a etapas avanzadas de la enfermedad.
Gallbladder neoplasms are rare in our clinical environment and are associated with high mortality and poor prognosis, principally because they are diagnosed and treated at an advanced stage.1,2 The neoplasm most frequently affects the fundus and body of the gallbladder and along with its non-specific, late clinical presentation which is comparable to other more common disorders–such as biliary colic or cholecystitis–this often results in delayed diagnosis.3 There are few therapeutic possibilities: radiotherapy and chemotherapy are largely ineffective4; radical surgery with lymphadenectomy is currently the only treatment which offers possibilities of long-term survival in selected cases.1,2,5
Abdominal ultrasound is frequently the first imaging test used to examine the gallbladder. The early recognition of ultrasound signs that are traditionally associated with gallbladder neoplasm would enable the surgeon to contribute towards improving the prognosis of the disease. The aim of this article is to review the ultrasound findings associated with early and advanced stages of gallbladder cancer, as well as to identify the elements in ultrasound imaging which could have achieved a diagnosis of suspected disease.
Materials and MethodsA descriptive and retrospective study was performed by reviewing the clinical histories of patients with a diagnosis on discharge of gallbladder cancer, with ultrasound and histological confirmation, treated in the General University Reina Sofía Hospital in Murcia between 2000 and 2011. This selection was made from the Documentation Service database, including patients who had been given a gallbladder cancer code (C23) according to the International Classification of Diseases (ICD)-10. The study protocol was approved by the centre's research committee.
Since only patients with histological confirmation were included in the study, those with clear ultrasound diagnosis of extravesicular tumour spread (such as liver metastases or lymphadenopathies), and false positive ultrasound scans with suspicion of neoplasm were not included. In this regard, the study could be considered limited.
Clinical parameters (age, gender, risk factors, symptoms and signs of the disease and clinical diagnosis), together with the imaging tests performed are shown in Table 1. We used the Tumour Node Metastasis (TNM) classification from the American Joint Committee on Cancer (AJCC)6 for primary tumour staging. Prognosis was based on surgery which would vary depending on the depth of tumour infiltration of the gallbladder wall (T). The main clinical and ultrasound findings were described and correlated with the histology and the stage of the disease in each case.
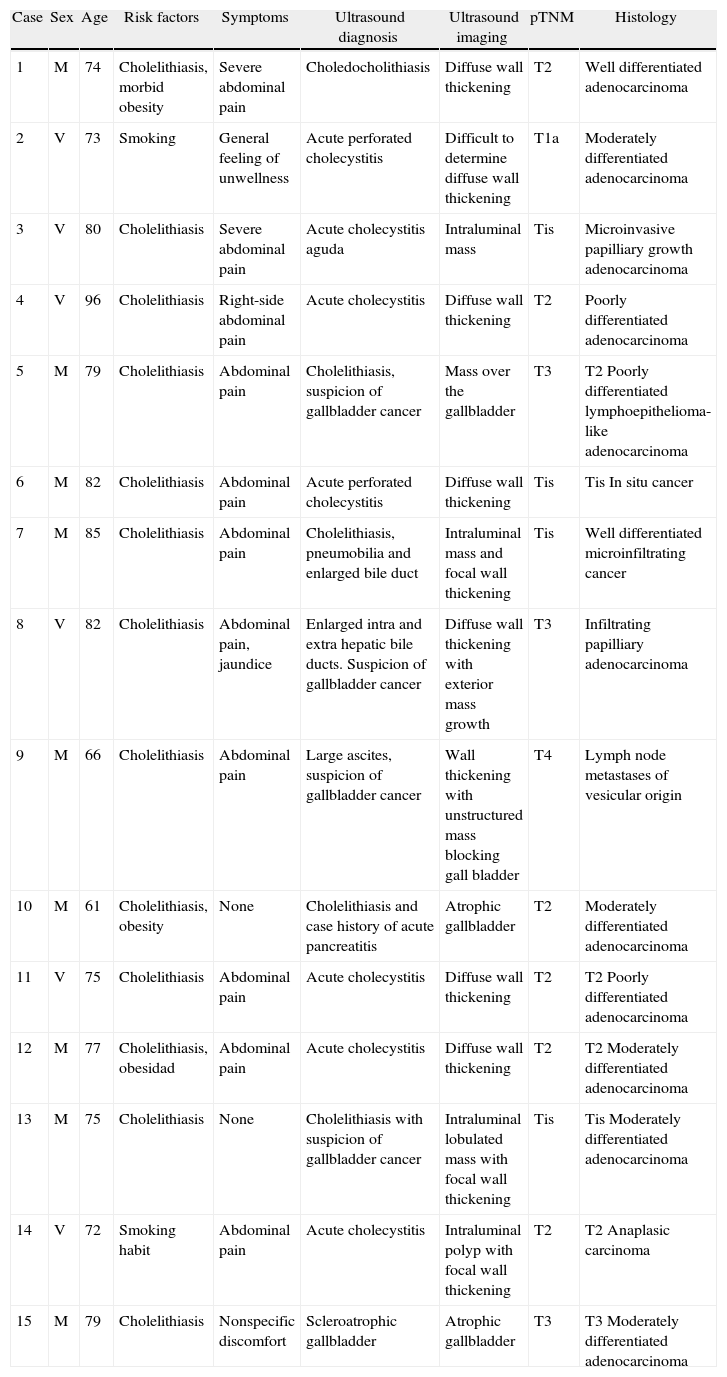
Clinical Data, Scan Findings, pT, Post Cholecystectomy and Type of Tumour.
| Case | Sex | Age | Risk factors | Symptoms | Ultrasound diagnosis | Ultrasound imaging | pTNM | Histology |
| 1 | M | 74 | Cholelithiasis, morbid obesity | Severe abdominal pain | Choledocholithiasis | Diffuse wall thickening | T2 | Well differentiated adenocarcinoma |
| 2 | V | 73 | Smoking | General feeling of unwellness | Acute perforated cholecystitis | Difficult to determine diffuse wall thickening | T1a | Moderately differentiated adenocarcinoma |
| 3 | V | 80 | Cholelithiasis | Severe abdominal pain | Acute cholecystitis aguda | Intraluminal mass | Tis | Microinvasive papilliary growth adenocarcinoma |
| 4 | V | 96 | Cholelithiasis | Right-side abdominal pain | Acute cholecystitis | Diffuse wall thickening | T2 | Poorly differentiated adenocarcinoma |
| 5 | M | 79 | Cholelithiasis | Abdominal pain | Cholelithiasis, suspicion of gallbladder cancer | Mass over the gallbladder | T3 | T2 Poorly differentiated lymphoepithelioma-like adenocarcinoma |
| 6 | M | 82 | Cholelithiasis | Abdominal pain | Acute perforated cholecystitis | Diffuse wall thickening | Tis | Tis In situ cancer |
| 7 | M | 85 | Cholelithiasis | Abdominal pain | Cholelithiasis, pneumobilia and enlarged bile duct | Intraluminal mass and focal wall thickening | Tis | Well differentiated microinfiltrating cancer |
| 8 | V | 82 | Cholelithiasis | Abdominal pain, jaundice | Enlarged intra and extra hepatic bile ducts. Suspicion of gallbladder cancer | Diffuse wall thickening with exterior mass growth | T3 | Infiltrating papilliary adenocarcinoma |
| 9 | M | 66 | Cholelithiasis | Abdominal pain | Large ascites, suspicion of gallbladder cancer | Wall thickening with unstructured mass blocking gall bladder | T4 | Lymph node metastases of vesicular origin |
| 10 | M | 61 | Cholelithiasis, obesity | None | Cholelithiasis and case history of acute pancreatitis | Atrophic gallbladder | T2 | Moderately differentiated adenocarcinoma |
| 11 | V | 75 | Cholelithiasis | Abdominal pain | Acute cholecystitis | Diffuse wall thickening | T2 | T2 Poorly differentiated adenocarcinoma |
| 12 | M | 77 | Cholelithiasis, obesidad | Abdominal pain | Acute cholecystitis | Diffuse wall thickening | T2 | T2 Moderately differentiated adenocarcinoma |
| 13 | M | 75 | Cholelithiasis | None | Cholelithiasis with suspicion of gallbladder cancer | Intraluminal lobulated mass with focal wall thickening | Tis | Tis Moderately differentiated adenocarcinoma |
| 14 | V | 72 | Smoking habit | Abdominal pain | Acute cholecystitis | Intraluminal polyp with focal wall thickening | T2 | T2 Anaplasic carcinoma |
| 15 | M | 79 | Cholelithiasis | Nonspecific discomfort | Scleroatrophic gallbladder | Atrophic gallbladder | T3 | T3 Moderately differentiated adenocarcinoma |
Of the 15 cases included in the study, 9 were women and 6 were men. All the patients were Caucasian, with a mean age of 77 (range 61–96). They presented with associated risk factors of: cholelithiasis in 13 cases, a smoking habit in 2 cases, and obesity in 3 cases.
In terms of clinical history, the most usual reason for consultation was abdominal pain that was present in 11 cases, although 2 patients had no discomfort. Clinical symptoms were: fever (4 cases), weight loss (4 cases), jaundice (3 cases) and abdominal swelling (one case). Ultrasound imaging supported the diagnosis of acute cholecystitis preoperatively in seven cases, 4 cases of suspected gallbladder cancer prior to surgery and another 4 were diagnosed with simple cases of cholelithiasis.
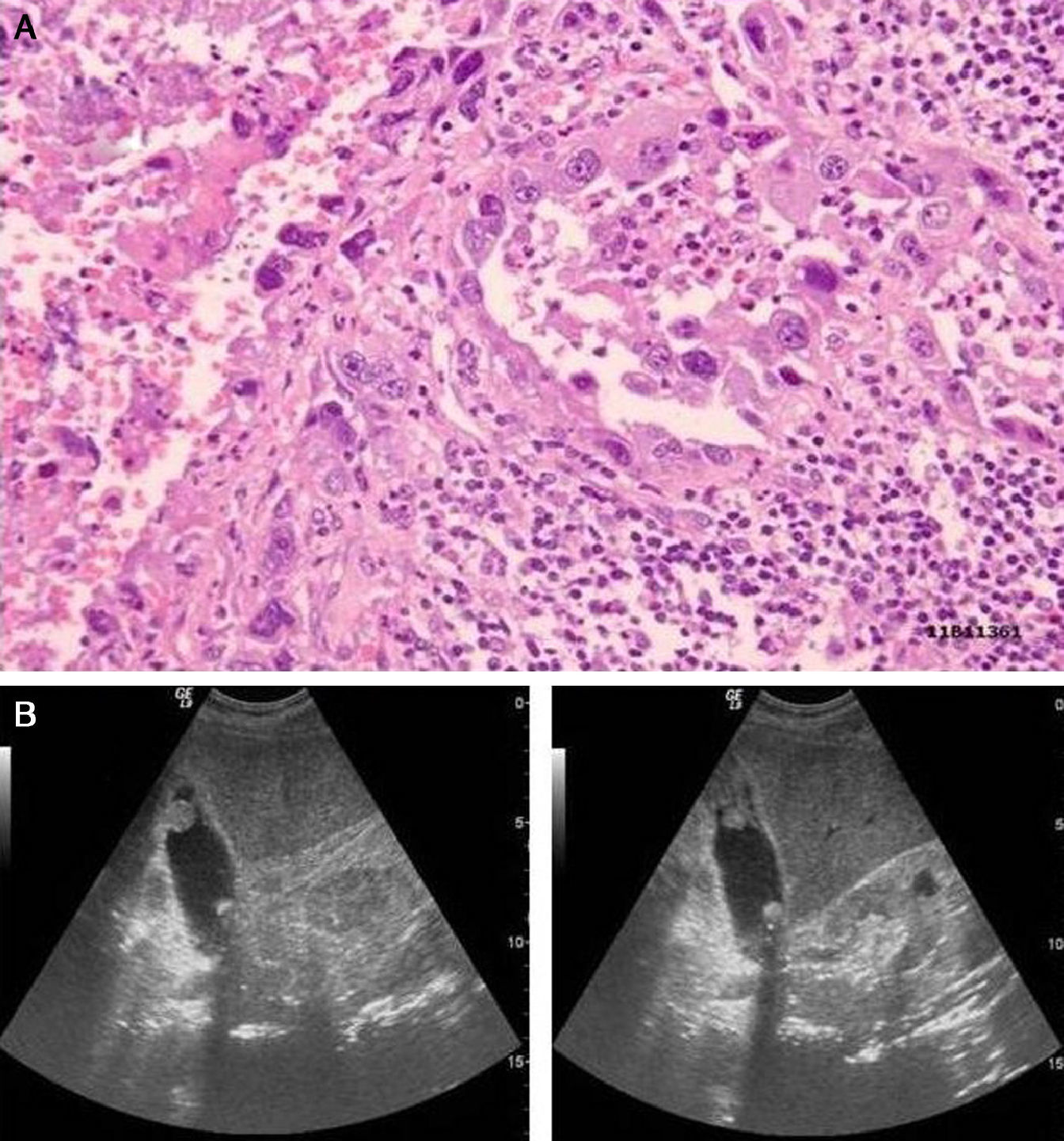
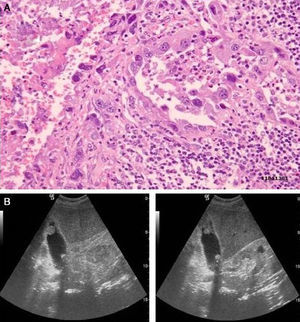
With regard to the histology, the most frequent tumour in our study was adenocarcinoma, recorded in 12 cases, one case of anaplastic carcinoma (Fig. 1) and another of a lymphoepithelioma-like carcinoma. In one case the pathological report only refers to gallbladder metastases.
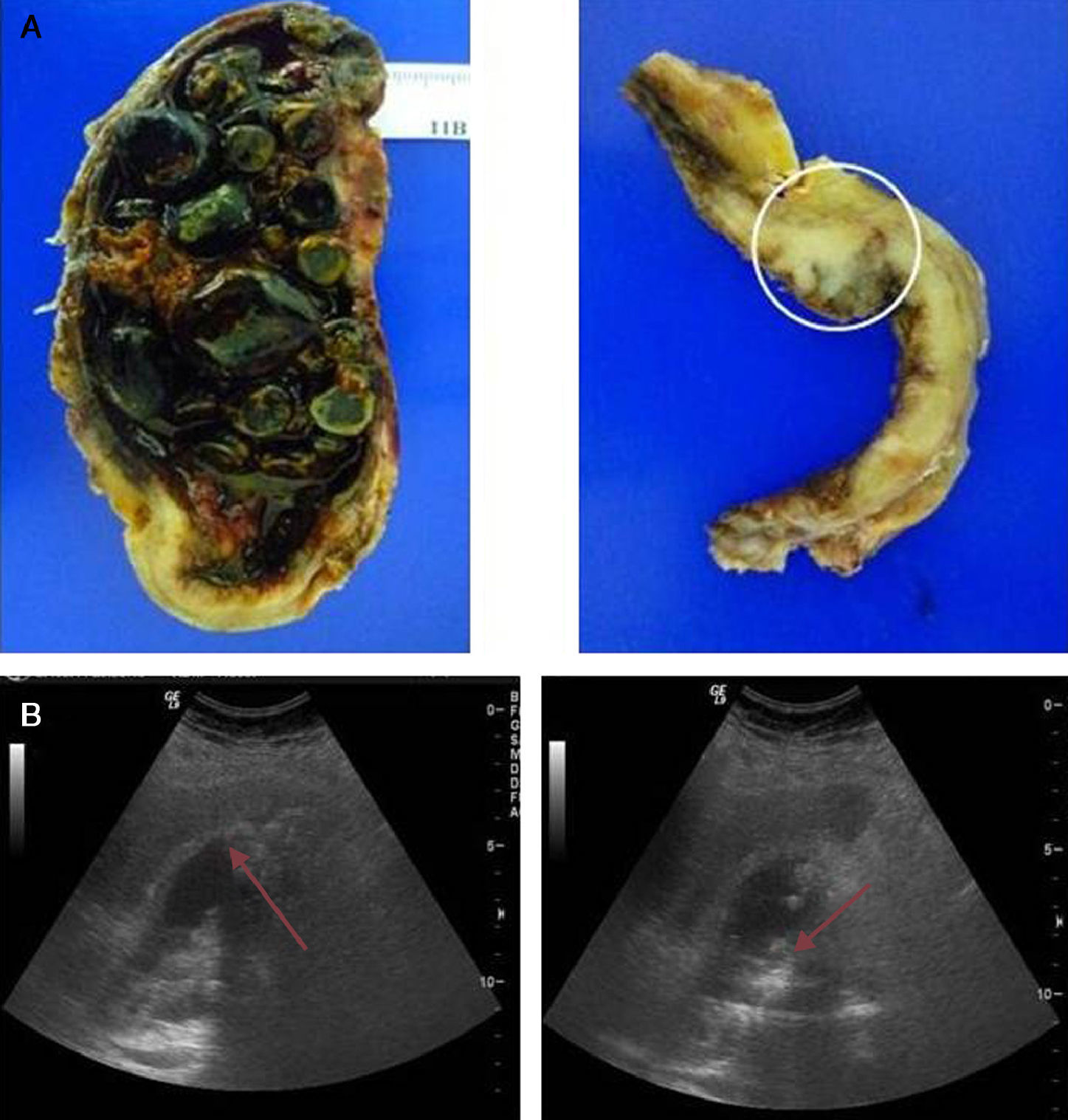
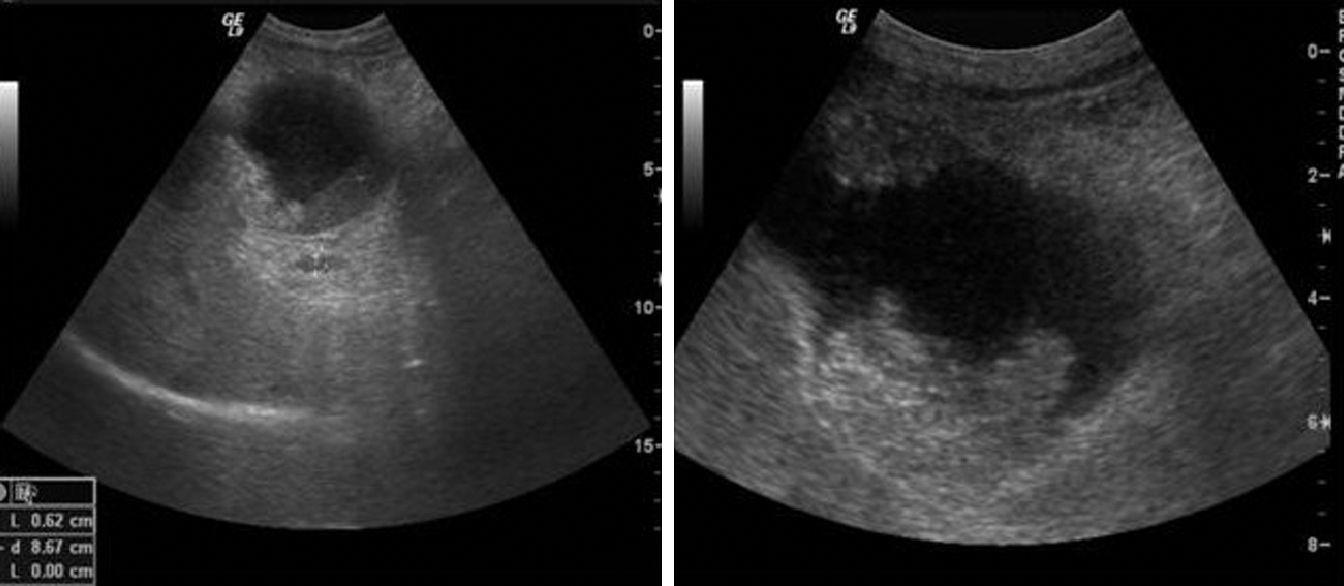
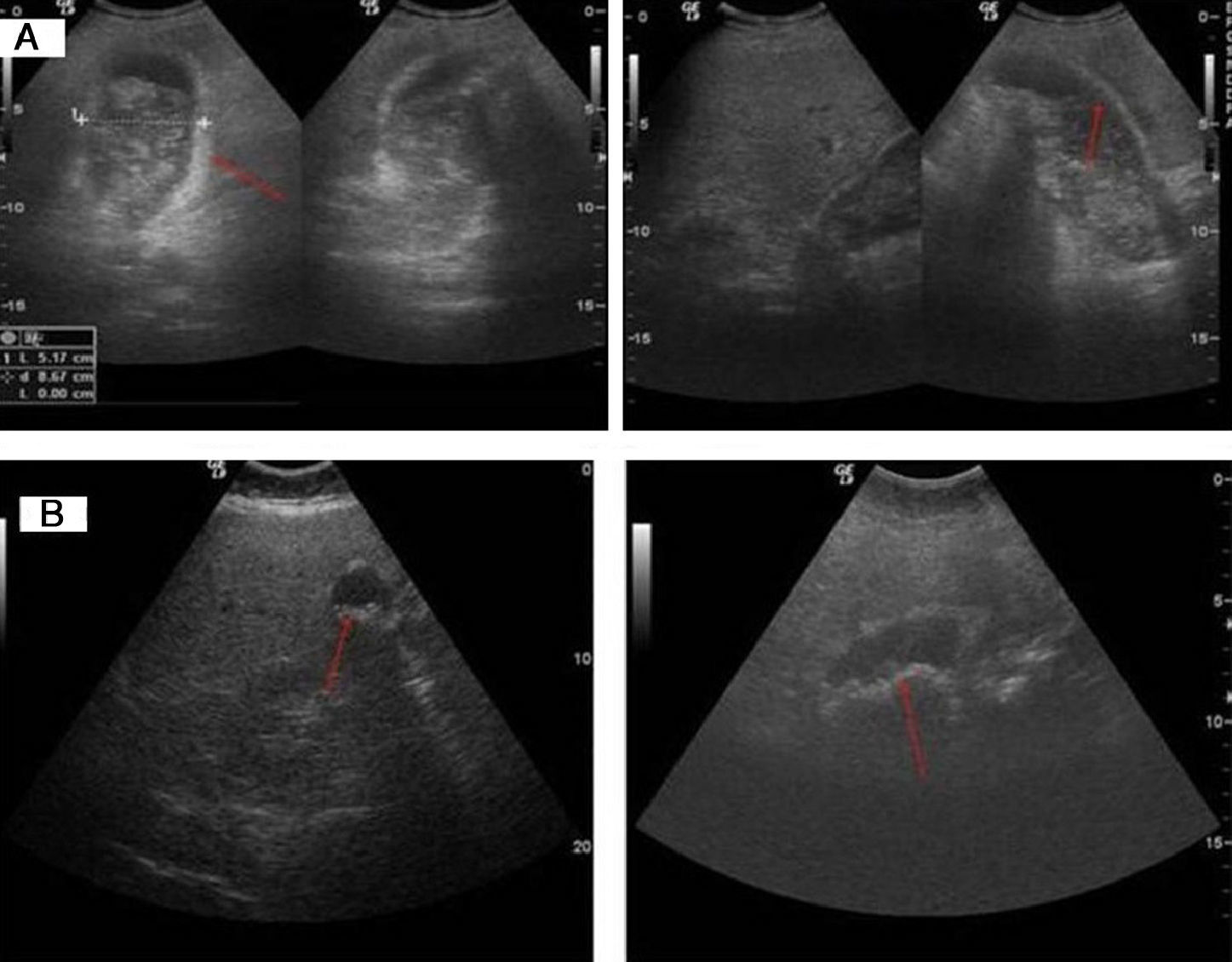
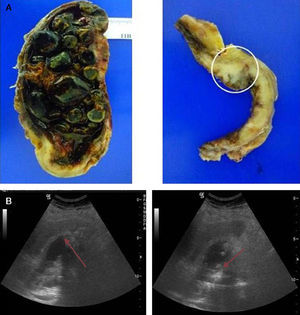
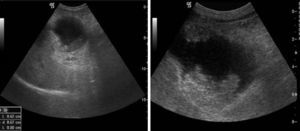
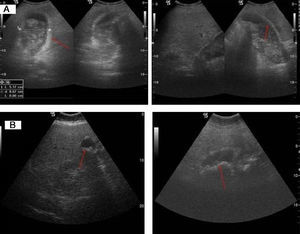
Regarding the ultrasound characteristics observed, the most prevalent pattern was focal or diffuse wall thickening (>4mm), present in 8 cases (Fig. 2). In one case the pattern was of a mass replacing the gallbladder (Fig. 3), and in another 4 cases there was an intraluminal mass, although in 3 there was also focal wall thickening (Fig. 4A). In 2 cases of gallbladder cancer none of these patterns were present; the ultrasound scans showed an atrophic and contracted gallbladder (Fig. 4B).
moderately differentiated carcinoma (T2). (A) Open gallbladder invaded by multiple faceted stones on a necrotic bed. Imaging of the gallbladder section in the background. A neoplasm infiltrating the muscular layer can be observed. (B) Diffuse and irregular gallbladder wall thickening with non-uniform echoes and acoustic shadow content.
(A) Poorly differentiated carcinoma (T2). Major wall thickening, with non-uniform echoes mass which shifts position when patient moves and produces acoustic shadow compatible with lithiasis and barium in the biliary tract or detritus. (B) Moderately differentiated carcinoma (T2). Atrophic and contracted gallbladder, with echogenic material on the inside and acoustic shadow compatible with lithiasis.
According to TNM classification T for gallbladder cancer, in our study 4 patients were recorded with a primary gallbladder carcinoma in situ (Tis) category, 3 of them presenting an intraluminal growth mass in the ultrasound imaging and one of them a diffuse wall thickening. One T1a case was recorded which presented with diffuse and irregular gallbladder wall thickening. Of the 6 T2 primary tumour cases, 4 showed diffuse wall thickening, one a focal thickening with an intraluminal tumour growth with polypoidal mass, and in another case the gallbladder was atrophic and contracted. Of the 3 cases with primary T3 tumour, one presented a mass pattern which replaced the gallbladder, another a diffuse wall thickening with a dependent mass, with growth towards the exterior of the organ, and the third case presented a scleroatrophic gallbladder with lithiasis inside it and dilatation of the intrahepatic biliary duct. The ultrasound and CT imaging of our only case of a T4 primary tumour showed a de-structured gallbladder with loss of morphology and execrescent wall mass towards the gallbladder exterior.
The cases of preoperative suspicion based on ultrasound findings were one Tis, 2 T3 and one T4.
It was confirmed that in 7 cases, the only pre-operative test was an ultrasound scan. CT abdominal scans with intravenous contrast were performed on 2 patients due to suspicion of gall bladder perforation. CT scans were also performed prior to surgery on 4 patients with pre-operative suspected cancer, in one case of cholelithiasis and a history of acute pancreatitis and in another case with choledocholithiasis.
A preoperative abdominal CT scan enabled staging to be completed. In the cases of suspected complicated cholecystitis the following were found: primary T1a (stage i) tumour and cancer in situ (stage i). In another case a CT scan was carried out previously, due to choledocholithiasis and a primary T3 (stage iii) tumour was found, and in the case of cholelithiasis with a history of pancreatitis a T2 (stage ii) tumour was found. In the cases of preoperative suspicion of gallbladder cancer, the CT staging scan found an in situ cancer (stage 0), 2 T3 (stage iii) and a T4 (stage iv).
When the pathologist reported on the Tis or T1a tumour in the surgical specimen following cholecystectomy, no treatment was added. Resection was extended to the gallbladder bed in the patients with incidental T2 cancer (3cm wedge resection of the area adjacent to the tumour with intraoperative histological study) with lymphadenectomy of the hepatic pedicle during the same operation or on reoperation.
Cholecystectomy and lymphadenectomy were performed on the patient with suspected Tis from preoperative ultrasound scan. One of the cases with suspected advanced T3 cancer presented dilatation of the biliary duct with jaundice. An exploratory laparotomy was performed which confirmed the unresectability of the neoplasm and the patient underwent a biliary bypass as a result.
DiscussionGallbladder cancer represents approximately 2%–4% of malignant tumours. It is the most frequent malignant neoplasm of the biliary system and the fifth of the digestive system. From an epidemiological viewpoint it appears to be predominant in females and usually affects adults in their sixties and seventies. Its incidence is higher in Latin American countries and is rarer in Northern Europe. Its incidence rate in Spain is intermediate.5,7–9
Both our study and the literature consulted1–5,7–9 showed that the principal associated risk factor is cholelithiasis (86%), which causes chronic irritation and inflammation of the gallbladder wall. This may lead to a dysplasia and subsequent appearance of cancer. Since this disease is highly prevalent, the presence of cholelithiasis alone does not help to establish early tumour diagnosis.5,7
The clinical expression is non-specific and often confused or associated with acute benign inflammation (acute cholecystitis),7–9 which occurred in 47% of the cases of our study. Moreover, of the 4 cases with preoperative suspicion of cancer, only 2 patients presented abdominal pain, and the other cases had no associated symptoms. Despite the fact that the majority of these neoplasms are asymptomatic in the early stages, several episodes of chronic cholecystitis, obstructive jaundice, external biliary fistula, and haemobilia have been recorded in literature.9
Regarding morphological features, tumours are highly variable in growth type and therefore, in their appearance on ultrasound imaging. The most commonly described presentation form is as a mass which replaces the gallbladder (40%–65%), visualized as a mass of heterogeneous echoes with irregular edges, with areas of necrosis or calcification on the inside.10 Echogenicity focal points and acoustic shadow associated with tumour may be related to the coexistence of lithiasis. Direct spread to the area around the liver and the biliary tree is common, and it may be impossible to establish an ultrasound limit between the mass and the liver parenchyma.11 Differential diagnosis should include metastases, cancer of the liver and cholangiocarcinoma.12,13 In this series, the only case with a mass pattern presented direct spread to the liver as a stage T3.
The second most frequent pattern is diffuse or focal wall thickening (20%–30%), which is the most difficult form of presentation to diagnose, since it is very non-specific and presents in many gallbladder diseases (acute cholecystitis and adenomiomatosis) and extravesicular diseases (hepatitis, cirrhosis, pancreatitis and heart failure).10 However there is some information which suggests malignancy and which should be recorded: wall thickening over 12mm which is irregular, marked wall asymmetry, loss of interface between the gallbladder wall and the liver, wall calcifications, adenopathies, and bile duct obstructions.10,11 In our study, this pattern presented in both early-stage and in T2 and T3 tumours.
A less common pattern is that of an intraluminal mass over 2cm, which presents in 15%–25% of cases as homogenous nodules or polyps which are well defined, without posterior shadow, and attached to the gallbladder wall. When they are smaller than 10mm they are indistinguishable from cholesterol polyps or adenomas and they usually represent early-stage neoplasms.9 In our study, 2 cases were in situ cancer and another 2 were stage T2, confirming that, as reflected in literature,10,11,14 this pattern is usually associated with neoplasms confined to the gallbladder wall.
The ultrasound imaging of the in situ gallbladder cancer and T1a, i.e., early stages, presented in our study as a pattern of wall thickening. This constitutes a diagnostic challenge, since the most common inflammatory pathologies of the gallbladder present a similar ultrasound pattern. Three cases of carcinoma in situ presented an intraluminal growth mass pattern; this pattern is usually associated with early stages and warrants a differential diagnosis with very common benign pathologies.
In our study, the most frequent pattern was gallbladder wall thickening (57%), whilst in literature it is one of a mass which replaces the gallbladder (65%). This could be due to our only recording a late stage diagnosis, which is associated more frequently with the latter pattern. In our opinion, the thickening pattern is replacing the mass pattern as the most frequent diagnostic imaging in gallbladder cancer because ultrasound is generally used as the first imaging test in patients with a non specific abdominal condition, which enables diagnosis of the disease in earlier stages. Several authors have proposed that signs of cholelithiasis and gallbladder wall thickening on ultrasound scan should be enough to indicate surgery, even in the absence of any other symptom.15
Diagnosis in early stages is difficult because the most common methods of imaging (ultrasound and CT scans) are insensitive and non-specific.3 In our experience diagnosis was only reached using ultrasound on 4 occasions and, when suspicion of neoplasm was confirmed, 3 of them were already too advanced. In advanced stages, ultrasound scanning may provide a greater than 80% diagnostic precision when both the gallbladder and the biliary ducts have been compromised, as well as providing very useful information regarding tumour size and the spread of the disease. In combination with the colour Doppler ultrasound, it can detect portal invasion in up to 83%–86% of cases. It is thus a very effective tool for identifying non resectable patients where the tumour has invaded these structures.5,9
Notwithstanding, when the preoperative images indicate a locally advanced stage, taking radiologically guided biopsies using fine needle puncture-aspiration assessment (PAAF) may prevent unnecessary laparotomy, as shown by De la Cruz et al.13 in a retrospective study. PAAF will only be indicated to confirm a histological diagnosis of gallbladder masses which are considered unresectable, in order to prevent the risk of an operable cancer spreading via the puncture route.9
In selected cases with suspected diagnosis from an ultrasound scan, different techniques can be used to improve the preoperative diagnosis and to plan the correct surgical strategy. CT scanning provides complementary information on tumour spread, and is the diagnostic tool of choice for disease staging and assessment of resectability when an ultrasound scan has shown suspected cancer. The magnetic resonance cholangiopancreatography test is the non-invasive imaging technique which provides the most information on biliary duct involvement.14,16 Positron emission tomography (PET)-fluorodeoxyglucose can also be used to establish whether the lesion is benign or malignant and for primary staging. If cancer is confirmed, spiral CT scanning can take diagnosis a stage further and establish local spread. Hybrid PET-CT systems provide structural and functional information at the same time, and may offer more specific early and correct classification, but they are not available in all hospitals.4
Other techniques, such as contrast-enhanced ultrasound, may also complete the study enabling wall thickening (through enhancement) to be differentiated from biliary sludge, and provide a clear view of the limit between the liver and the gallbladder wall.16 Endoscopic ultrasonography allows a diagnosis of gallbladder cancer to be established with a reliability rate of over 85% and particularly if combined with PAAF.14,17
ConclusionsDue to its non-specificity and comparability to other benign diseases, gallbladder cancer is diagnosed at an advanced stage. Ultrasound diagnosis is limited; only localized and irregular wall thickening, together with gallbladder lithiasis appears to be significant in the early stages, whilst the image of mass occupying the gallbladder is associated with more advanced stages of the disease.
Since ultrasound scan is the initial diagnostic procedure and the most effective in assessing gallbladder disease, it is important to consider the findings from this scan as a guide towards a probable neoplastic disease of vesicular origin.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Zevallos Maldonado C, Ruiz Lopez MJ, Gonzalez Valverde FM, Alarcon Soldevilla F, Pastor Quirante F, Garcia Medina V. Hallazgos ecográficos asociados al cáncer de vesícula biliar. Cir Esp. 2014;92:348–355.