Urachal cancer is one of the rarest and most aggressive neoplasms affecting the bladder. First described in 1863 by Hue and Jacquin, it represents less than 1% of bladder cancers and 0.01% of adult neoplasms, with an estimated annual incidence of one case per 5 million individuals1. The urachus is a tubular structure located in the midline that connects the umbilicus with the dome of the bladder2. It is an embryonic remnant of the cloaca and allantois that usually involutes from the third trimester of gestation to a fibrous structure that has no function, known as the median ligament. However, several autopsy studies describe the presence of urachal remnants in 32% of the adult population3,4. Its histological composition (internal-transitional epithelium, intermediate-connective tissue and external-muscular layer), metaplastic changes of the urothelium and the persistence of intestinal endodermal tissue help explain how an adenocarcinoma can present in an organ that has no glandular tissue2. Some 90% of cancers of the urachus are adenocarcinomas, which predominantly affect males (5:1) and usually present between the 5th and 6th decades of life3. In the Spanish literature, fewer than 40 cases have been published historically. Thus, we describe the diagnostic-therapeutic sequence followed in a patient with primary adenocarcinoma of the urachus, while also reviewing the existing scientific literature on this subject.
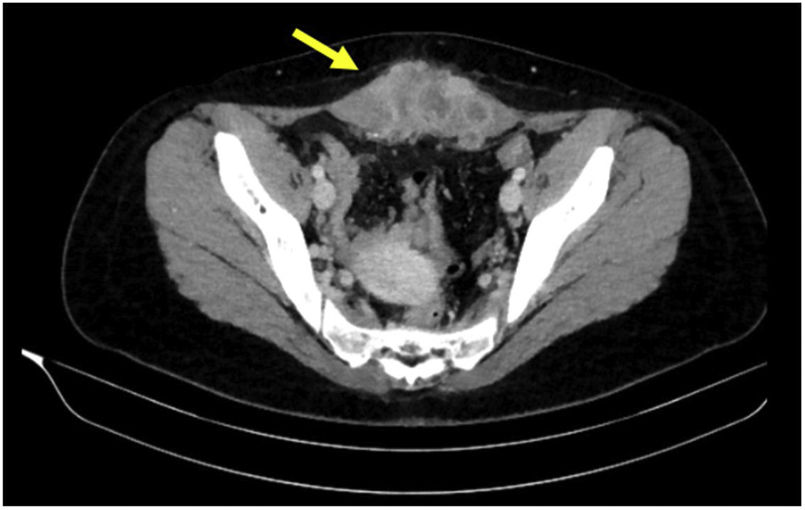
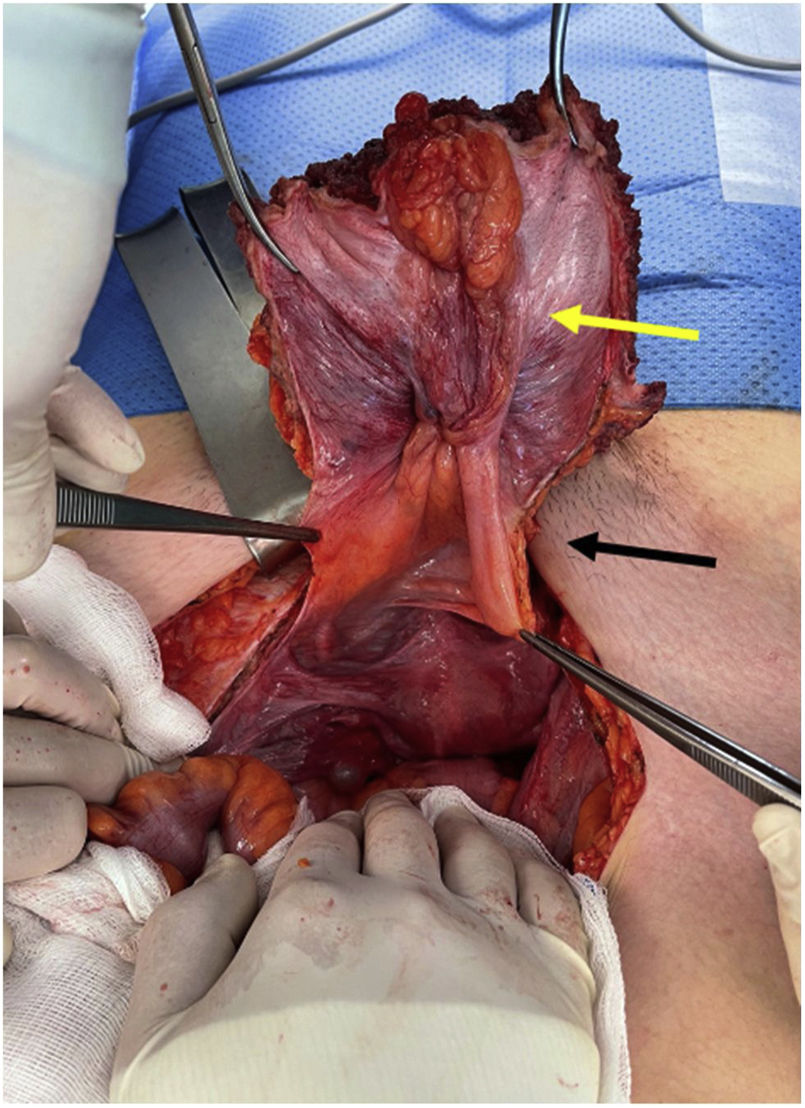
The patient is a 19-year-old woman with a history of right adnexectomy at the age of 15 due to a mucinous cystadenoma measuring 35 cm in diameter. She consulted for pain and a stone-like, immobile, hypogastric tumor located under the Pfannenstiel scar that had been progressing over the past 2 months. Abdominal-pelvic CT scan identified a solid infraumbilical lesion (8 × 8 × 4 cm) occupying both rectus muscles and showing signs of local invasion, suggestive of a desmoid tumor; likewise, a urachal remnant was observed connecting the umbilicus to the bladder (Fig. 1). The PET/CT scan ruled out distant involvement. An ultrasound-guided biopsy was performed, which provided a diagnosis of mucus-secreting adenocarcinoma with signet-ring cells, suggestive of urachal adenocarcinoma. The Multidisciplinary Team decided on the surgical resection, which included en bloc resection of the abdominal wall (anterior rectus muscles, umbilicus, median ligament, soft tissues, and parietal peritoneum) with a margin greater than 1.5 cm, but no excision of the dome of the bladder due to the absence of macroscopic invasion, followed by abdominal wall repair with partially absorbable macroporous bilayer mesh (Fig. 2). The anatomopathological study confirmed the diagnosis of adenocarcinoma of the urachus with a tubular pattern, undifferentiated areas and large necrotic areas (8.5 cm in diameter); free margins and 4/5 involved lymph nodes. Immunohistochemical profile (IHC): CK20q–, nuclear B-Catenin–, cytoplasmic B-Catenin+, CK34BetaE12+, GATA3–, CDX2+ (weak and very focal). All of this was compatible with Sheldon stage IIIB. Adjuvant chemotherapy was initiated with the FOLFOX regimen. Follow-up PET/CT scan 2 months later identified metastatic bone lesions in L5 as well as the right ischium and pubis. Currently, the patient continues with adjuvant therapy, and the distant lesions remain radiologically stable.
Axial abdominal-pelvic CT scan with intravenous contrast revealing a solid infraumbilical lesion (8 × 8 × 4 cm) occupying both rectus muscles with signs of local invasion, suggestive of a desmoid tumor (yellow arrow); likewise, urachal remnant connecting the umbilicus to the bladder is observed.
The most common form of presentation is hematuria, followed by a palpable suprapubic mass and mucus in urine. Other less frequent symptoms include bloody urethral discharge, recurrent urinary tract infections, and obstructive urinary symptoms5. However, these tumors usually remain asymptomatic for long periods of time, which allows them to locally invade other neighboring structures and metastasize to distant structures prior to their diagnosis2.
Suspicious images are often revealed by imaging studies, and the most widely used are ultrasound and computed tomography scans. Magnetic resonance imaging can delimit locoregional tumor invasion. Biopsy will make it possible to confirm the diagnosis either percutaneously in palpable parietal masses or through cystoscopy6.
The most widely accepted criteria for the anatomopathological diagnosis of urachal adenocarcinoma to differentiate it from other primary bladder adenocarcinomas are those proposed by Sheldon et al.7:
- •
Tumor located in the dome/anterior wall of the bladder
- •
Epicenter of the carcinoma in the bladder wall
- •
Absence of generalized cystic cystitis or glandular cystitis beyond the dome/anterior wall
- •
Absence of urothelial neoplasm in the bladder
- •
Absence of a known primary tumor elsewhere
The differential diagnosis should include: urachal cysts, desmoid tumors, primary bladder adenocarcinomas, contiguous invasion by colon adenocarcinomas, or tumors of the female genital tract1. For these, characteristic IHC markers can help identify the lesion, specifically β-catenin, CK7 and CK208.
In the absence of metastatic disease, the standard treatment is surgical: en bloc resection of the umbilicus + median ligament + soft tissue ± radical/partial cystectomy if previously demonstrated bladder involvement. Lymphadenectomy or the use of adjuvant therapies (chemotherapy or radiotherapy) are not systematically recommended, although favorable results have been reported in some cases; therefore, decisions must be individualized9,10.
In cases of disease located in the urachus, the prognosis is favorable; however, survival in distant disease does not usually exceed 12 months after diagnosis. Recurrence rates of 15% are described, especially during the 6 months after surgery2.
Carcinoma of the urachus is an aggressive, rare tumor with a silent behavior in early phases leading to late diagnosis, which is reflected in the unfortunate prognosis. The recommended treatment consists of surgical resection, while the debate about the benefits of radiotherapy and chemotherapy persists.
FundingThe authors have received no funding for this article.
Conflict of interestThe authors have no conflicts of interests to declare.