There are both biological and sociocultural differences in cardiovascular diseases. Inequalities in the prognosis between women and men are due to various variables, including specific risk factors for females, discrepancies in treatment strategies and pathophysiological differences.
ObjectiveIdentify sexual differences in patients with acute coronary syndrome.
MethodsAn observational, analytical, cross-sectional study was carried out on sex differences in 170 patients with a diagnosis of Acute Coronary Syndrome who were discharge from the Intensive Coronary Care Unit of the "Comandante Manuel Fajardo" Clinical-Surgical Hospital in 2016 and 2017.
ResultsFemales had statistically very significant association with a higher mean age (68 vs. 62 p < 0.01) and with a history of Arterial Hypertension (91.2% vs. 72.3% p < 0.01). The smoking habit showed a statistically significant association with male individuals (50.5% vs. 30.4% p = 0.017). The male sex had a significantly higher median creatinine (90 μmol/L vs. 80 μmol/L p < 0.01). Women showed an increased risk of hemodynamic complications (OR = 2.7,95% CI = 1.05–6.92).
ConclusionsIn women with Acute Coronary Syndrome, the female sex is associated with older age, a history of arterial hypertension and the appearance of intra-hospital hemodynamic complications. Males are associated with smoking habits and higher concentrations of serum creatinine.
Existen diferencias tanto biológicas como socioculturales en las afecciones cardiovasculares.Las desigualdades en el pronóstico entre mujeres y hombres se deben a diversas variables, entre las que se encuentran factores de riesgo específicos de las féminas, discrepancias en las estrategias de tratamiento y diferencias fisiopatológicas.
ObjetivoIdentificar diferencias sexuales en pacientes que presentan un síndrome coronario agudo.
MétodosSe realizó un estudio observacional, analítico, de corte transversal, sobre diferencias de sexo en 170 pacientes con diagnóstico de Síndrome Coronario Agudo egresados vivos de la Unidad de Cuidados Coronarios Intensivos del Hospital Clínico-Quirúrgico “Comandante Manuel Fajardo” en 2016 y 2017.
ResultadosLas féminas tuvieron asociación estadísticamente muy significativa con una media de edad mayor (68 vs 62 p < 0,01) y con el antecedente de Hipertensión Arterial (91,2 % vs 72,3 % p < 0,01). El hábito tabáquico mostró asociación estadísticamente significativa con los individuos varones (50,5 % vs 30,4 % p = 0,017). El sexo masculino tuvo una mediana de creatinina muy significativamente mayor (90 µmol/L vs 80 µmol/Lp < 0,01).Las mujeres mostraron un mayor riesgo de complicaciones hemodinámicas (OR = 2,7 IC 95 % = 1,05–6,92).
ConclusionesEn individuos con Síndrome Coronario Agudo el sexo femenino se asocia con mayor edad, antecedente de hipertensión arterial y aparición de complicaciones hemodinámicas intrahospitalarias. Los varones se asocian con el hábito tabáquico y mayores concentraciones de creatinina sérica.
Ischemic cardiopathy (IC) is the entity caused by an imbalance between myocardial offer and demand for oxygen. It includes acute coronary syndromes (ACS) when the symptoms establish or become acutely more severe.1
ACS in turn are classified according to the 12-lead electrocardiogram in acute coronary syndrome with elevated ST (ACSWEST), and acute coronary syndrome without elevated ST (ACSWOEST).1
The nosological entity par excellence within ACSWEST is ST elevation myocardial infarction (STEMI).2 Meanwhile, the clinical spectrum of ACSWOEST is broader, and it includes non-ST elevation myocardial infarction (NSTEMI) and unstable angina.3
The fourth universal definition of myocardial infarction defines it as an acute myocardial lesion (detected by means of cardiac biomarkers) in the course of an acute myocardial ischemia.4
There are biological (sexual) differences as well as sociocultural ones (gender-based) in cardiovascular complaints. Inequalities between the prognosis for women and men are due to a range of variables, including specific risk factors for women, discrepancies in treatment strategies and physiopathological differences.1
The characteristic biological differences of women which distinctively influence IC include endothelial oestrogen protection and loss of the same (in the menopause), a different distribution of fat, greater coronary microvascular dysfunction and fewer atherosclerotic plaques.5 Additionally, myocardial infarction without significant coronary lesions is statistically associated with the female sex.5,6
The European Society of Cardiology states that women have a higher risk of intrahospital death than men, because they receive treatments based on the most recent evidence less frequently.7
These previously described discrepancies led the authors to undertaken this study, which had the aim of identifying gender differences in patients with ACS.
MethodsA cross-sectional, observational analytic study was performed of the gender differences in patients diagnosed ACS who were discharged alive from the Cardiac Intensive Care Unit of the Hospital Clínico-Quirúrgico Comandante Manuel Fajardo from January 2016 to December 2017.
The universe was composed of 170 individuals admitted successively in the Cardiac Intensive Care Unit of the institution with a diagnosis of ACS, and who fulfilled the inclusion and exclusion criteria. They were divided into two groups for this study: individuals of the male sex (101) and those of the female sex (69). No sampling technique was used.
Inclusion criterion:
- •
Patients diagnosed ACS and discharged alive from the Cardiac Intensive Care Unit.
Exclusion criteria:
- •
Patients who lack all of the data evaluated in this study in the Cardiac Care Unit database. (58 patients were excluded because they had no record of blood creatinine levels, 11 because they had no record of cardiac biomarkers, and 101 because they had not been subjected to an echocardiogram during hospitalisation).
Of the total of 340 patients admitted due to ACS during the study period, a total of 170 were analysed after excluding those who did not fulfil the inclusion/exclusion criteria.
The data were extracted from a database belonging to the Intensive Cardiac Care Unit of the institution before entering them in the IBM SPSS Statistics 20 package for analysis. Qualitative variables were expressed as absolute and relative frequencies. The distribution of the quantitative variables was checked using the Shapiro-Wilk test, and the average and standard deviation (SD) were expressed when distribution was normal, and their median and interquartile range were expressed when it was not.
The X2 test or Fisher’s exact test were used to evaluate the association between categorical variables when fewer than 80% of the cells in the contingency table had expected values greater than 5. The Student t-test was used to compare the numerical variables for independent samples when they were distributed normally, or the Mann-Whitney U test was used when they were not. The odds ratio was used to evaluate the risk of complications, adjusted according to age (with the cut-off point at 45 years old for men and 55 years old for women) using a logistic regression model. P values < .05 were considered to be statistically significant, and where values of P < .01 were considered to be highly statistically significant. Confidence intervals of 95% were calculated.
The following variables were studied:
Clinical and sociodemographic variables: age; sex; personal pathological history: arterial hypertension, diabetes mellitus, obesity and BMI; smoking; form of presentation (ACSWEST or ACSWOEST); initial risk (according to the TIMI risk scores for ACSWEST8 and for ACSWOEST9) and intrahospital complications: hemodynamic problems (acute heart failure, cardiogenic shock, right ventricular failure and hyperdynamic states), electrical problems (supraventricular tachycardia, ventricular tachycardia, atrioventricular block, severe bradicardia with hemodynamic repercussion) and any complication (the latter refers to individuals who suffered at least one complication while hospitalised, regardless of what it was).
Analytical and imaging test variables: blood creatinine (measured in μmol/L), creatinine kinase MB isoenzyme (CK-MB) (measured in UI/L) and left ventricular ejection fraction (LVEF). The latter was classified according to the most recent cardiac insufficiency guidelines by the European Society of Cardiology.10
This research was approved by the Directorship of the Cardiac Department of the hospital after evaluating its compliance with the scientific research ethics. The data obtained were carefully guarded, complying at all times with the ethical principles for medical research established by the Helsinki Declaration, amended in the 52 General Assembly of Edinburgh in October 2002.
This research required no economic input or major material resources.
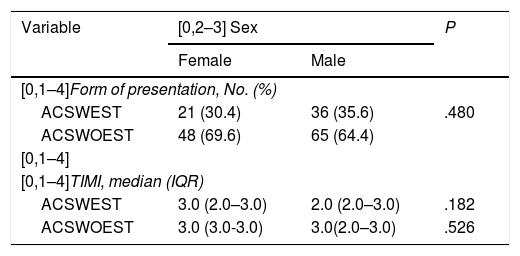
ResultsACSWOEST predominated in both sexes, without any significant statistical association with either of them. The TIMI risk scores were not associated with gender in either of the two forms of ACS (Table 1).
Association between forms of presentation, initial risk and sex.
| Variable | [0,2–3] Sex | P | |
|---|---|---|---|
| Female | Male | ||
| [0,1–4]Form of presentation, No. (%) | |||
| ACSWEST | 21 (30.4) | 36 (35.6) | .480 |
| ACSWOEST | 48 (69.6) | 65 (64.4) | |
| [0,1–4] | |||
| [0,1–4]TIMI, median (IQR) | |||
| ACSWEST | 3.0 (2.0–3.0) | 2.0 (2.0–3.0) | .182 |
| ACSWOEST | 3.0 (3.0-3.0) | 3.0(2.0–3.0) | .526 |
IQR: interquartile range.
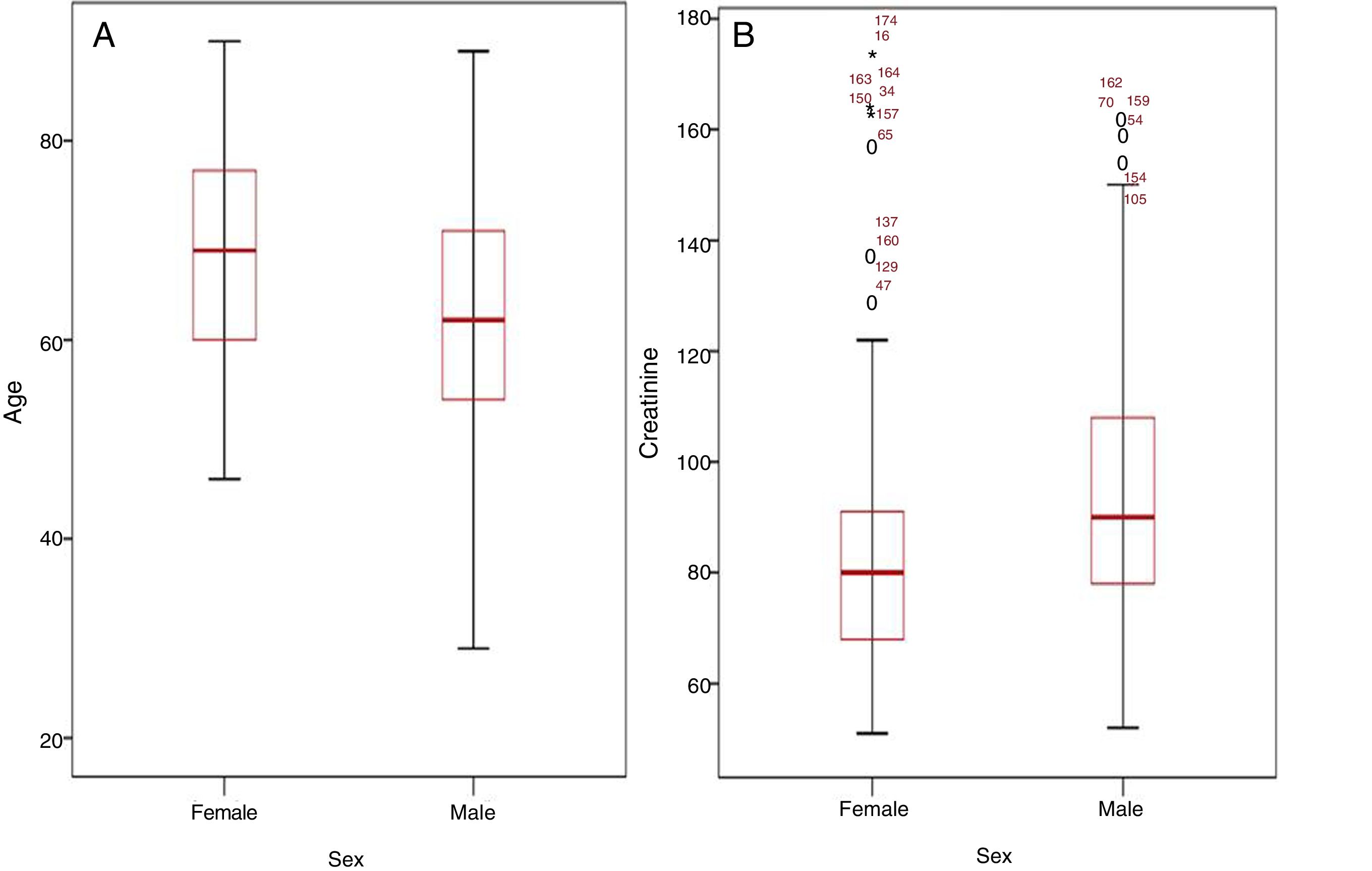
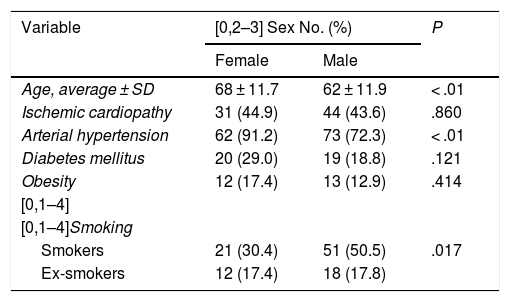
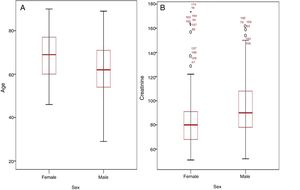
Table 2 shows the association between the personal pathological history of individuals and gender. The women had a highly significant association with a higher average age (P< .01) (Fig. 1A) and with a history of AHT (P< .01). Smoking was statistically significantly associated with the men (P = .017).
Association between clinical history and sex.
| Variable | [0,2–3] Sex No. (%) | P | |
|---|---|---|---|
| Female | Male | ||
| Age, average ± SD | 68 ± 11.7 | 62 ± 11.9 | < .01 |
| Ischemic cardiopathy | 31 (44.9) | 44 (43.6) | .860 |
| Arterial hypertension | 62 (91.2) | 73 (72.3) | < .01 |
| Diabetes mellitus | 20 (29.0) | 19 (18.8) | .121 |
| Obesity | 12 (17.4) | 13 (12.9) | .414 |
| [0,1–4] | |||
| [0,1–4]Smoking | |||
| Smokers | 21 (30.4) | 51 (50.5) | .017 |
| Ex-smokers | 12 (17.4) | 18 (17.8) | |
SD: standard deviation.
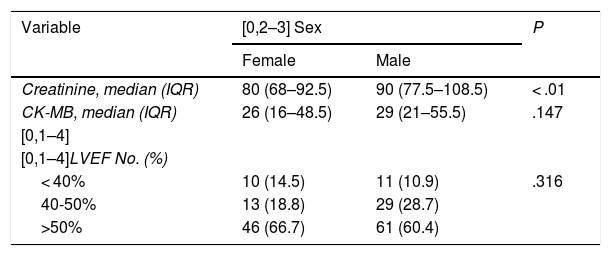
The men had a highly significantly higher median level of creatinine (P < .01) (Fig. 1B). There were no differences in terms of CK-MB values or LVEF (Table 3).
Association between blood analysis, LVEF and sex.
| Variable | [0,2–3] Sex | P | |
|---|---|---|---|
| Female | Male | ||
| Creatinine, median (IQR) | 80 (68–92.5) | 90 (77.5–108.5) | < .01 |
| CK-MB, median (IQR) | 26 (16–48.5) | 29 (21–55.5) | .147 |
| [0,1–4] | |||
| [0,1–4]LVEF No. (%) | |||
| < 40% | 10 (14.5) | 11 (10.9) | .316 |
| 40-50% | 13 (18.8) | 29 (28.7) | |
| >50% | 46 (66.7) | 61 (60.4) | |
CK-MB: creatinine-kinase MB isoenzyme; LVEF: left ventricular ejection fraction; IQR: interquartile range.
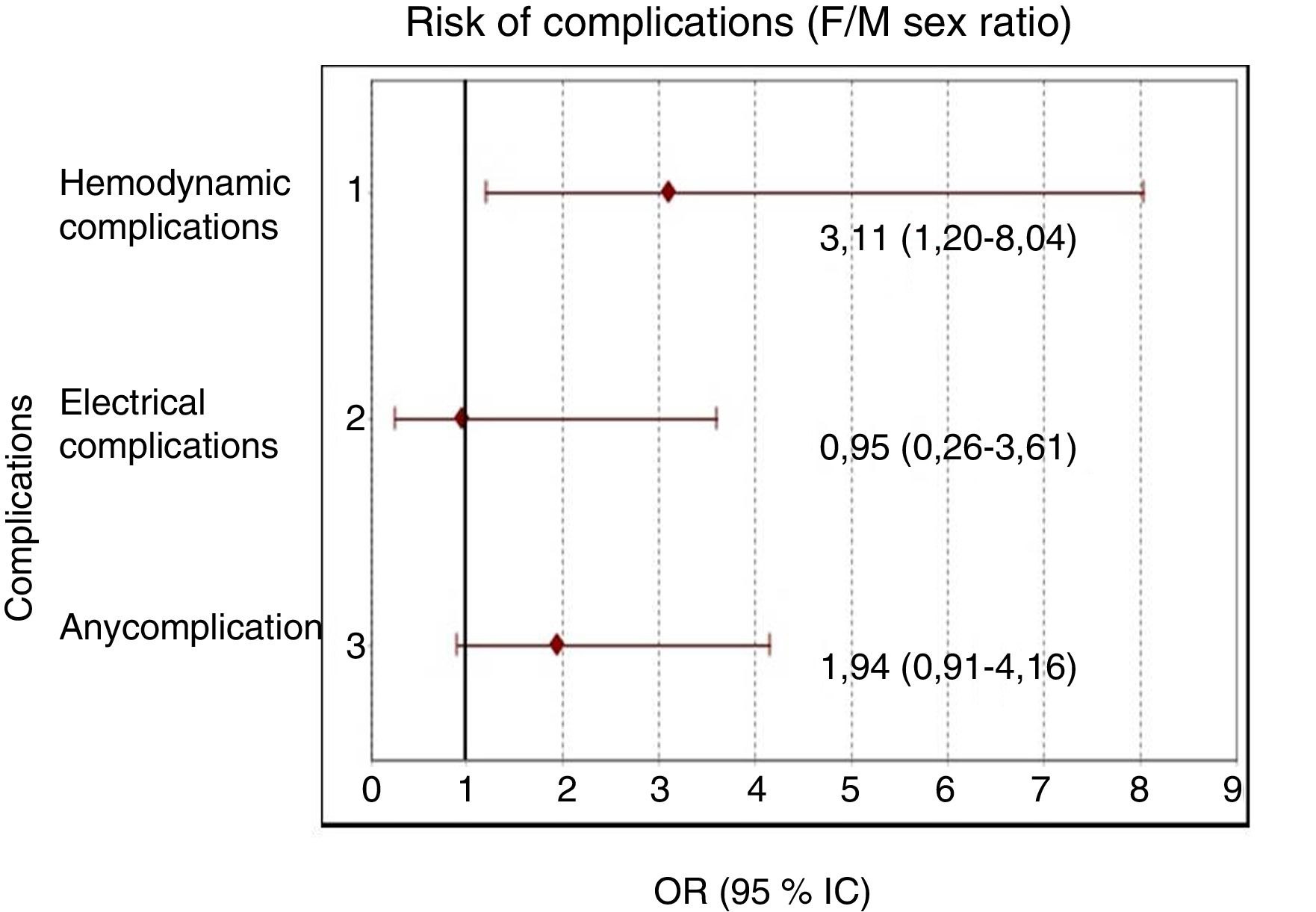
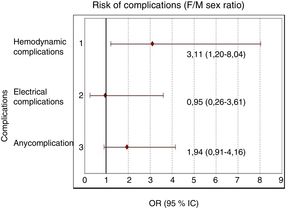
Fig. 2 shows the risk of intrahospital complications based on the female/male ratio. The women showed a statistically significant higher risk of hemodynamic complications when the cross products ratio was obtained (OR = 3.11 CI 95% = 1.20–8.04).
DiscussionThe main differences between the sexes in IC were found in pre-menopausal patients, given that the protection of oestrogen and its loss influences the course and prognosis of this entity.1
The above finding seems to explain why the women had a higher average age in the population that was studied, and this is similar to the findings of other studies.11–17
A systematic review that included 76,148 individuals in 11 clinical trials concluded that there is a clear association between a history of arterial hypertension and female sex in patients with ACSWOEST, and this finding was supported by our analysis.14 Other studies support this association.11,17–19
In a Turkish study of 3595 patients diagnosed ACS Kozan et al.11 found a significantly higher rate of smokers in the men (73.9% vs. 15.8%, P< .01). Robles-Mezcua et al.19 describe similar findings in a Spanish study of men under the age of 45 years old and women under the age of 55 years old (88.7% vs. 68.1%, P< .001), and in the men it was also associated with cocaine consumption. Other authors also describe this association.15,20
In agreement with the results of this study, Kozan et al.11 describe a higher concentration of blood creatinine in the men. Creatinine is a muscle metabolism product, and quantifying it is a practical method of calculating glomerular filtration and staging chronic kidney disease. It should be pointed out that this result is expectable, given that men have a greater muscle mass.21,22
Parra et al.23 find no association between a history of chronic kidney disease and male sex in ACS (18.9% vs. 4.1%, P = .004), as well as between male sex and higher levels of cardiac troponins. However, Sörensen et al.15 describe higher rates of glomerular filtration in men diagnosed ACS.
This study found no differences in terms of raised CK-MB (a cardiac biomarker) and sex. Nevertheless, although it would have been of interest to evaluate cardiac troponins instead of this, the hospital is not able to perform this complementary test.
This study found an association between women and the appearance of intrahospital hemodynamic complications. Pelletier et al.24, associated them with a higher rate of recurrence of ACS at 12 months, although they attribute this difference to social rather than biological factors. A multinational multicentre study concluded that women under the age of 55 years old hospitalised due to ACS had a lower quality of life over the long term than the men.25
A Columbian study found an association between female sex and mortality at 30 days in patients treated with a cardiac catheter (RP = 2.61, P = .017).26 Another study, undertaken in Germany with 185,132 individuals, concluded that women who received percutaneous cardiac surgery due to ACSWEST had a higher risk of intrahospital death and major cardiovascular and cerebrovascular events within the same time span as men.27 Other papers support these results.16,28
In contrast with the above findings, a paper by Sörensen et al.15 showed similar rates of repeat infarct and death between both sexes 2 years after suffering an ACS, although the men were readmitted more often for cardiovascular reasons and needed more revascularisations during this period. The RESCATE II study found higher mortality for men at 7 years after their first STEMI.17 Contradicting this, Robles-Mezcua et al.19 describe a higher survival rate over the long term in men with ACS than is the case in women.
The above considerations seem to indicate that women are at a higher risk of complications over the short term, although this tendency usually equals or even inverts in comparison with men over the long term.
The chief limitation of this study lies in that as it is cross-sectional this hinders the detection of causal relationship between statistically associated factors. Additionally, as the studied population is relatively small, this may influence the statistical analysis that was carried out. Nevertheless, this study may serve as the starting point for other larger scale studies that evaluate the times which pass until the appearance of the events in question.
ConclusionsThe women are significantly older and are associated with a history of arterial hypertension. Smoking predominates in the men, as does a significantly higher blood concentration of creatinine. Although the women have a higher risk of intrahospital hemodynamic complications, this is not the case for electrical complications.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Rojas-Velázquez J.M., Giralt-Herrera A., de la Torre Fonseca L.M., Machín-Legón M., Menéndez S.S.C. Diferencias sexuales en el síndrome coronario agudo. Hospital Comandante Manuel Fajardo, 2016-2017. Clin Investig Arterioscler. 2019. https://doi.org/10.1016/j.arteri.2019.08.001