Diabetes, especially type 2 (DM2), is considered a risk situation for atherosclerotic cardiovascular disease (ASCVD). Subjects with DM2 have a mortality rate due to ASCVD three times higher than that found in the general population, attributed to hyperglycemia and the frequent association of other cardiovascular risk factors, such as atherogenic dyslipidemia.
Numerous scientific societies have established a risk classification for ASCVD in diabetes based on 3 degrees (moderate, high and very high). The objectives of dyslipidemia control are clearly defined and accepted, and vary depending on the previously established cardiovascular risk.
In moderate or intermediate risk, the guidelines propose a less aggressive intervention, maintaining LDL-C levels <100mg/dL and NO-HDL-C levels <130mg/dL, and waiting 10 years until reaching the high-risk category to initiate more aggressive treatment. However, during the decade of follow-up recommended in the guidelines, cholesterol deposition in the arterial wall increases, facilitating the development of an unstable and inflammatory atheromatous plaque, and the development of ASCVD. Alternatively, diabetes could be considered from the outset to be a high-risk situation and the goal should be LDL-C <70mg/dL. Furthermore, maintaining LDL-C levels <70mg/dL contributes to reducing and stabilizing atheromatous plaque, avoiding or reducing mortality episodes due to ASCVD during those years of diabetes evolution.
Should we maintain the proposed objectives in subjects with diabetes and moderate risk for a decade until reaching the high cardiovascular risk phase or, on the contrary, should we adopt a more aggressive stance from the beginning seeking to reduce cardiovascular risk in the majority of patients with diabetes? Is it better to wait or prevent with effective therapeutic measures from the first moment?
La diabetes, especialmente el tipo 2 (DM2), está considerada como una situación de riesgo de enfermedad cardiovascular aterosclerosa (ECVA). Los sujetos con DM2 tienen una mortalidad por ECVA tres veces superior a la de la población general, atribuida a la hiperglucemia y a la frecuente asociación de otros factores de riesgo cardiovascular, como la dislipemia aterogénica.
Numerosas sociedades científicas han establecido una clasificación de riesgo de ECVA en la diabetes basada en 3 grados (moderado, alto y muy alto). Los objetivos del control de la dislipemia están claramente definidos y aceptados, y varían dependiendo del riesgo cardiovascular previamente establecido.
En el riesgo moderado o intermedio, las guías proponen una intervención menos agresiva, manteniendo cifras de C-LDL <100mg/dL y de C-NO-HDL <130mg/dL, y esperar 10 años hasta alcanzar la categoría de alto riesgo para iniciar un tratamiento más agresivo. Sin embargo, durante la década de seguimiento preconizada en las guías, el depósito de colesterol en la pared arterial va aumentando, facilitando el desarrollo de una placa de ateroma inestable e inflamatoria, y el desarrollo de ECVA. Alternativamente, se podría considerar desde el inicio que la diabetes conlleva una situación de alto riesgo y el objetivo debería ser C-LDL <70mg/dl. Además, mantener cifras de C-LDL <70mg/dL contribuye a reducir y estabilizar la placa de ateroma, evitando o disminuyendo episodios de mortalidad por ECVA durante esos años de evolución de la diabetes.
¿Deberíamos mantener los objetivos propuestos en los sujetos con diabetes y riesgo moderado durante una década hasta alcanzar la fase de alto riesgo cardiovascular o, por el contrario, adoptar desde el inicio una postura más agresiva buscando reducir el riesgo cardiovascular en la mayoría de los pacientes con diabetes? ¿Es mejor esperar o prevenir con medidas terapéuticas efectivas desde el primer momento?
Atherosclerotic cardiovascular disease (ASCVD) is the leading cause of death in the world1 and is a serious public health problem in Europe in light of its elevated morbimortality.2
Diabetes mellitus, and diabetes type 2 (DM2) in particular, is a common and ever-growing affliction that, in our country alone, affects 13.8% of the population.3 It is regarded as a situation that entails cardiovascular risk, especially for ASCVD. Even prediabetes, defined by HbA1c levels, exhibits a significant association with the risk of all-cause mortality, including ASCVD.4
Patients with DM2 have a three-fold ASCVD-related mortality rate and a two-fold total mortality rate of that found in the non-diabetic population of similar age and sex.5 A recent study with an 18-year follow-up period found that cardiovascular mortality among individuals who were previously diagnosed DM2 was three times higher in males and six times greater in females and was double in those having been recently diagnosed DM2 compared to the non-diabetic population of similar age and sex.6
This elevated prevalence of ASCVD among type 2 diabetics can be explained by the relationship with hyperglycaemia and disturbances in glycosylation, oxidation, and chronic inflammation and the frequent association with dyslipidaemia, especially atherogenic dyslipidaemia,7 which lends a special risk of ASCVD. It must be remembered that dyslipidaemia is not only a risk factor, but also a causal factor, given that lipoproteins having a diameter of less 70nm are those that penetrate the arterial wall, are deposited there, and form the atheromatous plaque, which leads to an important state of chronic inflammation.8 The common association of diabetes with other cardiovascular risk factors, such as arterial hypertension, kidney disease, obesity, and metabolic syndrome, also contributes to said risk.
Diabetic dyslipidaemia is characterised by a moderate increase in low density lipoprotein cholesterol (LDL-C), as well as increased lipoproteins rich in triglycerides, very low-density lipoproteins and their remnants, in addition to those rich in cholesterol, and that, as previously pointed out, they are capable of crossing the arterial wall and contribute to the deposit of cholesterol and to the development of the atheromatous plaque. A 1mmol/L (39mg/dL) increase in the remnant cholesterol causes a significant increase in cardiovascular episodes, having a magnitude similar to that caused by increased LDL-C.9
Lipid cardiovascular risk in general, and in diabetes in particular when triglycerides are elevated, is related to the collection of atherogenic lipoproteins that we can quantify clinically with plasma apoB levels, or non-HDL cholesterol (c-non-HDL), calculated as the difference between total cholesterol and high-density lipoprotein cholesterol (c-HDL), which encompasses cholesterol from all circulating apoB or atherogenic lipoproteins.7,10
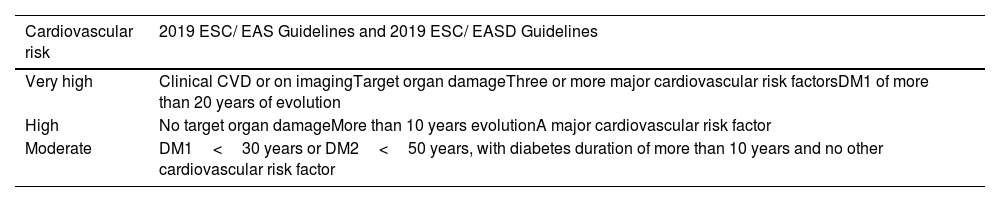
Classification of ASCVD risk in diabetesDM2 is recognised as a situation of heightened cardiovascular risk.11 In an endeavour to stage intervention guidelines, both the European Society of Cardiology/European Society of Arteriosclerosis12 and the European Society of Cardiology/European Association for the Study of Diabetes13 guidelines, issued in 2019, set the same parameters for calculating cardiovascular risk in diabetes (Table 1). The presence of chronic kidney disease per se, with an estimated glomerular filtration rate <30mL/min/1.73m2 and between 30–59mL/min/1.73m2 are classified as very high risk and high cardiovascular risk, respectively, especially if albuminuria is present.14
Cardiovascular risk in diabetes mellitus.
| Cardiovascular risk | 2019 ESC/ EAS Guidelines and 2019 ESC/ EASD Guidelines |
|---|---|
| Very high | Clinical CVD or on imagingTarget organ damageThree or more major cardiovascular risk factorsDM1 of more than 20 years of evolution |
| High | No target organ damageMore than 10 years evolutionA major cardiovascular risk factor |
| Moderate | DM1<30 years or DM2<50 years, with diabetes duration of more than 10 years and no other cardiovascular risk factor |
CVD: cardiovascular disease; DM1: Diabetes mellitus type 1; DM2: Diabetes mellitus type 2; EAS: European Atherosclerosis Society; EASD: European Association for the Study of Diabetes; ESC: European School of Cardiology.
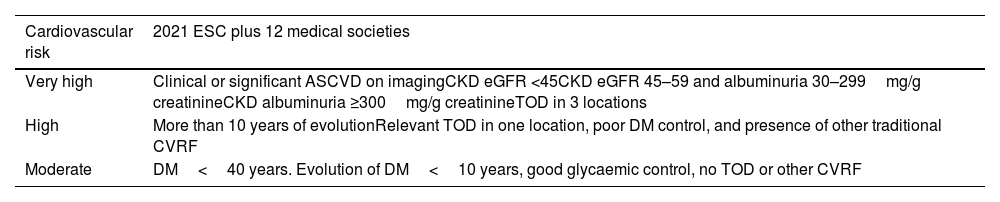
In the European Society of Cardiology guidelines, with the collaboration of 12 other societies, including the European Association for the Study of Diabetes, the European Society of Arteriosclerosis, and the International Diabetes Federation Europe, a new foundation for cardiovascular risk stratification has been established15 (Table 2), in addition to defining the categories of moderate, high, and very high risk.
Cardiovascular risk in diabetes mellitus (2021).
| Cardiovascular risk | 2021 ESC plus 12 medical societies |
|---|---|
| Very high | Clinical or significant ASCVD on imagingCKD eGFR <45CKD eGFR 45–59 and albuminuria 30–299mg/g creatinineCKD albuminuria ≥300mg/g creatinineTOD in 3 locations |
| High | More than 10 years of evolutionRelevant TOD in one location, poor DM control, and presence of other traditional CVRF |
| Moderate | DM<40 years. Evolution of DM<10 years, good glycaemic control, no TOD or other CVRF |
ASCVD: Atherosclerotic cardiovascular disease; CKD: Chronic kidney disease; CVRF: cardiovascular risk factors; DM: Diabetes mellitus; ESC: European Society of Cardiology; eGFR: estimated glomerular filtration rate (mL/ min/ 1.73m2); TOD: target organ damage.
Multifactorial therapy, including lifestyle changes, quitting smoking, administration of hypoglycaemic and antihypertensive drugs, is key to lowering the risk of ASCVD and all-cause mortality.16
Control of hyperglycaemiaIn order to control hyperglycaemia, the recommendation is to maintain HbA1c <7% in most people with diabetes, being less strict in older, frail subjects or those with uncontrolled cardiovascular disease; in these cases, maintaining HbA1c between 7 and 8% is deemed adequate. An HbA1c value of <6.5% may be an appropriate target in young individuals who have had diabetes for a short period of time and do not have ischaemic vascular disease.
Drug treatment must be personalised and based on the type of diabetes, the course of the disease, and existing complications. In subjects with ASCVD or at high or very high cardiovascular risk, it is recommended that treatment be initiated with metformin, if there is no contraindication; the next step is the administration of GLP1 receptor agonist drugs or SGLT2 inhibitors, and if the control target is not achieved with one of these drugs, both can be combined.17
Control of high blood pressureOnce the diagnosis of arterial hypertension has been established - systolic blood pressure≥140 and/or diastolic blood pressure≥90mmHg - the goals of treatment are: systolic blood pressure 120–130mmHg in people with diabetes aged 18–64 years and between 130–140mmHg in those over the age of 65 years and diastolic blood pressure<80mmHg in all groups, with recommended values of between 70–80mmHg, while keeping it from falling to <60mmHg.18
Treatment should be laid out in three steps: 1) angiotensin-converting enzyme inhibitor or angiotensin II receptor antagonist plus a calcium antagonist or diuretic (in patients with systolic blood pressure<150mmHg, over 80 years of age, or frail, it can be started as monotherapy); 2) angiotensin-converting enzyme or angiotensin II receptor antagonist, calcium antagonist, and diuretic, and, 3) if the values remain elevated after the previous treatment (refractory hypertension), secondary causes should be ruled out and a fourth drug, low-dose spiro-lactone 25–50mg/day, alpha blockers, or beta blockers, should be added.19
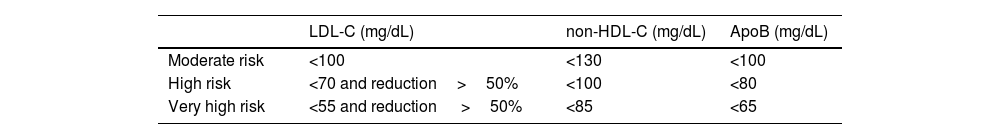
Control of hyperlipidaemiaUnlike what happens with other cardiovascular risk factors, targets for the control of hyperlipidaemia vary depending on the calculated degree of cardiovascular risk.
Goals for hyperlipidaemia are set by serum LDL-C, non-HDL-C, or by plasma apoB values, because the risk remains elevated in cases with adequate LDL-C control, but with elevated non-HDL-C.20 The targets are set out in Table 3.15
Lipid targets according to cardiovascular risk.
| LDL-C (mg/dL) | non-HDL-C (mg/dL) | ApoB (mg/dL) | |
|---|---|---|---|
| Moderate risk | <100 | <130 | <100 |
| High risk | <70 and reduction>50% | <100 | <80 |
| Very high risk | <55 and reduction >50% | <85 | <65 |
ApoB: Apolipoprotein B; LDL-C: Low-density lipoprotein cholesterol; non-HDL-C: Total cholesterol minus high-density lipoproteins.
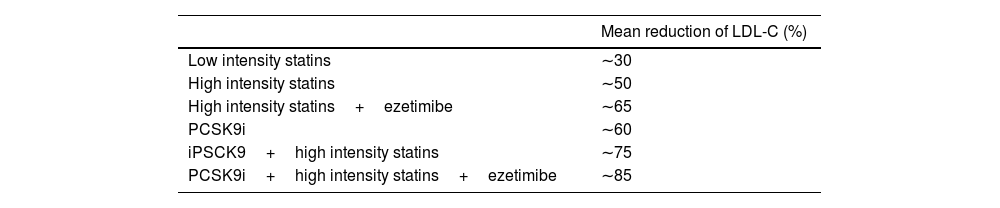
In all cases, pharmacological treatment will be titrated to achieve the required potency to achieve the intended target, based on the percentage of LDL-C reduction needed. The average potency of the various lipid-lowering drugs and their associations are listed in Table 4.
Approximate mean reduction in the percentage of LDL-C with the drugs most widely used in clinical practice.
| Mean reduction of LDL-C (%) | |
|---|---|
| Low intensity statins | ∼30 |
| High intensity statins | ∼50 |
| High intensity statins+ezetimibe | ∼65 |
| PCSK9i | ∼60 |
| iPSCK9+high intensity statins | ∼75 |
| PCSK9i+high intensity statins+ezetimibe | ∼85 |
LDL-C: Low density lipoprotein cholesterol; PCSK9i: Proprotein convertase subtilisin/kexin type 9.
After treatment with statins or combinations (Table 3) and after LDL-C and non-HDL-C targets have been met, fibrate administration (mainly fenofibrate) is recommended in those with triglyceride values>200mg/dL.7,21 In those at high or very high cardiovascular risk, the addition of eicosapentaenoic acid at a dose of 4g/day may reduce the number of AVCD episodes.22
We know that a decrease of 39mg/dL in LDL-C or c-non-HDL is associated with a 21% reduction in major cardiovascular events in treated subjects over a mean period of six years. This drop in cardiovascular events is greater with increasing years of treatment and also depends on the magnitude of the decrease; a reduction of 77mg/dL is associated with a 40% reduction in vascular events.23,24 In addition, the lower values, the lower the risk of AVCD,25 and lower figures may even stabilize and even decrease the volume of the atheromatous plaque.26 A meta-analysis has found that a 1% decrease in the volume of the atheromatous plaque produced by the drug treatment for dyslipidaemia was associated with a 20% reduction in the likelihood of major AVCD events.27
Action guidelines according to ASCVD riskIn high- and very high-risk situations, intensive lipid-lowering treatment with one or more drugs should be undertaken in order to attain the target values, a reduction of LDL-C to below the above-mentioned figures (<70 and <55mg/dL, respectively), in addition, a minimum reduction of 50% relative to baseline figures, as well as to reach the non-HDL-C or apoB targets.
Personal comments on intermediate risk in DM2With respect to the situation of moderate or intermediate risk, the guidelines establish very specific indications on how to act. In this regard, we would like to set forth the following considerations:
- 1
Patients at moderate risk must be assessed very carefully, inasmuch as this risk can be modified or reclassified as high risk depending on the presence of other compounding factors (Table 5). In addition to the usual cardiological examinations (ECG), it is of special interest that a vascular study be performed in the area of lipid metabolism and glycaemic control, with an echo-Doppler examination of the supra-aortic trunks to determine the existence of atheromatous plaques. Likewise, measurement of the ankle/brachial index or ankle/brachial systolic pressure ratio for each lower limb makes it possible to diagnose silent peripheral vascular disease. A value of less than 0.9 indicates a stenosis greater than 50% between the aorta and distal leg arteries with high specificity (90%) and a sensitivity rate of 79%.28
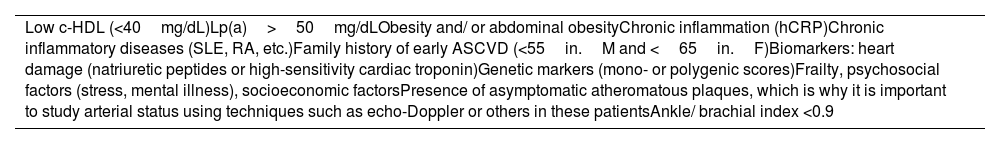
Table 5.Aggravating factors for ASCVD risk, especially during the moderate risk stage.
Low c-HDL (<40mg/dL)Lp(a)>50mg/dLObesity and/ or abdominal obesityChronic inflammation (hCRP)Chronic inflammatory diseases (SLE, RA, etc.)Family history of early ASCVD (<55in.M and <65in.F)Biomarkers: heart damage (natriuretic peptides or high-sensitivity cardiac troponin)Genetic markers (mono- or polygenic scores)Frailty, psychosocial factors (stress, mental illness), socioeconomic factorsPresence of asymptomatic atheromatous plaques, which is why it is important to study arterial status using techniques such as echo-Doppler or others in these patientsAnkle/ brachial index <0.9 ASCVD: Atherosclerotic cardiovascular disease; F: Females; hCRP: High-sensitivity C reactive protein; HDL-C: High density lipoprotein cholesterol; Lp(a): Lipoprotein (a); M: Males; RA: Rheumatoid arthritis SLE: Systemic lupus erythematosus.
- 2
Regardless of this possible reclassification based on the presence of the aforementioned aggravating factors, a number of situations should be taken into account in type 2 diabetics at moderate risk:
- -
The presence of the clinical manifestations of ASCVD is associated with a critical point of cholesterol deposit on the arterial wall, with the presence of an unstable, inflammatory plaque. This tipping point correlates with the plasma levels of cholesterol-rich lipoproteins (LDL and remnants) and with the time of exposure to these elevated lipoprotein values.29
- -
From the age of 10 years onwards, diabetics are considered to be at high risk (according to all consensus and guidelines) and therapeutic targets will be stricter. However, during this period, better lipid control would reduce the burden of cholesterol and inflammatory factors in the arterial wall and, as a result, improve the course toward possible cardiovascular events and cardiovascular death, which are so prevalent in individuals with DM2.
- -
The target in situations of moderate risk is to achieve levels of LDL-C<100mg/dL and c-non-HDL<130mg/dL, but cardiovascular risk is not the same if LDL-C near 70 or near 100mg/dL or its equivalent in c-non-HDL figures are maintained for 10 years, even if both are within the target range.
- -
Sustaining LDL-C<70mg/dL levels is linked to a reduction in atheromatous plaque volume and its stabilisation.26
- -
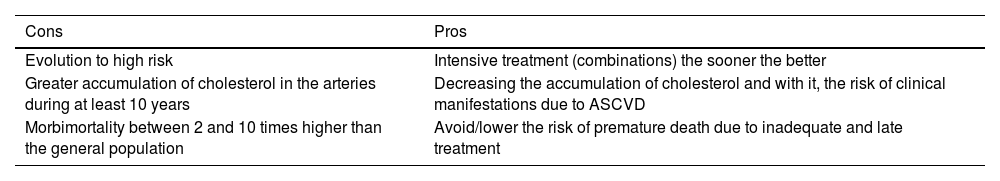
In the moderate risk subgroup, each case must be assessed on a case-by-case basis with the aforementioned studies to decide whether treatment goals should be stricter and we should act quickly,28 or whether, on the other hand, we should act given the high risk that the patient has or will have in 10 years’ time. The pros and cons of this scenario are laid out in Table 6.
The dilemma of lipid-lowering treatments in diabetes with a moderate level of risk.
| Cons | Pros |
|---|---|
| Evolution to high risk | Intensive treatment (combinations) the sooner the better |
| Greater accumulation of cholesterol in the arteries during at least 10 years | Decreasing the accumulation of cholesterol and with it, the risk of clinical manifestations due to ASCVD |
| Morbimortality between 2 and 10 times higher than the general population | Avoid/lower the risk of premature death due to inadequate and late treatment |
ASCVD: atheromatous cardiovascular disease.
Consequently, is it advisable to wait for a situation of moderate risk to evolve to the high-risk stage over the next decade, or should we act as if this were already the case and avoid or reduce atheromatous deposits and future complications in a disease in which the biggest problem will be cardiovascular events and cardiovascular mortality? Is it better to wait or to prevent with effective therapeutic measures?
Is it reasonable to allow it to evolve toward high-risk situations or is it more appropriate to intervene intensively to slow the progression of atheromatous plaque and prevent or mitigate the onset of cardiovascular events?
We believe that in DM2, the lowest LDL-C and c-non-HDL criteria possible should be maintained at all times, and the earlier we reach them, the easier it is to achieve a longer life expectancy.
ConclusionsDM2 is recognised as a situation of high or very high cardiovascular risk, especially in long-term diabetics with poor glycaemic control or those with comorbidities. Individuals considered to be at moderate cardiovascular risk should undergo thorough evaluation for possible reclassification to high or very high risk if other parameters or cardiovascular status warrant it. Intensive treatment should then be initiated to prevent and lower the significant risk of cardiovascular events and mortality associated with diabetes. Cardiovascular complications can occur even in the pre-diabetes period, as studies of newly diagnosed diabetics have proven. Current evidence reveals that maintaining LDL-C levels below 70mg/dL not only improves cardiovascular risk, but is associated with a reduction in atheromatous plaque volume and its stabilisation.26
FundingCIBER - Consorcio Centro de Investigación Biomédica en Red (Consortium of Biomedical Research Network) [CB07/ 08/ 0018], Instituto de Salud Carlos III (Carlos III Institute of Health), Ministerio de Ciencia e Innovación (Ministry of Science and Innovation), and the European Union (European Regional Development Fund).
Conflict of interestsThe authors have no conflict of interests to declare.