To assess the effect of a motivated physical activity program on the lipid parameters most related to excess weight (triglycerides [TG], and high density lipoprotein cholesterol [HDL]) in a weight-loss intervention in obese and overweight patients.
MethodsA randomised and controlled, 2-arm, clinical trial and a 12-months follow-up was conducted. The patients included in the study were randomised into 2 intervention groups: motivational intervention of obesity with a previously trained nurse (G1), motivational group, with digital platform support and motivated physical activity program (iwopi [G2]).
The anthropometric variables measured were height, weight, body mass index (BMI), as well as the analytical variables, total cholesterol, TG and HDL-C.
ResultsA total of 123 patients participated in the study, of which 61 were randomised to G1, and 62 to G2. Both groups significantly decreased weight at the end of the study, with the decrease in G1 being 4.898kg, and 6.292kg in G2. In both groups there was also a significantly decrease (p<0.05) in total cholesterol and TG, and increase in HDL cholesterol, with these changes being more intense in the G2 group, as well as being the group that lost more weight.
ConclusionsWeight reduction is accompanied by favourable changes in lipid parameters related to overweight and obesity, being more intense the greater the weight loss.
Valorar el efecto de un programa de actividad física motivada sobre los parámetros lipídicos más relacionados con el exceso de peso (triglicéridos [TG] y colesterol de las lipoproteínas de alta densidad [cHDL]) en una intervención para reducir peso en pacientes con sobrepeso y obesidad.
MétodosEnsayo clínico, aleatorizado y controlado, con 2 brazos y un seguimiento de 12 meses.
Los pacientes incluidos en el estudio fueron aleatorizados en 2 grupos de intervención: intervención motivacional de obesidad con enfermera entrenada previamente (G1), grupo motivacional, con apoyo de plataforma digital y programa de actividad física motivada (iwopi [G2]).
Las variables antropométricas medidas fueron estatura, peso, índice masa corporal (IMC) y las analíticas, colesterol total, TG y cHDL.
ResultadosHan participado en el estudio 123 pacientes, de los que 61 fueron aleatorizados al G1 y 62 al G2. Todos los grupos disminuyeron significativamente el peso al final del estudio, siendo la disminución en el G1 (−4,898kg) y del G2 (−6,292kg). También todos los grupos disminuyeron significativamente (p<0,05) el colesterol total y los TG, y aumentaron el cHDL, siendo estos cambios más intensos en el grupo G2, el grupo que más peso perdió.
ConclusionesLa reducción de peso se acompaña de cambios favorables en los parámetros lipídicos relacionados con el sobrepeso y la obesidad, siendo más intensos cuanto mayor es la pérdida de peso.
The World Health Organization (WHO) has been forced to declare that obesity is one of the great epidemics that will threaten us during the twenty-first century, which has led the governments of different countries and supranational institutions to grant increasingly greater importance to policies that can contribute to mitigate its effects. As with most of the diseases that have their main origin in environmental and social exposures, it is preventive measures, rather than therapeutic ones, that yield the most effective and efficient results, and in this sense most of the actions.1
Obesity is a major global public health problem and one of the most frequent metabolic alterations associated with this condition is the dyslipidemia that often accompanies it: its characteristic phenotypic pattern is preprandial hypertriglyceridemia, lowering of high density lipoprotein cholesterol (HDL-C), postprandial non-HDL hyperlipidemia and the real increase in the production of dense and small particles of low density lipoproteins. Comprehensive treatment (tmnt) of dyslipidemia in obese patients should always include an intense approach to addressing obesity and the identification and management of risk factors that interact with the condition, as well as a pharmacological risk-benefit assessment.1–3
In our environment, obesity and dyslipidemia are frequently linked; therefore, it is very likely that there will be a dyslipidemia phenotype when the body mass index is between 25.2 and 26.6kg/m2, as corroborated by numerous studies, among which is the United States National Health and Nutrition Examination Survey (NHANES).4–6. The separate reports on dyslipidemia in men and women and in different ethnic groups reflect a common dyslipidemia pattern: the significant increase in the real quantity of triglycerides (TG) (mainly very low density lipoproteins, total cholesterol [TC] and low HDL-C).
The NHANES data has shown that the levels of TC are greater in young obese men and women than in non-obese people. The NHANES III study has also demonstrated that in patients with metabolic syndrome the rates of obesity, hypertriglyceridaemia and hypercholesterolaemia are greater than 75%.4–9
It is well-known that treatment for dyslipidemia, both in overweight and obese patients, must start with weight loss.9,10 Accordingly, the interventions that are focused on changing dietary habits and increasing daily physical activity for the purposes of promoting a healthy lifestyle are the best options for tackling this problem; not forgetting that other interventions such as cognitive-behavioral therapy have proven useful when included in overweight and obesity program for the purpose of improving their effectiveness and helping maintain the results obtained.10
In 2004, the World Health Assembly approved the Global Strategy on Diet, Physical Activity and Health, with the aim of reducing the risk factors for non-communicable diseases related to unhealthy diets and physical inactivity.8 It urges all international, national and local organizations and institutions to develop actions that allow the creation of environments that promote an improvement in diet and reduce sedentary lifestyle.11
The level of physical condition, as well as the cardiovascular risk related to overweight and obesity in adults, is largely conditioned by the level of physical condition in childhood and adolescence.11,12 The benefits of low- to moderate-intensity physical activity form the basis of the physically-active lifestyle, which should be incorporated for a minimum of 30min daily, whether in leisure and free time, work, household chores, etc. planned or unplanned, and that they are part of everyday life, replacing hours of TV, computers and sedentary games with others of greater energy expenditure. Among the benefits provided, there is a decrease in mortality from all causes, regardless of their effects on weight. The 2016 WHO study (1) warned that more than 1.4 billion adults, just over a quarter of the world's adult population (27.5%), did not exercise enough. That year, about one in 3 women (32%) and one in 4 men (23%) worldwide did not reach the recommended levels of physical activity to stay healthy.
The multiple benefits of weight loss have been evidenced and it is undeniable that physical exercise helps to obtain greater energy expenditure. There are numerous authors who assert that the best option in weight loss for obese subjects is by combining a proper diet with a regular and structured practice of physical activity.9,10 The National Heart, Lung and Blood Institute (1998) advocates the combination of exercise and diet, given its evidence as the best allies of weight loss, with physical activity being the best mechanism.13–15
Our group designed a motivational group intervention for obese patients, conducted by a nurse who had previously been trained by psychological experts, combined with their routine treatment and with a 2-year follow-up period. The results were then published, with 36% of patients achieving weight loss ≥5%.16–18 This intervention was subsequently replicated in another region of Spain with the same results. As previously published, an hour-long motivational group intervention every two weeks from weeks 1 to 12, following the Lifestyle, Exercise, Attitudes, Relationships, Nutrition (LEARN)19–21 program guidelines, and then monthly from weeks 13 to 32, following the instructions of the Weight Maintenance Survival Guide program was added to routine treatment.22 Although the results were highly satisfactory, we now consider whether adding a motivated program of physical activity would add better results on the reduction of lipid parameters.
For this project, the following working hypothesis is proposed: by adding a digital platform intervention to the motivational group intervention, physical activity and weight results improve.
MethodRandomized and controlled clinical trial, with 2 arms, 12 months of follow-up and a 1:1 allocation ratio.
The data collection was made between July 2017 and July 2018. Patients, women and men, should have been referred from their company doctors with the diagnosis of overweight or obesity and an age between 25 and 70 years. They came from the health areas of Anoia and Barcelona. The exclusion criteria that were considered were: (1) severe diseases (bedridden, affected by neoplasms, cognitive disorders, etc.); (2) secondary obesity (hypothyroidism, Cushing's disease, etc.); (3) severe sensory diseases that interfere with motivational intervention, such as uncorrected visual or auditory impairments, etc.; (4) severe psychiatric diseases; (5) diagnosis of type 1 or type 2 diabetes mellitus with pharmacological tmnt; (6) diagnosis of arterial hypertension with pharmacological tmnt, and (7) diagnosis of dyslipidemia with pharmacological tmnt.
The patients who were included in the study signed an informed consent form approved by the regional Ethics Committee.
Interventions: patients were randomized into 2 intervention groups:
- -
Group 1 (G1): motivated obesity intervention (IMOAP), with trained nurse and small periodic work groups.
- -
Group 2 (G2): the use of a digital platform that monitors and promoted physical activity (iwopi) was added to the intervention of G1. This platform allows for registering physical activity and donating it for any of the social causes that exist on the platform. In fact, iwopi is a digital health platform with a methodology based on the science of behavior and behavioral activation, whose objective is to generate the necessary motivation in people to boost physical activity and, subsequently, healthy lifestyle habits. The ability to motivate and activate users is realized through elements of social gamification based on the improvement of physical, mental and social well-being. Among these elements of social gamification, iwopi promotes programs and emotional, collective and collaborative challenges, to stimulate physical activity and social relations with a solidary purpose. The user can monitor his or her physical activity through specific physical activity Apps, Devices (wearables, smartwatches, GPS watches), or through a Smartphone and systems such as Apple Health or Google Fit, and convert his or her movement into a real social impact. The technical characteristics are: development languages: HTML5, CSS3, Javascript; programming languages (Backend): Scala; databases: MySQL; servers: ApacheTecnología; desktop application: Play framework-Boostrap; mobile app development technology: Ionic; security certificate: Comodo SSL Premium Wildcard. Its structure as a single-page application allows a fluid interaction and the responsive design allows it to adapt to any modern browser (desktop, tablet or mobile) without changing the design nor the functionalities. This helps the user to interact on any of their devices and simplifies the learning curve, since the interaction is similar. The application is available on Google Play and Apple Store (www.iwopi.org).
In order to avoid possible influences of diet in the participating nurses, they were trained not to modify them as it was a criterion of withdrawal from the study.
Losses suffered during the study: one was lost in G1 because of a change in employment status and in G2 one left for family reasons.
Statistical analysisAll calculations were performed with the software program SPSS version 25.0 (v.25.0 of SPSS Inc., Chicago, IL, USA). Quantitative variables are shown as mean (standard deviation), qualitative variables as exact quantity and percentage. The ANOVA test was used to verify that the randomisation was performed correctly between the 3 groups compared. If there had been any significant differences between the groups, the Bonferroni method would be applied a posteriori. To compare the averages throughout the follow-up period, a repeated measures analysis of variance was used. When the normality and sphericity criteria were not met, the non-parametric Friedman test was used. When there were 2 groups to be compared, the differences between the means were calculated with the Student's t, for both independent and paired groups. Comparisons with a p value ≤0.05 were considered statistically significant.
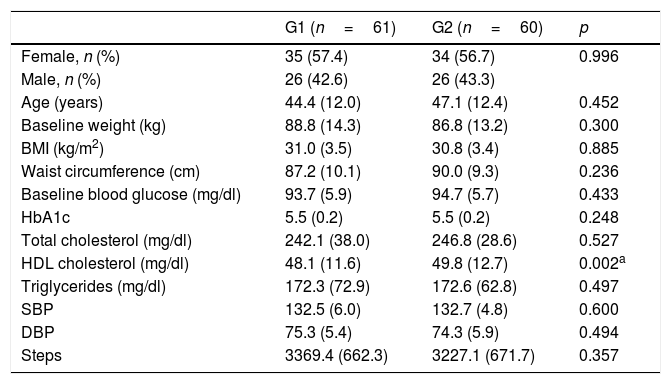
ResultsA total of 123 obese or overweight patients (62 in the G1 IMOAP and 61 in the G2 with iwopi) participated, of which 121 completed the study (61 in G1 and 60 in G2). Mean age 45.55±12.83 years. Sex: 57.2% female and 42.8% male.
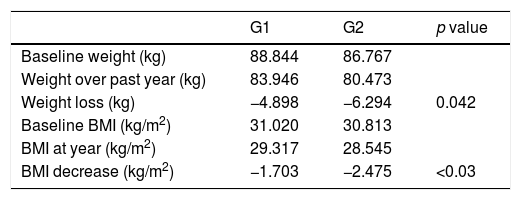
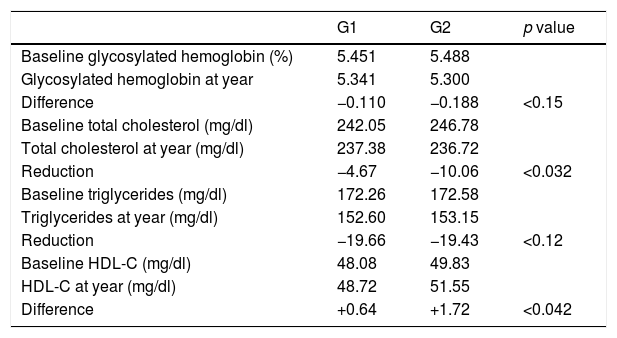
It can be seen how both weight and BMI and the main lipid parameters are reduced in both groups, the difference being significant in weight as well as BMI and TC. TGs are reduced in both groups, with the difference between both groups not being significant (Tables 1 and 2).
Baseline sample data by group.
| G1 (n=61) | G2 (n=60) | p | |
|---|---|---|---|
| Female, n (%) | 35 (57.4) | 34 (56.7) | 0.996 |
| Male, n (%) | 26 (42.6) | 26 (43.3) | |
| Age (years) | 44.4 (12.0) | 47.1 (12.4) | 0.452 |
| Baseline weight (kg) | 88.8 (14.3) | 86.8 (13.2) | 0.300 |
| BMI (kg/m2) | 31.0 (3.5) | 30.8 (3.4) | 0.885 |
| Waist circumference (cm) | 87.2 (10.1) | 90.0 (9.3) | 0.236 |
| Baseline blood glucose (mg/dl) | 93.7 (5.9) | 94.7 (5.7) | 0.433 |
| HbA1c | 5.5 (0.2) | 5.5 (0.2) | 0.248 |
| Total cholesterol (mg/dl) | 242.1 (38.0) | 246.8 (28.6) | 0.527 |
| HDL cholesterol (mg/dl) | 48.1 (11.6) | 49.8 (12.7) | 0.002a |
| Triglycerides (mg/dl) | 172.3 (72.9) | 172.6 (62.8) | 0.497 |
| SBP | 132.5 (6.0) | 132.7 (4.8) | 0.600 |
| DBP | 75.3 (5.4) | 74.3 (5.9) | 0.494 |
| Steps | 3369.4 (662.3) | 3227.1 (671.7) | 0.357 |
The results are expressed as an average (standard deviation) or absolute (relative) frequencies.
The averages were compared using path variance analysis and the a posteriori comparison between the groups using the Bonferroni test. The comparison between the proportions with the chi-squared test.
cm: centimetres; G1: IMOAP (structured motivational intervention) group; G2: IMOAP group to which the physical activity platform is added; HbA1c: glycosylated hemoglobin; HDL: high density lipoproteins; BMI: body mass index; kg/m2: kilograms divided by height in square meters; kg: kilograms; mg/dl: milligrams per deciliter; DBP: diastolic blood pressure; SBP: systolic blood pressure.
List of baseline and post-intervention anthropometric parameters.
| G1 | G2 | p value | |
|---|---|---|---|
| Baseline weight (kg) | 88.844 | 86.767 | |
| Weight over past year (kg) | 83.946 | 80.473 | |
| Weight loss (kg) | −4.898 | −6.294 | 0.042 |
| Baseline BMI (kg/m2) | 31.020 | 30.813 | |
| BMI at year (kg/m2) | 29.317 | 28.545 | |
| BMI decrease (kg/m2) | −1.703 | −2.475 | <0.03 |
The HDL-C increases in both groups, making it more in the motivated exercise group with significant difference.
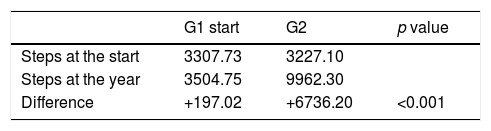
The physical activity of the group with motivated physical activity program intervention is 3 times higher than the group without intervention (Table 3).
Main analytical parameters.
| G1 | G2 | p value | |
|---|---|---|---|
| Baseline glycosylated hemoglobin (%) | 5.451 | 5.488 | |
| Glycosylated hemoglobin at year | 5.341 | 5.300 | |
| Difference | −0.110 | −0.188 | <0.15 |
| Baseline total cholesterol (mg/dl) | 242.05 | 246.78 | |
| Total cholesterol at year (mg/dl) | 237.38 | 236.72 | |
| Reduction | −4.67 | −10.06 | <0.032 |
| Baseline triglycerides (mg/dl) | 172.26 | 172.58 | |
| Triglycerides at year (mg/dl) | 152.60 | 153.15 | |
| Reduction | −19.66 | −19.43 | <0.12 |
| Baseline HDL-C (mg/dl) | 48.08 | 49.83 | |
| HDL-C at year (mg/dl) | 48.72 | 51.55 | |
| Difference | +0.64 | +1.72 | <0.042 |
There is a significant relationship between the increase in activity and weight loss (p<0.001), also between it and decreased cholesterol. The increase in physical activity also produces a significant increase in HDL-C.
DiscussionThis study has shown that one year after applying 2 weight-loss methods, both groups were successful, although weight loss was more intense in the moderate physical activity group (G2) than in the control group. Meanwhile, without any other kind of intervention, it was observed that the majority of patients with dyslipidemia linked to obesity progressed positively (decrease in TC and TG and increase in HDL-C), although the average values decreased significantly, with these values being greatest in the group who experienced the greatest weight loss, which is in line with these results. In other words, weight loss results in a positive change in the lipid parameters linked to obesity and this change is more extreme the more weight is lost. On average, this was based on a population with TC and TG above the optimum cut-off values (Table 1) and the changes observed were equally greater in the intervention group (G2) than in the recognized control group (G1). Given that the changes in weight were modest, but still significant, small changes in the lipid parameters may also be expected. In our study we can see how the groups with the greatest weight loss also have the greatest reduction in TC and TG and increase in HDL-C, which are not proportional to the drop in TG, which confirms that the lipid parameters most associated with physical activity are TC and HDL-C.
Physical activity is an effective tool to modify the lipid profile, acting significantly on the HDL-C indices and the reduction of cholesterol linked to low-density lipoproteins and serum TGs. In a meta-analysis performed by Kelley et al.,23 it was shown that physical activity in only 8 weeks was able to significantly increase the values of HDL-C in adults over 18 years. Our study presents HDL-C elevations of 0.64 and 1.72, which although they are discrete increases, if this observation were applied to our results, the increase in the level of HDL-C through the exercise determined by this analysis would result in a reduction of the risk of CVD of approximately 5.1% in men and 7.6% in women; this is potentially of importance in cardiovascular prevention, which is reduced by increasing the level of HDL-C. This is in accordance with a meta-analysis performed by Kodama et al.,24 which indicated that the effect of aerobic training resulted in an increase of 2.53mg/dl of HDL-C. In a prior observational study,23 each increase of 1mg/dl (0.026mmol/l) in the level of HDL-C, it was reported as associated with a 2 and 3% decrease in the risk of CVD in men and women, respectively. However, the modest elevation in the level of HDL-C showed that this analysis is of clinical importance and was not far from the previous meta-analysis findings in which Kelley et al.25 and Halbert et al.26 reported average net elevations in the level of HDL-C of 1.2mg/dl and 1.9mg/dl, respectively.
The adherence by both groups is high, since there has been only one loss of a patient in each group.
Our study has several strong points. We use very strict inclusion criteria, which allowed the extraction of effects of physical exercise with minimal effects of confounding factors. For example, there were no significant changes in dietary intake. Therefore, we could more accurately assess the relationship between exercise itself and the increases in the level of HDL-C. This approach is essential and practical because most people have limitations on volume or time to exercise (Table 4).
ConclusionsTo conclude, we can confirm that G1, with intensive, permanent tmnt, presents good results that improve with the inclusion of a motivated physical activity program and although telemedicine opens up an interesting opportunity; the use of new information technologies in the field of healthcare (already accessible for almost all patients), that facilitate doctor–patient communication and improve cost-effectiveness, as well as being an instrument of great help in consultations, especially in Primary Care.
The average net increase in the level of HDL-C by exercise itself was modest, but highly significant and more when it is related to cardiovascular risk.
Conflict of interestsThe authors declare that they have no conflicts of interests.
Please cite this article as: Madrona Marcos F, Panisello Royo JM, Tarraga Marcos ML, Rosich N, Carbayo Herencia JA, Alins J, et al. Efecto de un programa de actividad física motivada en los parámetros lipídicos de pacientes con obesidad o sobrepeso. Clín Investig Arterioscler. 2019;31:245–250.