To determine the relation between epicardial fat thickness and coronary in-stent restenosis in patients with acute myocardial infarction and percutaneous coronary intervention.
MethodsA prospective study was conducted, which included 129 patients (67.3% male, mean age 62.9±10 years) with ST segment elevation acute myocardial infarction undergoing primary percutaneous coronary intervention with bare metal stent. Patients were divided in two groups according to the presence (n=21) or not (n=108) of in-stent restenosis during one year follow-up.
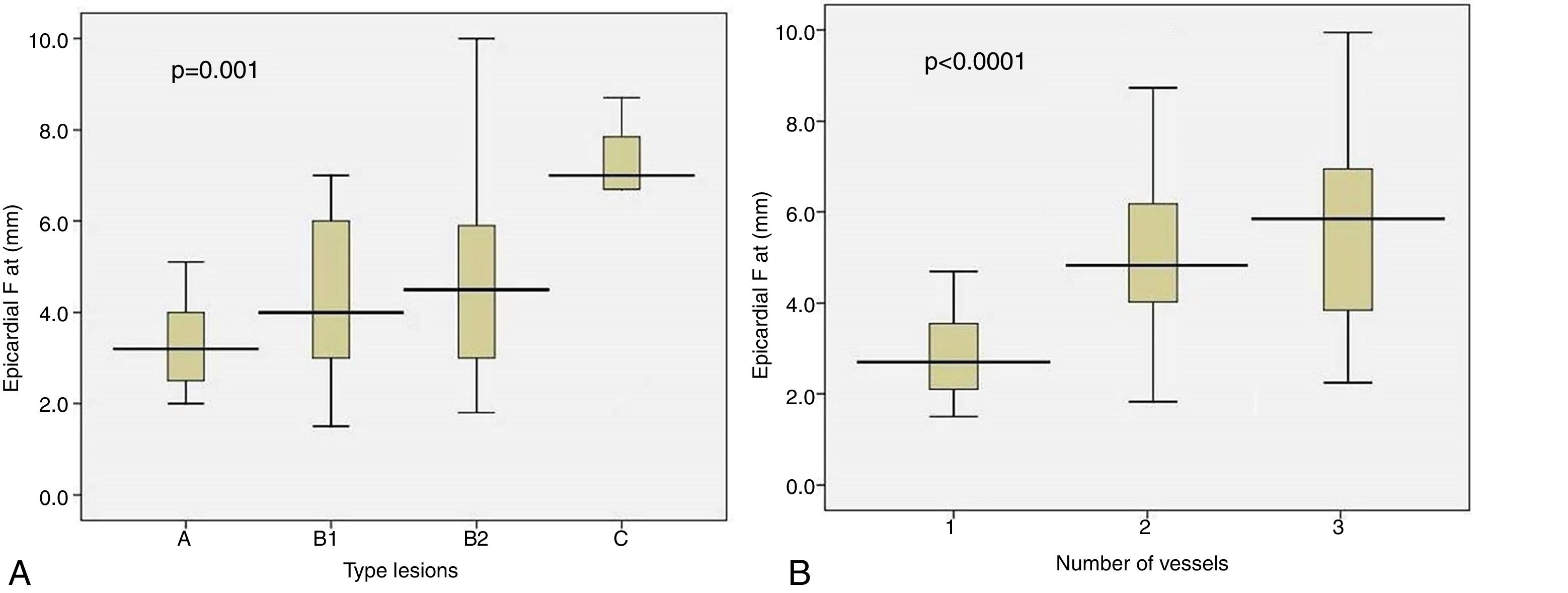
ResultsEpicardial fat was significantly thicker in patients with coronary in-stent restenosis (5.51±1.6 vs 4.14±2.0mm, p=0.006). A proportionally and significantly thicker epicardial fat was found according to the increase in coronary disease severity (3.3±0.9mm vs 4.3±1.8mm vs 4.7±2.3mm vs 6.7±2.2mm, for type A, B1, B2 and C lesions, respectively, p=0.001) and number of vessels (3.07±1.2mm vs 4.92±1.8mm vs 5.43±2.2mm, for one, two and three vessels disease, respectively, p<0.0001). Epicardial fat thickness ≥4.7mm had 75.0% sensibility and 69.0% specificity for predicting restenosis (AUC=0.737).
ConclusionsEchocardiographic evaluation of epicardial fat thickness could identify those patients with acute myocardial infarction with greater probabilities of in-stent restenosis after percutaneous coronary intervention.
Determinar la relación entre el grosor de la grasa epicárdica y la reestenosis del stent en pacientes con infarto agudo de miocardio e intervención coronaria percutánea.
MétodosSe realizó un estudio prospectivo en 129 pacientes (67,3% del sexo masculino, edad media: 62,9±10 años) con diagnóstico de infarto agudo de miocardio con elevación del ST e intervención coronaria percutánea primaria con stent metálico convencional, divididos en 2 grupos según presencia (n=21) o no (n=108) de reestenosis durante un año de seguimiento posterior a la intervención.
ResultadosLa grasa epicárdica fue significativamente mayor en los pacientes con reestenosis del stent (5,51±1,6 vs. 4,14±2,0mm; p=0,006), aumento en la severidad de la lesión angiográfica (3,3±0,9vs. 4,3±1,8vs. 4,7±2,3vs. 6,7±2,2mm, para lesiones tipo A, B1, B2 y C, respectivamente; p=0,001) y el número de vasos enfermos (3,07±1,2vs. 4,92±1,8vs. 5.43±2.2mm, para uno, 2 y 3 vasos, respectivamente; p<0,0001). La grasa epicárdica ≥4,7mm mostró una sensibilidad del 75,0% y una especificidad del 69,0% en la predicción de reestenosis (área bajo la curva de 0,737).
ConclusionesLa evaluación ecocardiográfica de la grasa epicárdica puede identificar pacientes con infarto agudo de miocardio con mayores probabilidades de reestenosis del stent después de una intervención coronaria percutánea.
Epicardial fat is an endocrine organ that secretes inflammatory hormones and cytokines with a fundamental role in the pathogenesis of coronary atherosclerosis, especially due to its proximity to the adventitia of the coronary arteries and the underlying myocardium.1 As there is no fascia that separates the epicardial adipose tissue from the myocardium and the coronary vessels, both structures are in intimate contact. Therefore, it has been postulated that the migration of cells and the diffusion of secreted molecules between these adjacent structures can occur, serving as an argument to explain the causal relationship between the amount of epicardial fat and the presence or not of atherosclerosis in the coronary arteries.2
The relationship of epicardial fat with the metabolic syndrome, subclinical atherosclerosis, glucose tolerance, insulin resistance, blood pressure levels, various inflammatory markers and the presence of significant coronary artery disease (CAD) suggest that this echocardiographic marker can be extremely useful in the cardiovascular risk stratification during daily clinical practice.3 However, the relationship of epicardial fat with stent restenosis after coronary angioplasty and the use of this echocardiographic marker in the prediction of restenosis has hardly been addressed, because of the few and contradictory existing evidence and the absence of studies with conventional metallic stent implantation.
The search for new tools to identify patients with higher probabilities of restenosis after a percutaneous transluminal coronary angioplasty (PTCA) is of particular interest, taking into account that the use of conventional metallic stent, for which higher rates of restenosis (20–30%) compared to drug-eluting stents (<10%) has been described, continues to be the first option in terms of cost for developing countries. The objective of this study is to determine the relationship between epicardial fat thickness and bare metal stent restenosis in patients with primary PTCA after ST elevation myocardial infarction (STEMI).
Materials and methodsStudy populationA prospective study was conducted, which included 129 patients (67.3% male, mean age 62.9±10 years) with ST segment elevation acute myocardial infarction undergoing primary percutaneous coronary intervention (PCI) with bare metal stent at the National Institute of Cardiology and Cardiovascular Surgery between January 2012 and January 2014, with one year follow up after PCI, which were divided in two comparison groups according to the presence (n=21) or not (n=108) of in-stent restenosis. We excluded those patients with: (1) previous PCI or coronary artery bypass grafting and (2) coronary anatomy suitable for surgical myocardial revascularization.
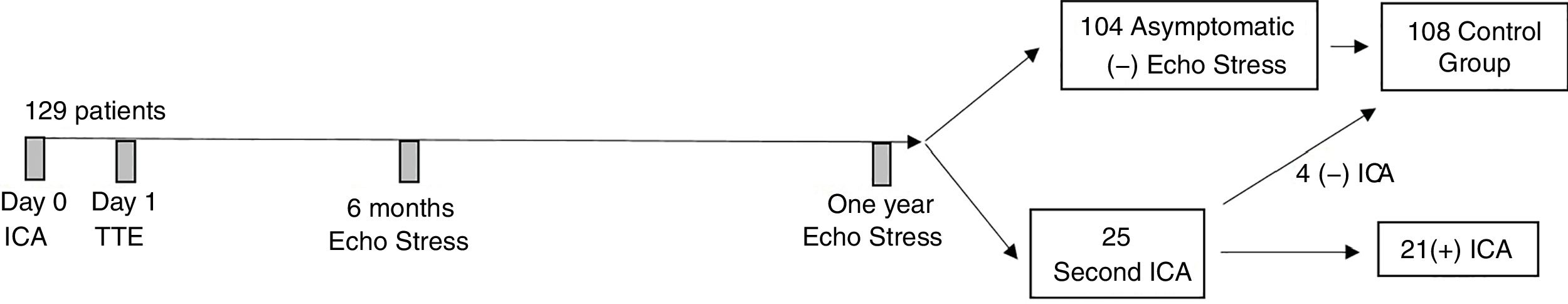
Study designOnce the invasive coronary angiography (IC) was performed, clinical, anthropometric and biochemical variables were acquired during the hospital stay. The echocardiographic examination was performed the day after the IC by an echocardiographer who was blinded to the subject's clinical and angiographic data. All patients received an echo stress imaging at six months and one year after performing the PTCA. Twenty five patients (of which 21 patients had angiographic confirmed restenosis) underwent a second IC during one-year follow-up for the following reasons: (1) seven patients due to recurrent exertion angina; (2) six patients due to unstable angina and (3) 12 patients due to positive stress imaging test. The remaining 104 patients not undergoing a second IC were asymptomatic with negative echo stress imaging during follow-up (Fig. 1).
We included clinical (age, sex, current smoking, arterial hypertension, dyslipidemia, diabetes and infarction location), anthropometrical (waist circumference and body mass index), biochemical (glucose, total cholesterol, triglycerides, uric acid and creatinine), echocardiographic (epicardial fat thickness, left-ventricular ejection fraction, segmentary wall motion score, LV end-diastolic and end-systolic volumes) and angiographic variables (number of vessels, ACC/AHA classification lesion type, number of stents, as well as stent length and diameter).
Blood chemistry testingA 10-ml blood sample was withdrawn from the cubital vein and blood was transferred into three tubes: one with EDTA, another with heparin and a serum tube with gel separator. Fasting blood glucose, total cholesterol, HDL-C, low density lipoprotein cholesterol (LDL-C) and triglycerides were determined. Blood glucose, total cholesterol and triglycerides were assayed using RapiGluco-Test, Colestest and Monotriglitest reagents, respectively, manufactured by the “Carlos J. Finlay” Enterprise of Biological Products, Havana, Cuba. An enzymatic colorimetric assay was used to measure blood glucose in an Eppendorf device and cholesterol, triglycerides and uric acid were determined with a Hitachi 7170A (Tokyo, Japan) blood analyzer. HDL-C and LDL-C were measured using HDL-C Inmuno FS and LDL-C Select FS reagents, by in vitro serum or plasma quantitative determination in photometric systems (immunoturbidimetric assays) manufactured by DiaSys Diagnostic Systems GmbH, Holzheim, Germany).
Echocardiographic parametersTransthoracic echocardiographic examinations were performed using a Philips iE33 2006 (USA) cardiac ultrasound machine (version 2.0.1.420, S5-1 transducer with 1.3–3.6MHz phase array), with patients in the left lateral decubitus position. Concurrent electrocardiographic monitoring was provided during echocardiographic studies.
Echocardiographic epicardial fat thickness was measured according to the method previously described and validated.4 Epicardial fat was identified as the echo-free space between the outer wall of the myocardium and the visceral layer of pericardium. Epicardial fat thickness was measured perpendicularly on the free wall of the right ventricle at end-systole in three cardiac cycles. Maximum epicardial fat thickness was measured at the point on the free wall of the right ventricle along the midline of the ultrasound beam, perpendicular to the aortic annulus, used as anatomical landmark for this view. The average value of three cardiac cycles from each echocardiographic view was considered.
Left ventricular volumes were measured from the apical four-chamber view using the biplane Simpson's method.
Segmental wall motion abnormalities were assessed according to Cerqueira et al.5 recommendations.
Coronary angiography dataCoronary angiographic analysis was performed by two experienced invasive cardiologists using Judkin's method, following the percutaneous puncturing of the femoral artery or via a radial artery approach and digitally recorded by a Hicor system (Siemens, Munich, Germany). Coronary lesions were evaluated from at least two orthogonal views. CAD was defined as the presence of one or more stenoses ≥50% in diameter of a major epicardial vessel. The extent of CAD was quantified according to the number of vessels with ≥50% stenosis.
Statistical analysisStatistical analysis was performed using SPSS 16.0 statistical Software (SPSS Inc., Chicago, IL, USA). Continuous variables are expressed as means±SD and categorical variables as absolute numbers and percentages. Comparisons of continuous variables were performed using unpaired Student t test. Categorical variables were compared with the chi-square test. Multivariate analysis was performed using a multiple linear regression model including potential confounders (variables with p value <0.20 in the univariate analysis). Level of significance was set at p<0.05.
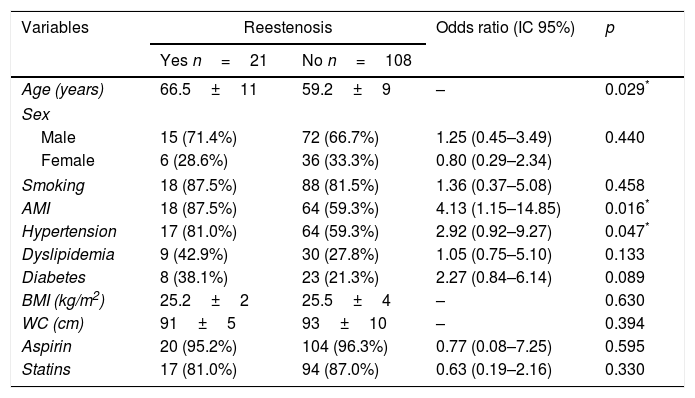
ResultsPatients with stent restenosis showed a more advanced age (66.5±11 vs 59.2±9 years, p=0.029) and a significantly higher percentage of arterial hypertension (81.0% vs 59.3%, p=0.047) and anterior location of AMI (87.5% vs 59.3%, p=0.016). The percentage of patients with a history of dyslipidemia and diabetes was also higher in those with restenosis, although these differences were not significant (Table 1).
Clinical and anthropometrical variables according to in-stent restenosis.
| Variables | Reestenosis | Odds ratio (IC 95%) | p | |
|---|---|---|---|---|
| Yes n=21 | No n=108 | |||
| Age (years) | 66.5±11 | 59.2±9 | – | 0.029* |
| Sex | ||||
| Male | 15 (71.4%) | 72 (66.7%) | 1.25 (0.45–3.49) | 0.440 |
| Female | 6 (28.6%) | 36 (33.3%) | 0.80 (0.29–2.34) | |
| Smoking | 18 (87.5%) | 88 (81.5%) | 1.36 (0.37–5.08) | 0.458 |
| AMI | 18 (87.5%) | 64 (59.3%) | 4.13 (1.15–14.85) | 0.016* |
| Hypertension | 17 (81.0%) | 64 (59.3%) | 2.92 (0.92–9.27) | 0.047* |
| Dyslipidemia | 9 (42.9%) | 30 (27.8%) | 1.05 (0.75–5.10) | 0.133 |
| Diabetes | 8 (38.1%) | 23 (21.3%) | 2.27 (0.84–6.14) | 0.089 |
| BMI (kg/m2) | 25.2±2 | 25.5±4 | – | 0.630 |
| WC (cm) | 91±5 | 93±10 | – | 0.394 |
| Aspirin | 20 (95.2%) | 104 (96.3%) | 0.77 (0.08–7.25) | 0.595 |
| Statins | 17 (81.0%) | 94 (87.0%) | 0.63 (0.19–2.16) | 0.330 |
AMI: anterior myocardial infarction; BMI: body mass index; WC: waist circumference.
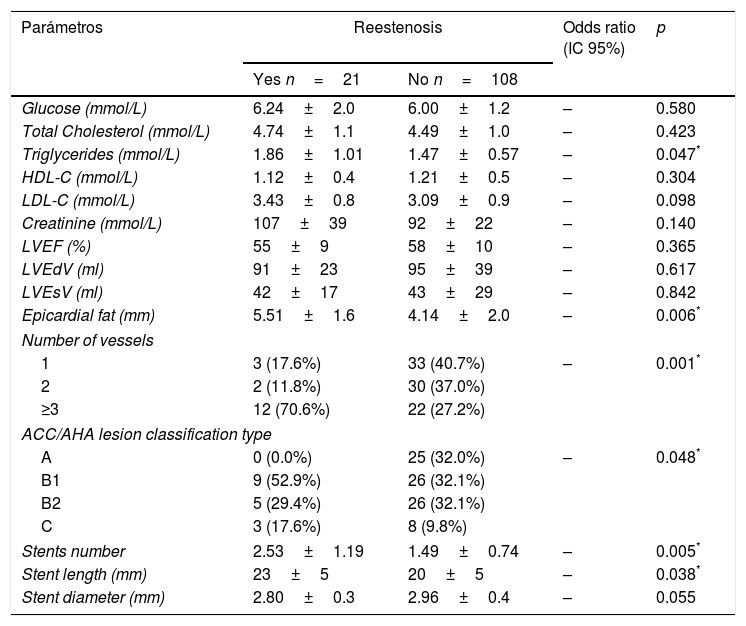
The epicardial fat thickness was significantly higher in patients with stent restenosis (5.51±1.6 vs 4.14±2.0mm, p=0.006). Likewise, the levels of triglycerides, uric acid, the percentage of patients with disease of three or more vessels, the lesion type, the number of stents and the stent length, were significantly related to restenosis at one year of follow-up (Table 2).
Biochemical, echocardiographic and angiographic parameters according to in-stent restenosis.
| Parámetros | Reestenosis | Odds ratio (IC 95%) | p | |
|---|---|---|---|---|
| Yes n=21 | No n=108 | |||
| Glucose (mmol/L) | 6.24±2.0 | 6.00±1.2 | – | 0.580 |
| Total Cholesterol (mmol/L) | 4.74±1.1 | 4.49±1.0 | – | 0.423 |
| Triglycerides (mmol/L) | 1.86±1.01 | 1.47±0.57 | – | 0.047* |
| HDL-C (mmol/L) | 1.12±0.4 | 1.21±0.5 | – | 0.304 |
| LDL-C (mmol/L) | 3.43±0.8 | 3.09±0.9 | – | 0.098 |
| Creatinine (mmol/L) | 107±39 | 92±22 | – | 0.140 |
| LVEF (%) | 55±9 | 58±10 | – | 0.365 |
| LVEdV (ml) | 91±23 | 95±39 | – | 0.617 |
| LVEsV (ml) | 42±17 | 43±29 | – | 0.842 |
| Epicardial fat (mm) | 5.51±1.6 | 4.14±2.0 | – | 0.006* |
| Number of vessels | ||||
| 1 | 3 (17.6%) | 33 (40.7%) | – | 0.001* |
| 2 | 2 (11.8%) | 30 (37.0%) | ||
| ≥3 | 12 (70.6%) | 22 (27.2%) | ||
| ACC/AHA lesion classification type | ||||
| A | 0 (0.0%) | 25 (32.0%) | – | 0.048* |
| B1 | 9 (52.9%) | 26 (32.1%) | ||
| B2 | 5 (29.4%) | 26 (32.1%) | ||
| C | 3 (17.6%) | 8 (9.8%) | ||
| Stents number | 2.53±1.19 | 1.49±0.74 | – | 0.005* |
| Stent length (mm) | 23±5 | 20±5 | – | 0.038* |
| Stent diameter (mm) | 2.80±0.3 | 2.96±0.4 | – | 0.055 |
LVEF: left ventricular ejection fraction; LVEdV: left ventricular end-diastolic volume; LVEsV: left ventricular end-sistolic volume; SMS: score de motilidad segmentaria.
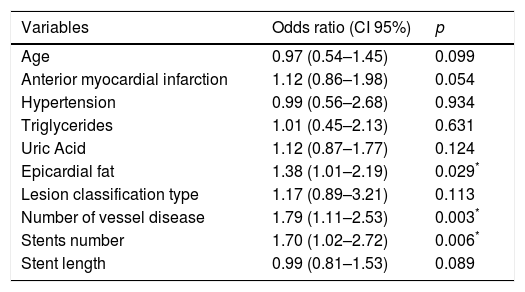
Of the variables that showed a significant relation with stent restenosis in the univariate analysis, only the number of diseased vessels, the number of stents and epicardial fat thickness, maintained a significant and independent association in multivariable analysis (Table 3).
Multivariable analysis of variables related to in-stent restenosis.
| Variables | Odds ratio (CI 95%) | p |
|---|---|---|
| Age | 0.97 (0.54–1.45) | 0.099 |
| Anterior myocardial infarction | 1.12 (0.86–1.98) | 0.054 |
| Hypertension | 0.99 (0.56–2.68) | 0.934 |
| Triglycerides | 1.01 (0.45–2.13) | 0.631 |
| Uric Acid | 1.12 (0.87–1.77) | 0.124 |
| Epicardial fat | 1.38 (1.01–2.19) | 0.029* |
| Lesion classification type | 1.17 (0.89–3.21) | 0.113 |
| Number of vessel disease | 1.79 (1.11–2.53) | 0.003* |
| Stents number | 1.70 (1.02–2.72) | 0.006* |
| Stent length | 0.99 (0.81–1.53) | 0.089 |
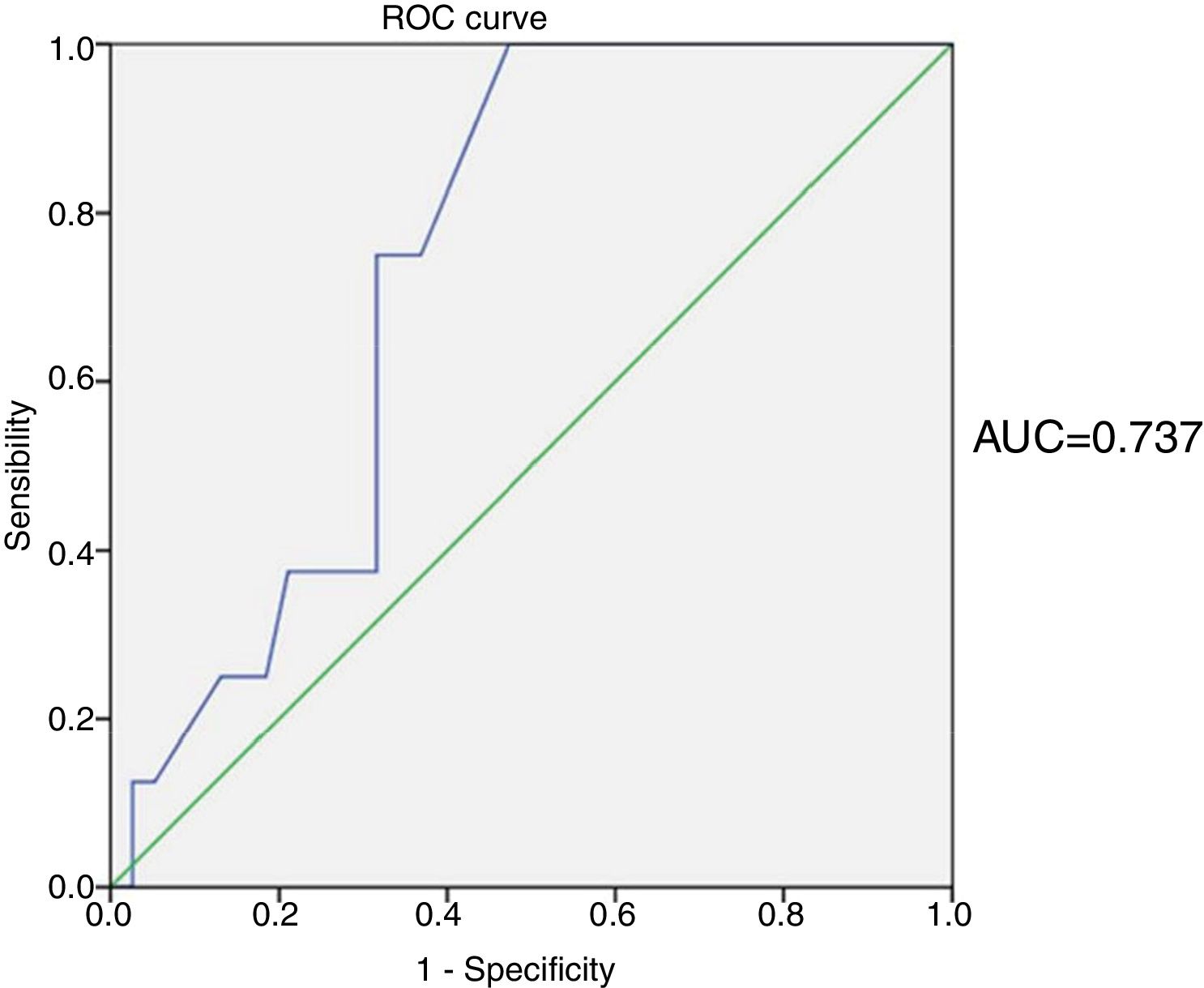
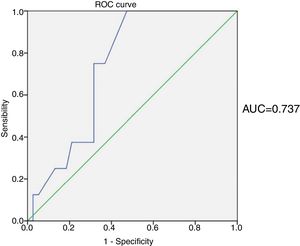
The area under the ROC curve of the epicardial fat values in the prediction of stent restenosis was 0.737. The epicardial fat ≥4.7mm showed a sensitivity of 75.0% and specificity of 69.0% in the prediction of restenosis (Fig. 2).
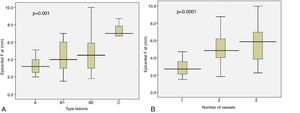
A proportional and significant increase of the epicardial fat thickness was found according to the increase in the severity of the angiographic lesion (3.3±0.9mm vs 4.3±1.8mm vs 4.7±2.3mm vs 6.7±2.2mm, for type A lesions, B1, B2 and C, respectively, p=0.001) and the number of vessels (3.07±1.2mm vs 4.92±1.8mm vs 5.43±2.2mm, for one, two and three vessels, respectively, p<0.0001) (Fig. 3).
DiscussionThe most important findings of the present study are: (1) epicardial fat shows a significant relationship with in-stent restenosis and (2) has an acceptable accuracy in the prediction of restenosis.
The first studies that addressed the relationship between epicardial fat and the presence, extent and severity of CAD, compared with clinical and anthropometric variables, began to be published at 2006.6–9
In Cuban patients, Mustelier et al.10 showed a significant relationship between increased epicardial fat thickness and the presence of CAD. Other studies carried out in Cuba have also shown the relationship of epicardial fat with subclinical carotid atherosclerosis and coronary artery calcification in patients with metabolic syndrome,11 insulin resistance12 and asymptomatic adults.13
Multiple studies conducted in the last decade indicate that inflammatory mechanisms play a central role in the process of neoproliferation of the intima that leads to restenosis after the implantation of an intracoronary stent. The cellular damage caused by stent implantation seems to be a triggering factor for the release of chemotactic molecules, such as IL-1, IL-6 and TNF-α by endothelial cells and leukocytes, causing intra stent inflammatory cell recruitment.14
In this regard, it has been pointed out that the presence of inflammatory cells in the epicardial adipose tissue could occur in response to a plaque rupture (like in the angioplasty process) and lead to the amplification of vascular inflammation and even to the plaque instability, through processes of apoptosis and neovascularization.15 This process of amplification of the inflammatory phenomenon would justify the creation of a vicious circle in which the increase in sustained epicardial fat in time per se would contribute to the progression of the coronary atherosclerosis after PCI was performed, but the stenting process itself, with the consequent plaque fracture, could further promote the dysfunction and inflammation of the perivascular adipose tissue at the site of the stenosis due to a reverse phenomenon.15
In this sense, Spener et al.16 demonstrated a lower production of adiponectin in epicardial adipose tissue obtained by biopsy of areas near the coronary stent implantation site, in comparison with distant areas in untreated arteries, in samples from the same patient. Park et al.17 enrolled 60 patients with CAD studied by intravascular ultrasound, which were divided into two groups according to epicardial fat thickness greater or less than 3.5mm. Patients with greater epicardial fat thickness showed thinner fibroatheromatous plaques and greater plaques number, as well as a greater volume of the lipid nucleus. These evidences also suggest that epicardial fat thickness increase is related to a greater vulnerability and instability of the atheroma plaque.
In the first study carried out with the aim of evaluating the possible relationship between epicardial fat and stent restenosis, Nikaeen et al.18 included 117 patients treated with drug-eluting stents, in whom no difference of epicardial fat thickness was demonstrated between both comparison groups, according to presence or not of restenosis.
Park et al.19 included 407 patients who had received PCI, with a follow-up of two years. Similar to our results, the epicardial fat thickness was significantly higher in the group of patients with restenosis (3.7mm vs 3.0mm, p=0.001), with significantly less restenosis-free survival in those with greater epicardial fat thickness.
Zhou et al.20 reported in 364 patients undergoing 64-slice coronary computed tomography angiography, subsequent PCI and coronary angiography follow-up, a significantly increased epicardial fat volume in patients with in-stent restenosis compared with those without restenosis, a relation that remained significant after adjustment for conventional cardiovascular risk factors and angiographic parameters.
On the other hand, Eroglu et al.7 showed that epicardial adipose tissue ≥5.2mm had 85% sensitivity and 81% specificity (area under the ROC curve 0.914, p<0.001) to predict CAD. Similarly, Sade et al.21 found 85% sensitivity and 75% specificity (area under the curve 0.845) for epicardial fat values>4.5mm in the prediction of coronary flow reserve reduction in angiographically normal women. In a study conducted in Cuban patients, Mustelier et al.10 reported an area under the curve of 0.712, with a sensitivity of 65.4% and specificity of 61.5% for epicardial fat≥5.2mm in the prediction of CAD. Although with different objectives, the area under the curve obtained in the present study is slightly higher than the one found in the previous study carried out in Cuba,10 and can be considered acceptable.
Other variables that were significantly and independently related to stent restenosis, in addition to epicardial fat, were the vessels and stents number.
The factors involved in the onset of restenosis are several, among them are: clinical (advanced age, sex, presence of stable and unstable angina, acute myocardial infarction, diabetes mellitus, hypertension, dyslipidemia, obesity and smoking), angiographic factors (proximal lesions, PCI on the main left coronary artery and the anterior descending artery, arteries of small diameter, long stenosis, use of several conventional stents) and factors inherent to the procedure (smaller diameter at the end of PTCA, elastic recoil, neointimal hyperplasia, mural thrombus, among others).22 In this sense, other variables that showed a relationship with stent restenosis in the present study (although only in the univariate analysis) were age, anterior location of myocardial infarction, history of hypertension, triglycerides and uric acid levels, as well as the type of lesion and the stent length.
ConclusionsThe result of this study not only demonstrate the relationship of epicardial fat thickness increase with a greater probability of restenosis in patients with STEMI treated with bare metal stent, but also provides an acceptable restenosis predictive value for those patients with epicardial fat≥4.7mm.
Study limitationsLimitations of this study includes: (1) the small sample size, which is why future studies with larger, multi-ethnic populations are needed to generalize the results found and (2) the lack of angiographic follow-up because it was not performed routinely but was left to the clinical judgment of the responsible cardiologist, based on patient clinical data and the results of stress imaging test, which may have included false controls with restenosis. However, overall negative predictive value for echo stress in the detection of restenosis has been declared as high as 97%.23
Conflicts of interestsNone.