Los estudios cualitativos muestran que las personas que padecen sensibilidad química múltiple (SQM), o intolerancia ambiental idiopática, piensan que existe una falta de conciencia por parte de los profesionales sanitarios acerca de la enfermedad, lo que dificulta la comunicación. El objetivo de este trabajo es describir el sufrimiento de las personas que padecen SQM y evaluar la repercusión de la enfermedad en cada dimensión del sufrimiento, mediante un estudio descriptivo y correlacional. Una muestra compuesta por 125 personas cumplimentaron una encuesta de tres escalas que miden el impacto de la SQM y tres escalas que miden el sufrimiento. Los resultados revelan que la SQM afecta sobre todo a mujeres. La evaluación mediante el Inventario Rápido de Exposición y Sensibilidad al Entorno (QEESI) mostró que los participantes padecían la enfermedad en grado elevado. La esfera física del sufrimiento es la más afectada, seguida de la psicológica y la existencial. La correlación entre el QUEESI y las escalas de sufrimiento es elevada. La ecuación de regresión multivariada explicaba el 38.2% de la varianza del sufrimiento observada. Se concluye que la SQM produce sufrimiento físico, psicológico y existencial. La gravedad de los síntomas es las variable que más sufrimiento produce, seguido de la repercusión vital. El sufrimiento psicológico se caracteriza por la ansiedad o la preocupación y la falta de alegría. El sufrimiento existencial revela pensamientos de fracaso y falta de armonía interior. La detallada descripción del sufrimiento en la SQM constituye una base útil para la terapia. La carencia de conocimiento entre los profesionales sanitarios provoca falta de atención a estos pacientes por parte de los profesionales sanitarios. Esperamos con esta investigación inducir la toma de conciencia sobre esta enfermedad emergente para así poder mejorar la comunicación entre el personal sanitario y los pacientes.
Qualitative studies show that patients suffering from Multiple Chemical Sensitivity (MCS) or Idiopathic Environmental Intolerance (IEI) are aware of health-care professionals' non-awareness of the disease, making communication difficult. The objective of this paper is to describe the suffering in individuals with MCS and to assess the disease's impact on each measured dimension of suffering by means of a descriptive and correlational study. A sample of 125 subjects fill out a survey consisting of three scales for assessing the impact of MCS and three scales for assessing suffering. The results show that MCS affects mostly women. Assessment with the Quick Environmental Exposure and Sensitivity Inventory (QEESI) showed that participants have high levels of disease. The physical sphere of suffering is the most affected, followed by the psychological and the existential. There are high correlations between the QEESI and suffering scales. A multivariate regression equation explained 38.2% of the variance of suffering observed. We conclude that MCS generates physical, psychological, and existential suffering. Severity of symptoms is the variable that generates most suffering, followed by life impact. Psychological distress is marked by anxiety or worry and lack of gaiety; existential suffering reveals thoughts of failure and lack of inner harmony. A detailed description of suffering in MCS is a useful basis for therapy. Lack of awareness among health-care personnel implies inattention of these patients within the general health-care service. With this investigation we hope to raise awareness of this emerging disease in order to improve the communication between health-care workers and patients.
Multiple Chemical Sensitivity (MCS), also termed Idiopathic Environment Intolerance (IEI) is a term used to describe a set of physical, cognitive, and emotional symptoms that appear when a person is exposed to low levels of a large variety of environmental chemicals including perfumes, household cleaning products, and paints which, prior to the onset of the disease, were well tolerated. In Spain the estimated prevalence is between 0.2% and 4% (Arnold et al., 2011).
Randolph (1954) highlighted that exposure to certain environmental chemicals could be the cause of a syndrome characterized by a variety of symptoms which, in current terms, would correspond to MCS. Later, Cullen (1987) described the syndrome as an "acquired disorder characterized by recurrent symptoms referable to multiple systems, occurring in response to many chemical unrelated compounds at doses far below those established as causing harmful effects in the general population". This definition has been subjected to many objections and suggestions that attempted to refine and/or broadened it (Labarge & McCaffrey, 2000). Thus, a group of 89 clinicians and researchers with different views of the etiology of the disease established 5 diagnostic criteria to define MCS (Nethercott , Davidoff, Curbow, & Abbey, 1993). These were: 1) the condition must be chronic; 2) the symptoms should be reproducible; 3) the response should occur at low exposure levels; 4) the response needs to be to multiple chemical substances; and 5) the response is improved when the trigger substance is removed. Bartha et al. (1999) included a 6th criterion, i.e., the symptomatology should involve multiple organ systems. These 6 criteria (5 +1) are known as the Consensus Criteria.
The range of physical symptoms associated with MCS is very broad and related to multiple systems. In a systematic review conducted by Labarge & McCaffrey (2000) 151 symptoms were identified that were especially related to the central nervous system (CNS) and respiratory and gastrointestinal tracts. Subsequent studies (Lacour, Zunder, Schmidtke, Vaith, & Scheidt , 2005) highlighted the prevalence of non-specific symptoms related with the CNS such as headache, fatigue, and cognitive deficits. More recently, Nogué et al. (2007) in a study involving 52 cases found that the predominant symptoms were irritation of the oropharyngeal mucosa and breathing problems. In the same study, they found that people were mostly intolerant to chemical products found in household cleaning items, as well as perfumes and toiletries. Gibson and Vogel (2009) established that most of the symptoms were caused by pesticides, formaldehyde, fresh paint, new carpets, gasoline fumes, fragrances, and air fresheners. A further 29 chemicals that were associated with symptoms in the study participants were also listed.
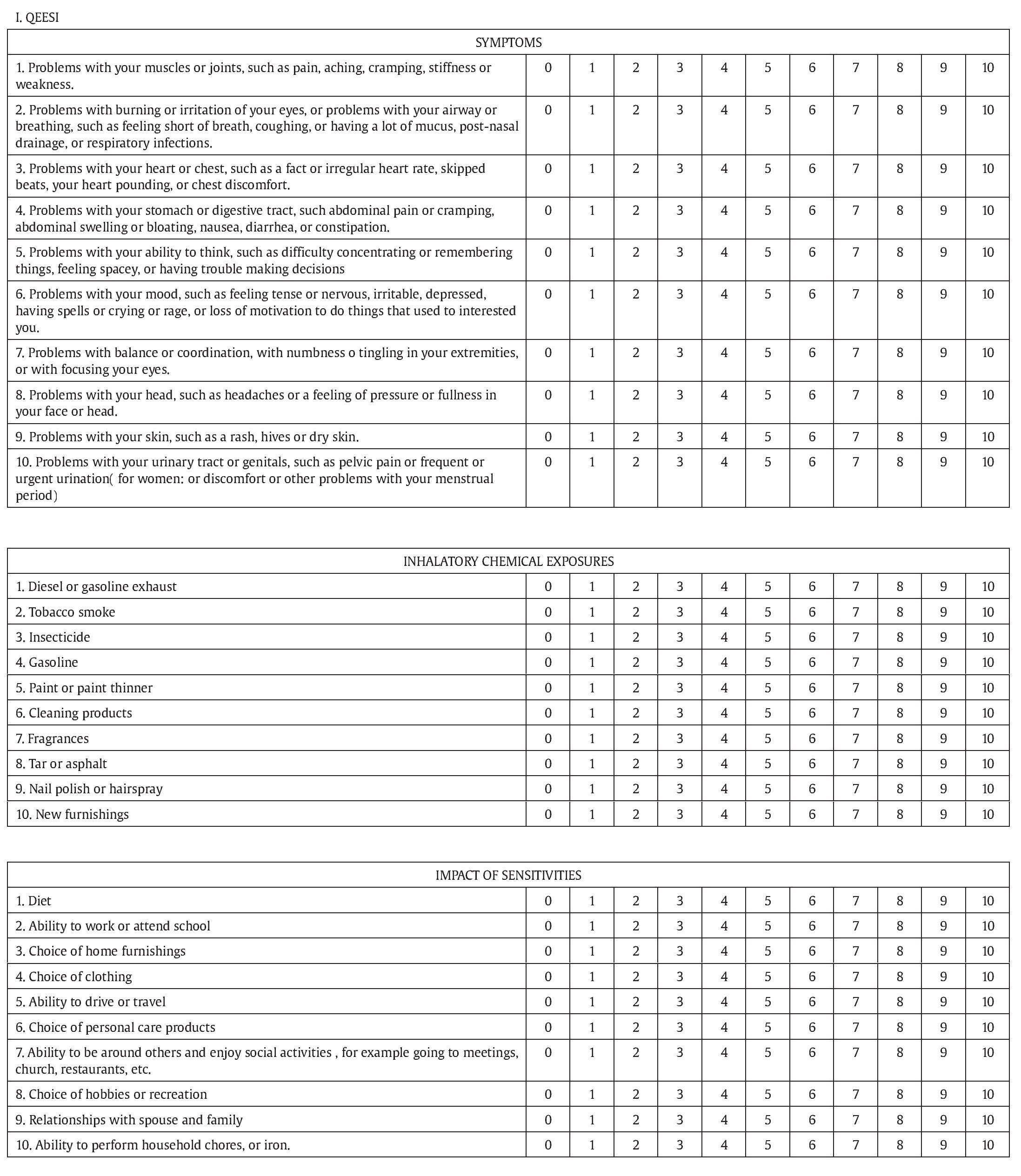
The etiology of MCS is difficult to define since there is no accepted physiopathological mechanism that may explain the clinical symptoms. Hence, the diagnosis of the disease is clinical and is based on the patient's history and clinical examination. Currently, there is the support of an assessment tool called the Quick Environmental Exposure and Sensitivity Inventory (QEESI) which is composed of 5 scales that can help assess the extent of the disease and the chemical triggers (Miller & Prihoda, 1999).
The dearth of physiological markers and diagnostic tests that would facilitate a definitive diagnosis has led to the development of several treatment options, many of them may not have been scientifically validated and, hence, the controversy surrounding MCS continues (Fox, Joffres, Sampalli, & Cas, 2007; Ortega, 2005). Individuals with MCS increasingly resort to alternative treatments and innovative strategies to manage their symptoms. Of considerable note is that the information obtained in informal interviews with the patients indicates that these alternative therapies are valued more highly than those provided by the official state-sponsored National Health System (NHS) and are perceived as being more useful (Koch, Vierstra, & Penix , 2006).
Most studies have focused on evaluating, via qualitative methodology, the impact of MCS on the quality-of-life (QoL) of the individuals involved. Some studies (Gibson, Sledd, McEnroe, & Vos, 2011; Koch, 2006; Skovbjerg, Brorson, Rasmussen, Johansen, & Elberling, 2009) describe the impact of MCS on daily-life activities, as well as the psychological and social effects of daily living while trying to avoid certain chemicals.
As highlighted by patients, routine tasks such as shopping or using public transport can represent an exposure that will induce the symptoms. With respect to social restrictions, the patients emphasize the need for other people to understand their problem, which otherwise could lead to breakdown in relationships and stigmatization; the result could be a lack of openness regarding the condition. Working conditions require adjustments and colleagues' collaboration, and these are not always possible. Of critical importance is that the medical profession is ignorant of the disease or has a low priority for clinical attention.
Nordin, Andersson, and Nordin (2010) described the most commonly used coping strategies of people with MCS. Most strategies focused directly on the problem such as avoiding odorous environments and also requesting that their most intimate colleagues avoid the use of the symptom-inducing perfumes and/or deodorants. However, a resigned acceptance of the situation appears to be most-often chosen. High levels of MCS are associated with the use of problem-focused strategies and mild degrees of disease with emotion-focused strategies. Although this co-occurrence of symptoms and experiences in the person with MCS could contribute to the suffering experienced at some point in the process, we have not encountered any published study evaluating the experience of suffering in this patient population.
Cassell (1982) conceived suffering as a "state of severe distress specifically related to the imminent threats, perceived or actual, to the integrity or existential continuity of the person". Later, Chapman and Gravin (1993) broaden Cassell's definition to include suffering as "an affective and cognitive negative and complex state characterized by negative feelings experienced by a person who is threatened in their integrity, because of their sense of impotence to deal with this threat and exhaustion of personal and psychosocial resources that would deal with it".
Following-up on the definition of Chapman and Gravin (1993), Bayés, Arranz, Barbero, and Barreto (1997) proposed an intervention model known as the "Threat and Resources Model". According to this model, a person suffers if: 1) something happens that he/she perceives as a threat or harm to his/her integrity, or to someone or something considered of vital importance to his/her integrity; and 2) the person assesses his/her resources as being insufficient to cope with the threat.
Recently, Krikorian and Limonero (2012) widened the model proposed by Bayés. They considered that suffering occurs when the perception of threat involves damage to personal integrity, resources, and regulatory processes (including coping strategies and neurophysiological processes involved in the stress response) that are perceived as being insufficient, leading to psycho-social depletion and exhaustion. According to this holistic view, suffering is a global, multi-dimensional (physical, psychological, social, and spiritual), and dynamic experience.
Assessment of suffering is essentially subjective. The causes of suffering, as well as their expression, are varied and dynamic in nature. Hence, the clinical interview appears to be the tool-of-choice, since the patient's experiences are tested directly and individually.
Currently, several instruments and tools that facilitate quantitative assessment of suffering have been developed. The one by Schulz et al. (2010) made a compilation and integration of previously-developed instruments, extracting a set of items that do not overlap and which can be organized in 3 dimensions: physical symptoms, psychological distress, and spiritual or existential aspects.
This construct may be more appropriate than the quality-of-life (QoL) concept used in previous studies because: 1) the QoL is assessed with items that investigators consider as the basis of the problem but which often do not coincide with the patient's perception of what constitutes a threat and causes suffering; 2) QoL dimensions need to be stable, which makes it difficult to approximate to the subjective experience of the sufferer which, by definition, is very changeable; and 3) a person's existential dimension has little influence on QoL evaluation, but is a dimension that could be seriously affected by this disease.
Hence, the main objectives of this study were: to describe suffering in individuals diagnosed with MCS; to identify the dimensions of suffering (using three questionnaires) that contribute the most to the MCS patient's suffering; and to relate any differences in the measured variables to the severity of the disease.
Method
Design
A descriptive, correlational, cross-sectional, quantitative design was used.
Sample
For the present study we carried out convenience sampling, i.e., extended participation to all those individuals who visited the blog "Mi Estrella de Mar" (http://mi-estrella-de-mar.blogspot.com/) between March 27th 2012 and April 12th 2012, and who met the criteria specified below.
The blog "Mi Estrella de Mar" [My Sea Star] is a pioneer space for disseminating information on MCS. It has several quality accreditations, including the Physicians Association, WIS (Web of Health Interest), HON Code, Disability Information Service (Ministry of Health), M21, and Health Documentary. We chose this access path for sample selection because currently, there are no public health centers in Catalonia for the diagnosis and treatment of this disease.
Inclusion criteria:
• Diagnosed as having MCS
• Aged > 18 years
• Informed consent to participation in the study Exclusion criteria
• Pregnant (due to common transient intolerance to odors during pregnancy).
The final sample consisted of 125 persons, of whom 91.2% were women with a mean of 47 years of age and most (84%) living in urban areas.
Instruments
Quick Environmental Exposure and Sensitivity Inventory (QEESI). This questionnaire was created by Claudia Miller and Thomas J. Prihoda in 1999 with the aim of providing the scientific community with a useful tool to assess individuals with MCS, which had not been so far described as an entity. The QEESI is a short version of the Environmental Exposure and Sensitivity Inventory (EESI). It is an instrument with 5 subscales of 10 items each, with 11 Likert response options in 4 of the subscales and 4 options in 1 subscale. Its psychometric properties indicate an internal consistency of between .89 and .97 in the different subscales, together with a sensitivity of 92% and a specificity of 95% as a screening tool for the MCS. It is the questionnaire recommended by the Consensus of 1999 to assess MCS symptoms.
A Spanish version of this questionnaire is available and has been validated. Internal consistency reliability achieved Cronbach's alphas of .94, .96, and .86 for symptom severity scales, chemical intolerances, and impact on QoL respectively.
The Spanish version was used in the current study. Theα values obtained in the Severity Scales, Inhalatory Intolerances, and Life Impact were .864, .938, and .862 respectively.
Currently there are no screening cut-off points for the Spanish version of this questionnaire but the cut-off points recommended by the authors of the original version to detect disease are those that correspond to high scores ≥ 40 on Severity and Intolerances and ≥ 25 on Life Impact. The cut-off points recommended to detect disease-free individuals are those corresponding to low scores ≤ 20, 20, and 10 respectively.
Scales of suffering. The suffering variable has been measured with ad hoc questionnaires made via modifications of the questionnaire proposed by Schulz et al. (2010), which assesses three dimensions of suffering: physical, psychological, and existential.
The physical suffering scale consists of 10 questions with Likert scores of 0 to 3, where 0 is nothing and 3 is a lot. The psychological suffering scale consists of 15 questions with the same options as the previous scale and, finally, existential suffering scale consists of 9 items with responses from 0 to 4, where 0 is nothing and 4 is much.
The evaluation of the psychometric characteristics of the original questionnaire achieved an acceptable reliability (internal consistency and test-retest) and validity (principal component analysis, convergent, and discriminant validity) in the three samples tested by the authors.
For this research we have made some changes in the physical scale, which has been adapted to the symptoms reported by individuals suffering MCS. Also, because of the lack of a Spanish version of the instrument we made a translation, which was back-translated by another person not connected to the study.
The Cronbach alpha obtained in this study for the full scale trial was .934 and for the physical, psychological, and existential dimensions the alpha values were .82, .92, and .89 respectively.
The format of both instruments, QEESI and suffering scales, have been adapted for electronic format and uploaded onto a web platform dedicated to survey management. The first question of the survey was a mandatory question and if the respondents were unable to answer, they were stopped from getting further. The question addressed informed consent, which explained the research's title, the objectives of the study, guarantee of confidentiality, and the requirement for informed consent to participating. The survey was revised and approved by the blog's author.
As control measures, we restricted access to the survey form to only one person/computer, and once a question had been answered progress was made to the next stage. Reversal was not permitted. Questionnaires are annexed.
Procedure
Initially, we contacted the blog's author (María José Moya Villén) to explain the objectives of the project and to request permission to invite participants into the research program via her blog. Once she agreed, she posted a link to the questionnaire on the blog home page "Mi Estrella de Mar" [My Sea Star]. The call for participation was posted across different groups in the social network, including Facebook, the websites of the "Asociación Alicantina para el Estudio de las Intolerancias Alimentarias y Ambientales" [Alicante Association for the Study of Intolerance in Food and Environment] (http://aaeiaa. wordpress.com/), and "Todoalergias" [AllAllergies] (http://www. todoalergias.com/).
Diffusion was made via a pdf document, which provided information concerning the research (aim, questionnaires) and the principal investigator (profession, workplace). Individuals who agreed to participate were linked into the survey and the data sent automatically to the principal investigator. All data were codified to ensure anonymity.
Data Analysis
Completed questionnaires were collected in an Excel 2007 database and analyzed using SPSS (Statistical Package for Social Sciences version 17 for Windows). Descriptive statistics were used to describe the socio-demographic and clinical variables. The degree or extent of disease was evaluated by comparing means of independent samples using Student's t-test. The Pearson correlation coefficient was used to check for associations between variables. Multiple linear regression analyses were applied to establish a predictive model of suffering. A value of p < .05 was considered statistically significant.
Results
Description of the Socio-demographic Characteristics of the Study Sample
The characteristics of participants are summarized in Table 1. Of the 125 participants in the study, 114 were women and 11 were men, aged between 26 and 72 years with a mean age of 47. Most were urban dwellers, well educated (mainly university graduates), predominantly unemployed due to their MCS disability, and married or in a stable partnership. Concomitant diseases included fibromyalgia, chronic fatigue, and other chronic diseases such as hypothyroidism, irritable bowel syndrome, and Sjögren's syndrome among the most prevalent.
Description of Clinical Data: Multiple Chemical Sensitivity
At the time of responding to the survey, the years of disease status ranged between 0 and 30, with a mean of 8.5 (SD = 7.1).
Overall, the degree of disease status was high with a mean score of 235 (SD = 45.2). Table 2 summarizes the different central tendency measures (mean, standard deviation, minimum, and maximum scores) obtained for each of the scales of the QEESI, and for the years of disease progression. The table also contains the overall data subgrouped according to disease severity: moderate (n = 25) and severe (n = 100). Considering the high degree of impact of the disease on the study sample, the cutoff was established as one standard deviation below QEESI mean score, which corresponded to a score of 190.
Comparisons between the two subgroups were statistically significant for all scales of QEESI, as well as for the total score obtained from the sum of the three scales. The difference between the two degrees of severity is not statistically significant for the years of disease progression (Table 2).
Table 3 summarizes the three QEESI scales. The most affected systems in the severity of symptoms scale are the dermatological, gastrointestinal, musculoskeletal and neurological systems. The products that induced intolerance were insecticides, bleach, household cleaners, perfumes, and air fresheners. The most affected life-style areas were maintaining daily personal hygiene, household cleaning, and work or study.
Description of Clinical Data: Suffering
The mean score for suffering was 53.7 (SD = 20.6). The three dimensions of suffering (physical, psychological, and existential) for the overall study sample (sum of the 3 dimension scores) and for moderate vs. severe MCS subgroups are summarized in Table 4. The maximum possible score was 30 on the physical suffering scale, 45 on the psychological scale, and 36 on the existential scale. Because of the differences in scoring of the three dimensions, we expressed the sum of the scores as an overall percentage so as to improve comparisons. In general, the physical sphere of suffering was the most affected in the overall study sample, as well as in the two severity subgroups. This was followed by the psychological sphere and, finally, the existential dimension. All scores were higher in the severe disease category than in the moderate disease subgroup.
Table 5 summarizes the responses to the different scales of suffering. Of note was that in the physical dimension of suffering, musculoskeletal and respiratory problems were those that produced more discomfort, whereas in the psychological dimension the feelings that produced more discomfort were worry or anxiety and lack of gaiety. In the existential area, thoughts of lack of inner harmony and a sense of failure in life were the most intense.
Associations between Study Variables
Table 6 highlights the correlations (Pearson's r coefficients) between the QEESI scales and the 3 dimensions of suffering, and between the total scores of the QEESI variables and suffering. There was a high positive correlation between severity scales, impact on life-style, and all measures of suffering. The Intolerance scale did not segregate with suffering (low r coefficient).
A linear regression analysis with the three subscales of QEESI as predicting variables and suffering as the dependent variable (see Table 7) showed that the equation was statistically significant (F = 24.720, p < .001) and explained 38.2% of the variance in the total score of suffering (R2 = .382) and with significance in the three measured variables: severity of illness (B = 0.581), chemical intolerances (B = -0.270) and life impact (B = 0.334).
Discussion
The current study provides the initial approach to suffering in people diagnosed with MCS. In Spain, it is a poorly documented disease among the general population and among health-care professionals as well. This had prompted us to evaluate in detail the clinical and socio-demographic characteristics of participants, their suffering and the associated factors. Our findings are similar with respect to gender, age and comorbidity to those found by Nogué et al. (2007) with, in our study, a slightly higher percentage of those with permanent disability and years of disease evolution.
According to the QEESI scores, there were high levels of disease on the three scales, with mean scores significantly higher than cutoff points recommended by Miller and Prihoda (1999). The scores in the Nogué et al.'s study (2007) were similar in severity and intolerance scales, but considerably higher, in our study, on the life impact scale (80.86 vs. 66.6)
The comparison of our data with those obtained by Nogué et al. in 2007 suggests: 1) an increase in years-of-evolution of the disease; 2) an increase in work disability; and 3) an increase in the impact on daily-life activities. These results could indicate that the evolution of the disease is conducive to greater disability. However, our study showed no differences in severity in relation to years-of-evolution of the disease.
We observed, in relation to suffering, that the most affected dimension of suffering was the physical with respect to severe and moderate levels of disease, followed by the psychological and, finally, the existential dimension. Apart from the suffering inherent in the physical problems, the disease causes the individual considerable worry or anxiety, sadness, fear, and feelings of lack of purpose in their lives. These symptoms are often aggravated as the disease progresses, or the longer the disease remains untreated.
The high correlations between disease and different dimensions of suffering have, however, an exception in the case of inhalation intolerances scale. Here the correlations with all dimensions of suffering are weak, even being reversed in the case of existential suffering. These results could be explained by the Threat and Resources Model (Bayés et al., 1996), according to which the patients would be evaluating symptoms and the limitations they pose on their daily lives because they did not have enough resources to cope with the symptom-provoking event. However, the chemicals to which they are intolerant, although being the cause of discomfort, can be avoided in some cases and, as such, the threat is reduced. The disease has a variable course in which it is possible to reduce the symptoms if living in a toxin-free environment. However, opting for a toxin-free environment poses other problems such as social wellbeing and employment opportunities (Gibson et al., 2011) and, hence, a balance needs to be stuck by the individual between all these competing areas of a person's lifestyle.
Apart from the analysis of intolerance scale described above, of considerable note was the negative correlation between intolerance and existential suffering. This inverse trend could be indicative of a greater adjustment to the illness, i.e., the more serious the intolerances the greater the individual's need to avoid such threatening substances and a better adjustment to the disease. This is concordant with the findings of Nordin et al. (2010) who showed that the avoidance strategy is the most effective way of coping with the problem.
Although the correlations between severity of disease and dimensions of suffering are significant, these associations are less strong in existential suffering. One explanation could be that the causes of this weaker association is that in moderate degree of disease when physical limitations and everyday life limitations are few, the expectation of future limitations and breaking-off of vital projects could imply a loss that affects the existential sphere.
Our study has some limitations that need to be considered in future investigations. Firstly, given that there are no normative data in this population, there is considerable difficulty in comparing and interpreting the scores on suffering. Our study population did not contain individuals with the mild form of the disease. This was probably due to the fact that only those individuals with moderate-to-severe disease were affected enough to contact the webpage and/or that the ones with mild disease had not as yet been diagnosed with MCS. A further limitation is that although we evaluated the physical, psychological, and existential aspects of the suffering, one real consequence of the disease is severe isolation, the social trauma of which we were unable to explore in the current study.
Knowing the causes of an individual's suffering is essential when addressing possible solutions. In this respect, our study provides a comprehensive quantitative assessment of suffering in individuals with MCS. As for other ambiguous chronic illnesses (Johnson & Johnson, 2006), such knowledge will help health-care providers to identify and diagnose the symptoms since the organic causes for the symptoms are not easy to identify. Further, our data provide a basis for specific future therapies, with the hope of reducing the suffering.
Conclusions
MCS is a disease that causes physical, psychological, and existential suffering. The severity of symptoms generates the most suffering, followed by QoL constraints, while the number and severity of inhalation intolerances decrease overall suffering. Musculoskeletal and respiratory problems cause the most physical suffering. Psychological suffering is marked by worry or anxiety and joylessness. Existential suffering reveals thoughts of failure and lack of inner harmony.
Relevance to Clinical Practice
This study provides a detailed description of MCS and the consequences that the disease has on the individual. This knowledge can provide the bases for future therapies. Given the current lack of knowledge of the disease on the part of health-care professionals, and the consequent lack of attention of these patients, the findings may help sensitize health-care workers to this problem, which can only increase with progressively increasing industrial and domestic pollutants.
Conflict of interest
The authors of this article declare no conflict of interest.
Acknowledgements
We gratefully acknowledge María José Moya Villén for her excellent collaboration and diffusion of the project's intent and purpose via her webpage (http://mi-estrella-de-mar.blogspot.com/). We also thank all the individual participants for their enthusiastic support in the survey.
Appendices
Manuscript received: 25/11/2013
Revision received: 27/02/2014
Accepted: 21/04/2014
Doi: http://dx.doi.org/10.1016/j.clysa.2014.06.006
*Correspondence concerning this article should be addressed to
Rosa García-Sierra. Consorci Sanitari de Terrassa.
Carretera Torrebonica s/n. 08227 Terrassa (Barcelona), Spain.
E-mail: rgarcias@cst.cat
References
Arnold, P., Climent, B., Fernández-Solà, J., López, F., Maestu, C., Márquez, J., ... Lois, M. (2011). Informe de consenso 2011. Ministerio de Sanidad. Gobierno de España. Nota de prensa del 30 de noviembre de 2011. Retrieved from http://www.mspsi.gob.es/organizacion/sns/ planCalidadSNS/pdf/equidad/SQM_documento_de_consenso_30nov2011.pdf
Bayés, R., Arranz, P., Barbero, J., & Barreto, P. (1997). Propuesta de un modelo integral para una intervención terapéutica paliativa. Medicina paliativa, 3, 114-121.
Bartha, L., Baumzweiger, W., Buscher, D. S., Callender, T., Dahl, K. A., Davidoff, A., ... Ziem, G. (1999). Multiple chemical sensitivity: a 1999 consensus. Archives of Environmental Health, 54, 147-149.
Cassell, E. J. (1982). The nature of suffering and the goals of medicine. New England Journal of Medicine,306, 639-645.
Cullen, M. R. (1987). The worker with multiple chemical sensitivities: an overview. Occupational Medicine2, 655-661.
Chapman, C. R., & Gravin, J. (1993). Suffering and its relationship to pain. Journal of Palliative Care,9, 5-13.
Fox, R. A. Joffres, M. R., Sampalli, T., & Cas, J. (2007). The Impact of a Multidisciplinary. Holistic Approach to Management of Patients Diagnosed with Multiple Chemical Sensitivity on Health Care Utilization Costs: An Observational Study. The journal of alternative and complementary medicine,13, 223-229.
Gibson, P. R., & Vogel, V. M. (2009). Sickness related dysfunction in persons with self reported multiple chemical sensitivity at four levels of severity. Journal of Clinical Nursing, 18, 72-81.
Gibson, P. R., Sledd, L. G., McEnroe, W. H., & Vos, A. P. (2011). Isolation and lack of access in multiple chemical sensitivity: A qualitative study. Nursing and Health Sciences,13, 232-237.
Johnson, J. E., & Johnson, K. E. (2006). Ambiguous Chronic Illness in Womwn: A Community Health Nursing Concern. Journal of Community Heatlh Nursing, 23, 159-167.
Krikorian, A., & Limonero, J. T. (2012). An integrated view of suffering in palliative care. Journal of Palliative Care, 28, 41-9.
Koch, L., Vierstra, C., & Penix, K. (2006). A qualitative investigation of the psychosocial impact of multiple chemical sensitivity. Journal of Applied Rehabilitation Counseling, 37, 33-40.
Labarge, X. S., & McCaffrey, R. J. (2000). Multiple chemical sensitivity: a review of the theoretical and research literature. Neuropsychology Review,10, 183-211.
Lacour, M., Zunder, T., Schmidtke, K., Vaith, P., & Scheidt, C. (2005). Multiple chemical sensitivity syndrome (MCS) - suggestions for an extension of the US MCS-case definition. International Journal of Hygiene and Environmental Health,208, 141-151.
Miller, C. S., & Prihoda, T. J. (1999).The Environmental Exposure and Sensitivity Inventory (ESSI): a standardized approach for measuring chemical intolerances for research and clinical applications. Toxicology and Industrial Health,15, 370-385. Nethercott, J. R., Davidoff, L. L., Curbow, B., & Abbey, H. (1993).
Multiple chemical sensitivities syndrome: toward a working case definition. Archives of Environmental Health,48, 19-26.
Nogué, S., Fernández-Solà, J., Rovira, E., Montori, E., Fernández-Huerta, J. M., & Munné, P. (2007). Sensibilidad Química Múltiple: análisis de 52 casos. Medicina Clínica, 129(3), 96-99.
Nordin, M., Andersson, L., & Nordin, S. (2010). Coping strategies. social support and responsibility in chemical Intolerance. Journal of Clinical Nursing,19, 2162-2173.
Ortega, A. (2005). Sensibilidad a múltiples compuestos, una enfermedad comúnmente inadvertida. Medicina Clínica, 125, 257-262.
Randolph, T. (1954). Allergic-type reactions to industrial solvents and liquid fuels; mosquito abatement fogs and mists; motor exhaust; indoor utility gas and oil fumes; chemical additives of food and drugs; and synthetic drugs and cosmetics. Journal of Laboratory and Clinical Medicine, 44, 910-922.
Schulz, R., Monin, J. K., Czaja, S. J., Lingler, J. H., Beach, S. R., Lynn, M., ... Cook, T. B. (2010). Measuring the Experience and Perception of Suffering. The Gerontologist,508, 774-784.
Skovbjerg, S., Brorson, S., Rasmussen, A., Johansen, J. D., & Elberling, J. (2009). Impact of self-reported multiple chemical sensitivity on everyday life-a qualitative study. Scandinavian Journal of Public Health,37, 621-626.