El objeto del estudio es determinar si las variables ansiedad-estado, ansiedad-rasgo, afecto positivo, afecto negativo, alexitimia y recursos adaptativos (personales e interpersonales) pueden predecir el desajuste emocional en personas infértiles, analizando el posible papel modulador del sexo en dicho desajuste. Participaron en el estudio 101 personas con un diagnóstico de infertilidad (51 hombres y 50 mujeres) que respondieron a una batería de pruebas psicológicas (DERA, Cuestionario de Desajuste Emocional y Recursos Adaptativos en Infertilidad, Inventario de Ansiedad Estado-Rasgo [STAI], PANAS, Escala de Afectos Positivos y Negativos y TAS-20 [Escala de Alexitimia de Toronto]). Los efectos moduladores, parciales y de interacción de las variables se analizaron mediante un análisis de regresión de orden jerárquico. El modelo resultante explica el 71.1% de la varianza total, constituyendo el sexo una importante variable moduladora, mientras las variables ansiedad-rasgo, ansiedad-estado, afecto negativo y bajos recursos interpersonales actúan como importantes predictores del desajuste emocional en personas infértiles. Los resultados pueden ayudar en la elección de apoyos y tratamientos psicológicos y adecuados para alcanzar el ajuste emocional en hombres y mujeres infértiles.
The objective of this study is to find out if the variables state-anxiety, trait-anxiety, positive-affect, negative-affect, alexithymia, and adaptive (personal and interpersonal) resources can predict emotional maladjustment in infertile people, taking into account the potentially moderating role of gender. A sample of 101 participants with an infertility diagnosis (51 males and 50 females) completed a battery of psychological tests (DERA, Emotional Maladjustment and Adaptive Resources in Infertility questionnaire, State-Trait Anxiety Inventory [STAI], PANAS, Positive and Negative Affect Schedule, and TAS-20, [Toronto Alexithymia Scale]). The moderating, partial, and interactive effects of the variables were analyzed using hierarchical regression analysis. The resulting model explained 71.1% of total variance, resulting in gender as an important moderating variable and trait anxiety, state anxiety, negative affect, and low interpersonal resources as strong predictors of emotional maladjustment in infertile people. These results provide guidance in selecting the most appropriate psychological support and treatment for the emotional adjustment of infertile women and men.
The World Health Organization considers infertility, the inability of a couple to conceive children, a chronic disease. This disease does not usually manifest physical symptoms. Generally, it is detected after several months of regular intercourse without achieving pregnancy.
A year of failed attempts is the criterion for requesting diagnostic tests, but most couples come to assisted reproduction units after trying much longer and so the interval is considered by Moreno-Rosset, Antequera, Jenaro, and Gómez (2009) as a stressful life event that makes infertility an anxious process that increases as months pass without achieving the desired child and which affects different areas (social, work, family, etc.) of women, men, and couples.
Medicine and Reproductive Biology have focused on developing assisted reproductive technology (ART) to achieve pregnancy in infertile people. Louise Joy Brown was the first person born in the UK through IVF in 1978. In Spain, Victoria Anna was the first in 1984 and during this period investigation focused on the physiological and biological aspects of people who could not achieve pregnancy by natural means.
Later, together with the medical aspects, infertility has been studied by Reproductive Psychology, which evaluates and treats the emotional pain caused by this disease without physical symptoms but with clear signs such as the appearance of menstruation as an indication of no pregnancy. All processes related to the reproductive cycle, although natural, can lead to significant emotional alterations such as PMS or postpartum depression, among others. As indicated by Nereu, Neves, and Casado (2013), the stages a pregnant woman passes through constitute a kind of emotional ‘merry go round”, but when she does not become pregnant the suffering increases, turning into a “roller coaster”. Perhaps for these reasons the International Federation of Gynecology and Obstetrics (FIGO) defines infertility as the “disease” that afflicts people who do not get pregnant after a year of regular sexual relations.
Looking back on the psychological study of infertility, we see an evolution of the focus of interest coupled to the models and psychological schools that have developed. So, the psychological causes of infertility have been sought from psychoanalytic approaches in the beginning (Feder, 1980; Goldschmidt & Jürgensen, 1985). Later, the perspective widens, analyzing the effects and consequences that infertility and assisted reproduction treatments cause (Eugster & Vingerhoets, 1999). Furthermore, not taking men into account has been criticized since most studies initially focused on women as females undergo the most painful part of the ART treatments (Greil, 1997). This author in his literature review also highlights the need to apply methodology and assessment tools that are suitable and specific to the field.
Classically, the main variables studied have been anxiety and depression without finding conclusive results in many cases (Verhaak et al., 2007). Antequera, Moreno-Rosset, Jenaro, & Ávila-Espada (2008) provide a review of emotional changes before an infertility diagnosis, during treatment, and during pregnancy and parenting, highlighting the need to differentiate between emotional maladjustment and psychopathological alteration in infertile people in order to detect those couples that are vulnerable to developing psychopathology.
The new approaches on health and prevention investigate variables such as distress or emotional discomfort as well as emotional imbalance, which, not being clinical measures, become psychopathology risk indicators for people undergoing stressful processes. This is true in chronic diseases such as cancer, in which emotional distress has been studied (Hernández & Cruzado, 2013) or in infertility that, although not affecting individuals’ survival, shows parallelism with the processes of cancer patients. One third of infertile people studied by Van Dongen, Kremer, Van Sluisveld, Verhaak, and Nelen (2012) are at risk of emotional maladjustment before the start of ART treatments. El Kissi et al. (2014) found greater emotional mal-adjustment, emotional disturbances, and worse quality of life in infertile couples compared to general population. Also, variables such as coping strategies and alexithymia were analyzed with an interest in their relationship with the emotional distress experienced in infertility (Phillips, Elander, & Montague, 2014; Shi, Wu, & Zhu, 2006).
Another perspective on the rise more recently is Positive Psychology, which proposes wellbeing, strengths, and resource variables to help manage the psychological distress. How positive and negative affects interact with biological variables such as the number of transferred oocytes and term pregnancies has been studied, as well as stress and anxiety (Coughlan, Walters & Ledger, 2014; Mahajan et al., 2010; Schalet, Cook, Choi, & Cella, 2014). Resilience and post-traumatic growth, suggesting that there is a strengthening of the welfare of the couple and the individual by overcoming the difficulty faced by infertile couples, have also been studied (Hermann et al., 2011; Yu et al., 2014).
In short, a significant evolution in the study of psychological factors in infertility can be seen. In addition to the evaluation of the clinical aspects, such as anxiety and depression, the protective variables of couple wellbeing were added and hence the present study can be considered part of a holistic view of the emotional health of infertility that includes clinical and non-clinical variables, with the aim of detecting prodromal symptoms to alert of possible subsequent psychopathological problems.
The aim of this study was to determine whether state-anxiety, trait-anxiety, positive-affect, negative-affect, alexithymia, and adaptive (personal and interpersonal) resources can predict emotional maladjustment in infertile people. In addition, gender is analyzed as a possible moderating effect on the analysis of the prediction.
Method
Participants
The sample consisted of 101 participants with infertility problems, 51 males and 50 females, who attended a private assisted reproduction unit in Zaragoza, Spain, asking for assisted reproduction treatment. One female participant was not included in the study due to a mistake when completing the questionnaire. The mean age for the male group is 35.88 years (SD = 4.37), minimum 27 and maximum 47, and the mean age for the female group is 34.42 (SD = 4.37), minimum 25 and maximum 44. Both groups are homogeneous in terms of educational level (χ2 = 1.719, p = .787). All participants were required: a) to be legally married or living with a partner in a heterosexual relationship; b) be over 18; c) be intelligent enough to understand the questionnaires; and d) have no major medical or psychological problems.
Procedure
Infertile couples who consulted the Assisted Reproduction Unit for treatment of their infertility were informed about the research and asked to collaborate in it. The couples that agreed to participate signed the corresponding consent form and became part of the study’s sample group. In general terms, people invited to participate voluntarily did so. Only those couples who had time problems turned down the offer. The selection of the sample was carried out over six months. The instruments for psychological assessment were individually completed by each member of the couple in the clinic. This procedure (in situ and each one independently) avoided any possible assessment bias. The study had been previously approved by the Healthcare Ethics Committee of the Center for Assisted Reproduction.
Measures
Participants were assessed by means of the following instruments:
– Emotional Maladjustment and Adaptive Resources in infertility questionnaire (DERA; Moreno-Rosset, Antequera, & Jenaro, 2008). This instrument consists of 48 elements with a five-point Likert type response format that asks the extent to which the subject agrees with each of the statements presented. It consists of four factors: emotional maladjustment, personal resources, interpersonal resources, and adaptive resources. Cronbach’s alpha coefficient is .85 for the global scale and .90, .57, .78 and .74. respectively for the individual scales. The validity studies convergent with the questionnaire on ways of coping with stressful events (CEA; Rodríguez-Martín, Terol, López-Roig, & Pastor, 1992) give evidence of the validity of the instrument. Other psychometric data can be found in the study by Moreno-Rosset, Antequera, and Jenaro (2009).
– Positive and Negative Affect Schedule (PANAS; Watson, Clark, & Tellegen, 1988), Spanish adaptation by Sandín et al., (1999). This scale consists of 20 items. It measures affect in two independent non-correlated dimensions. The positive affect reflects the extent to which someone feels enthusiastic, active, alert, energetic, and with pleasant participation. The negative affect shows a general dimension of subjective ill-being and unpleasant participation, including a variety of aversive emotional states, such as annoyance, anger, blame, fear, and nervousness. Cronbach’s alpha coefficients for the Spanish version used in this study are .89 for the positive affect scale and .91 for the negative affect scale for males and .87 for the positive affect scale and .89 for the negative affect scale for females (Sandín et al., 1999).
– State-Trait Anxiety Inventory (STAI; Spielberger, Gorsuch, & Lushene, 1970), Spanish version by TEA (2008). It consists of two scales, state anxiety and trait anxiety, with 40 items, 20 items for each scale describing respectively – how the subject feels at a given moment and how they feel generally. The Spanish version of this scale presents indices of internal consistency for the state-anxiety scale of between .90 and .93 and for the trait-anxiety scale of between .84 and .87. Reliability values calculated by the two halves method reach a value of .94 in state anxiety and .86 in trait anxiety.
– Toronto Alexithymia Scale (TAS-20; Bagby, Parker, & Taylor, 1994), Spanish adaptation by Martínez-Sánchez (1996). The TAS-20 is a 20-item self-report measure, which measures the degree of alexithymia. It consists of three factors: difficulty identifying feelings and distinguishing physiological sensations that accompany emotional arousal, difficulty describing feelings and pattern of externally oriented thinking. This adaptation has an internal consistency of .78 and a test-retest reliability of .71. Of the various techniques used for the assessment of alexithymia, the TAS-20 is the most frequently used because its outstanding psychometric properties (Bagby, Taylor & Parker 1994; Martínez-Sánchez & Ortiz, 2000). The stability and replicability of the factorial structure has been confirmed in both clinical and non-clinical samples.
Data Analysis
First, descriptive analysis and t-test analysis for independent samples were performed to observe possible differences in study variables between men and women. Analysis of correlations between emotional maladjustment and the remaining variables using the Pearson’s correlation coefficient were also carried out.
Finally, partial and interactive effects of the variables were analyzed using a multiple regression analysis with hierarchical order of inclusion. The model was analyzed using participants’ gender as potentially moderating variable in step 1. The main predictors of emotional maladjustment (state-anxiety, trait-anxiety, positive-affect, negative-affect, alexithymia, personal resources, interpersonal resources, and adaptive resources) were included in step 2. Interactions between gender and the main predictor variables were analyzed in step 3.
Statistical significance was set at a confidence interval of 95% and p < .05 as the criterion. Analyses were performed using SPSS v. 19 for Windows.
Results
Previous Analysis
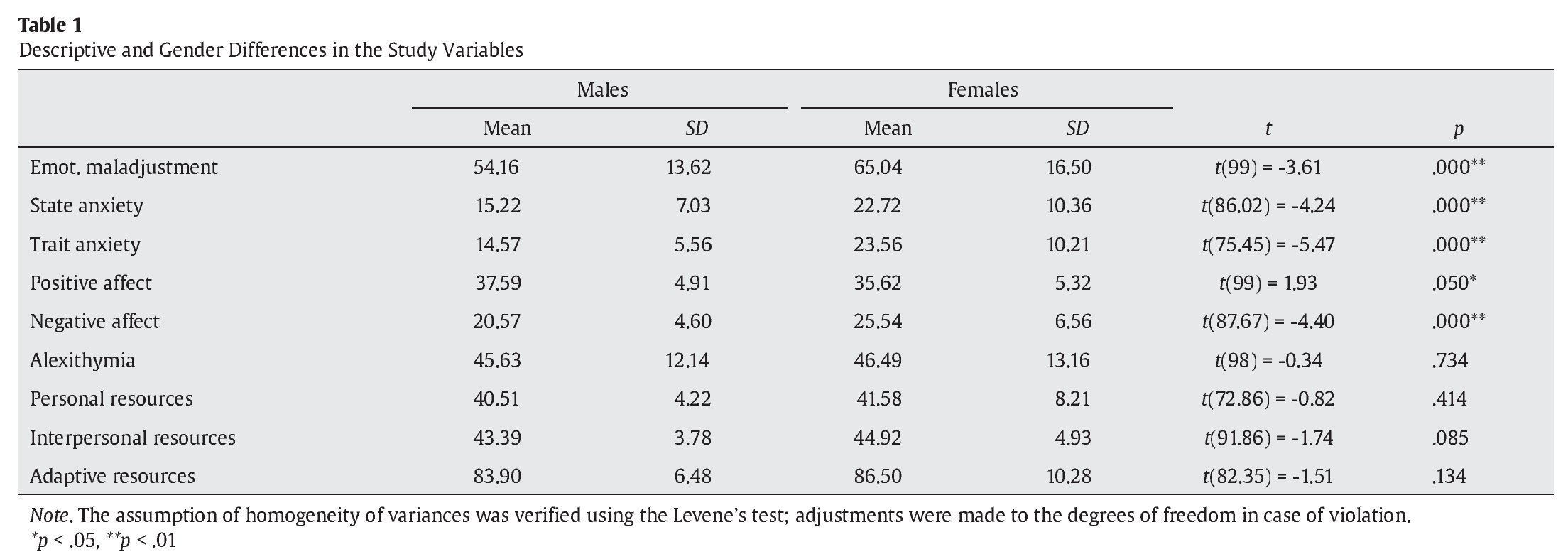
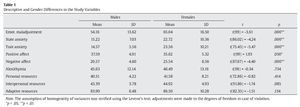
Table 1 shows the means and standard deviations of the study variables. It can be seen that women tend to have higher scores on all variables except for positive-affect, where men scored higher. These differences are significant in the case of the variables emotional maladjustment, t(99) = -3.617, p = .000, state anxiety, t(86.02) = -4.249, p = .000, trait anxiety, t(75.45) = -5.479, p = .000, negative affect, t(87.67) = -4.402, p = .000, and positive affect, t(99) = 1.931, p = .050.
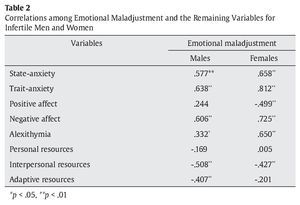
With the aim to explore the relationship between the emotional maladjustment variable and the other variables, two correlation analysis based on participants’ gender were performed. The results are shown in Table 2.
For men, there are significant positive correlations between emotional maladjustment and state anxiety (.577, p = .000), trait anxiety (.638, p = .000), negative affect (.606, p =.000) and alexithymia (.332, p = .017) and significant negative correlations between emotional maladjustment and interpersonal resources (-.508, p = .000) and adaptive resources (-.407, p = .000). As for women, significant positive correlations were found between emotional maladjustment and state anxiety (.658, p = .000), trait anxiety (.812, p = .000), negative affect (.725, p = .000), and alexithymia (.650, p = .000) and significant negative correlations between emotional maladjustment and positive affect (-.499, p = .000) and interpersonal resources (-.427, p = .002).
Predictive Analysis: Moderating, Partial and Conditioned Effects
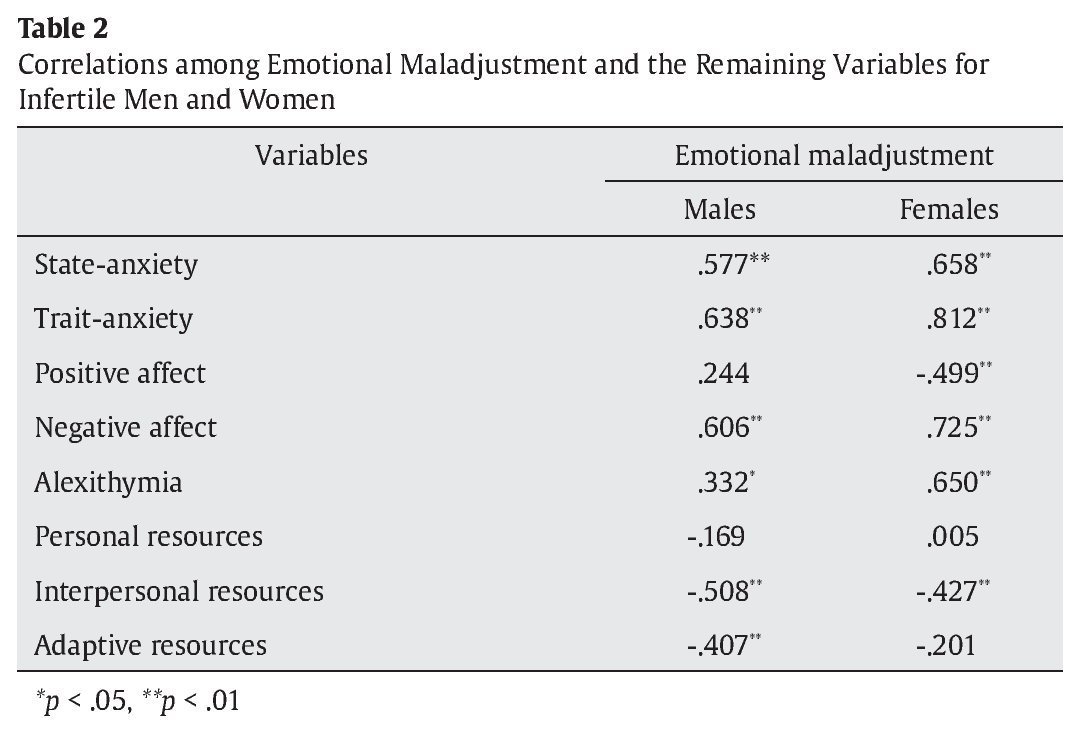
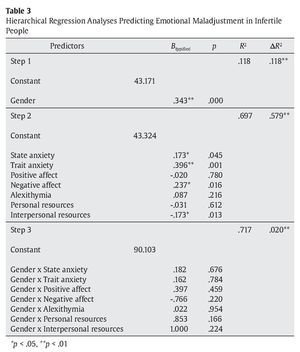
Partial and interactive effects of the variables were analyzed using a multiple regression analysis with hierarchical order of inclusion. The model was analyzed using participants’ gender as a potentially modulating variable in step 1. The main predictors of emotional maladjustment were included in step 2 and interactions between gender and the main variable predictors were analyzed in step 3. This model explained 71.7% of the variance in psychological maladjustment in infertile people.
As shown in Table 3, step 1 indicates a significant effect of the variable gender (β = .343, p = .000). This moderating variable explained 11.8% of the variance in emotional maladjustment in infertile people.
Results in step 2 show that state anxiety (β = .173, p = .045), trait anxiety (β = .396, p = .000), negative affect (β = .237, p = .016), and interpersonal resources (β= -.173, p = .013) all contributed significantly to emotional maladjustment. Collectively, these variables explained an additional 57.9% of the variance in emotional maladjustment in infertile people. Finally, results of analyses in step 3 indicate that the interactions between gender and predictor variables increase the overall variance explained by the model by 2%. However, there is no significant concrete interaction effect.
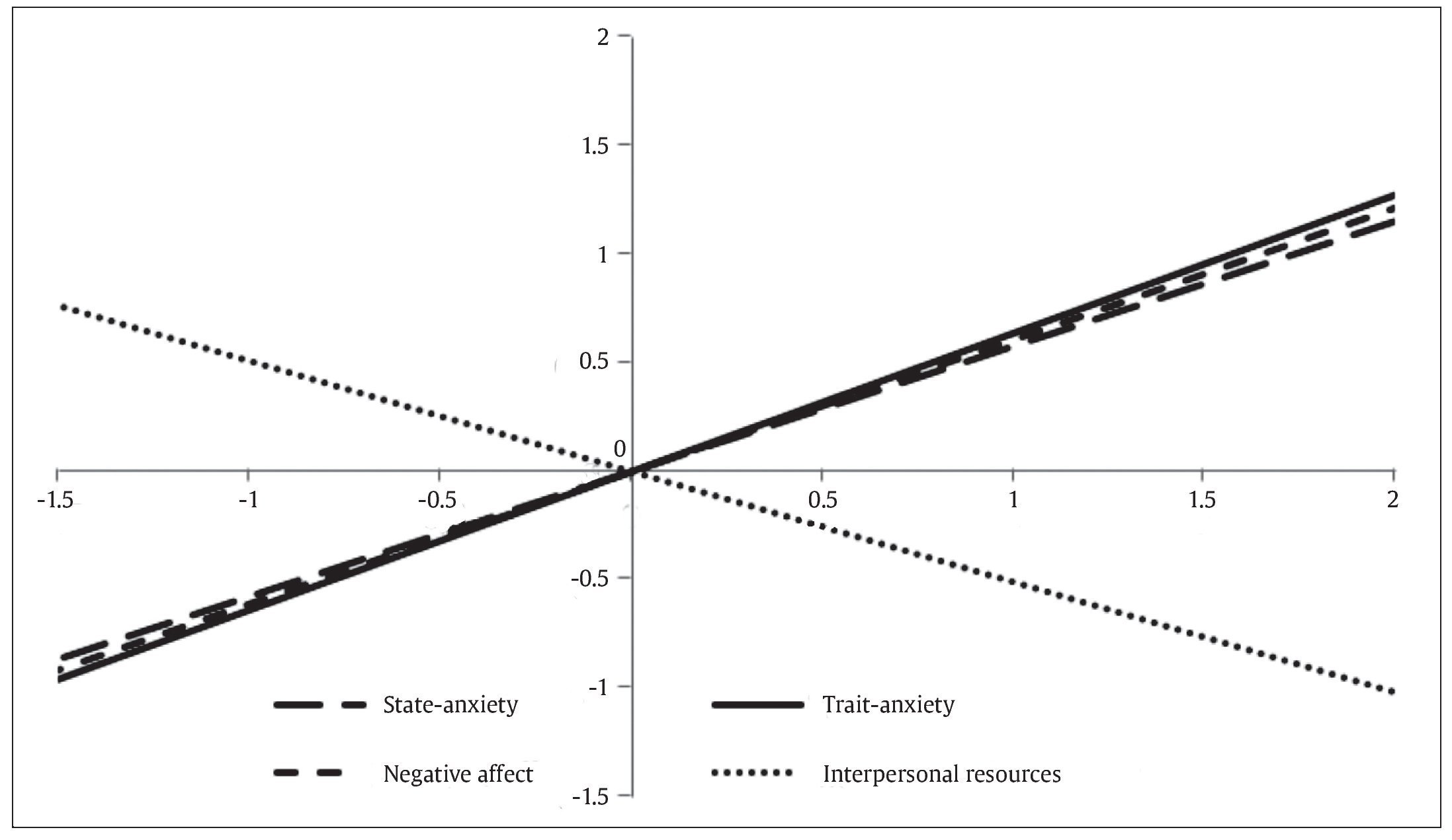
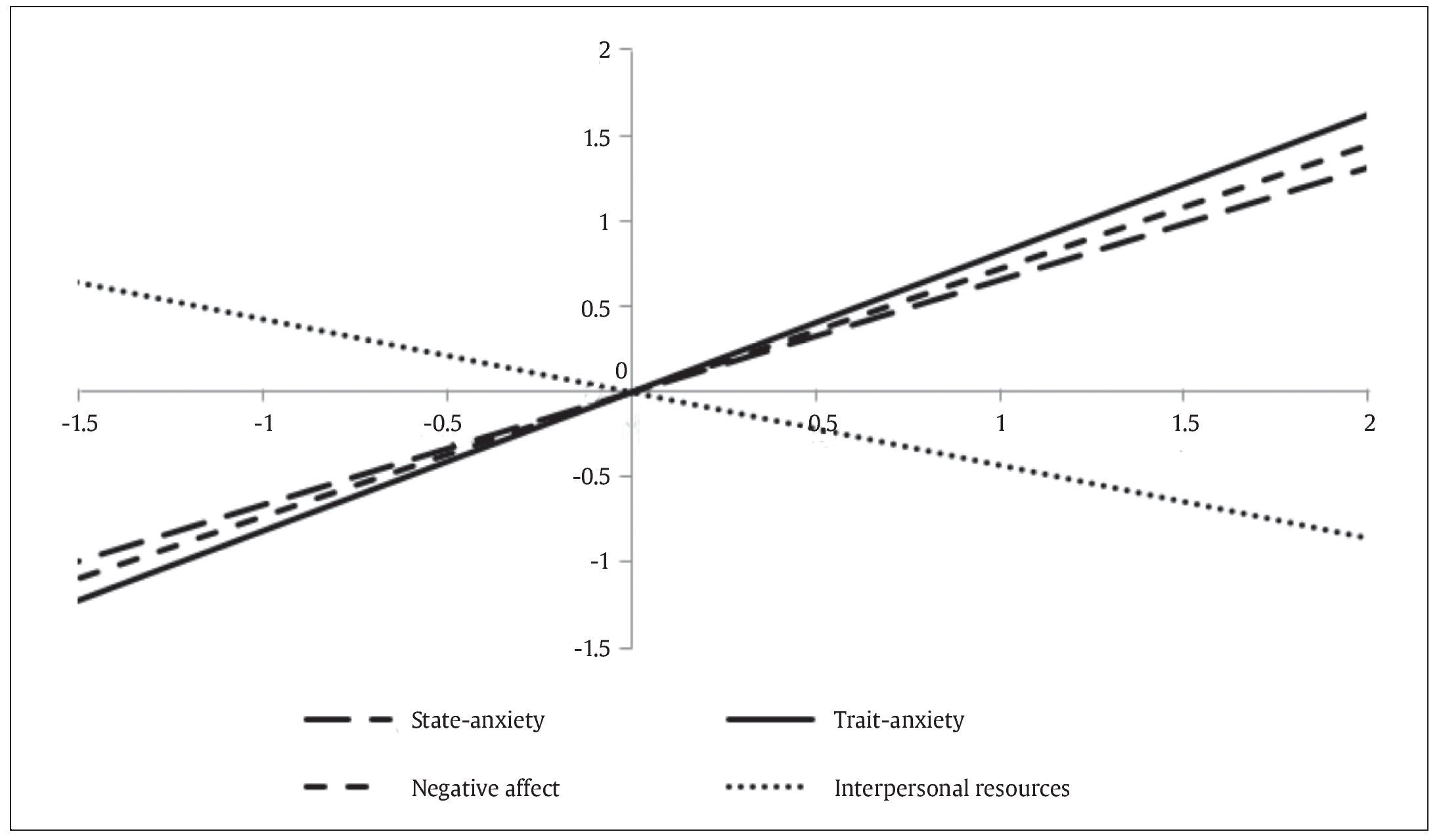
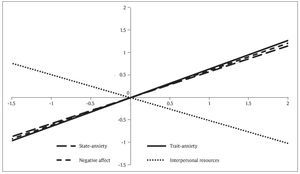
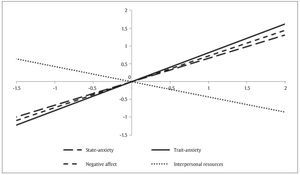
Figures 1 and 2 graphically show the results of the hierarchical regression analysis predicting emotional maladjustment from typical scores obtained from the variables trait anxiety, state anxiety, negative affect, and interpersonal resources for infertile men and women, respectively.
Figure 1. Prediction of Emotional Maladjustment from Typical Scores Obtained for the Predictor Variables (infertile males).
Figure 2. Prediction of Emotional Maladjustment from Typical Scores Obtained for the Predictor Variables (infertile females).
Discussion
In previous work we have found that infertile women in the study sample had a higher level of emotional maladjustment and negative affect, while men had higher positive affect (Del Castillo, Moreno-Rosset, Martín, & Ramírez-Uclés, 2009). We also found that women experience higher levels of state and trait anxiety (Moreno-Rosset, Del Castillo, Ramírez-Uclés, & Martín, 2011). In this paper we propose to establish a predictive model of emotional maladjustment in infertility and know the potentially moderating role of gender in order to help design support and psychological interventions targeting women and men at first contact with Assisted Human Reproduction Units.
The results obtained from regression analysis lead us to conclude that gender acts as a moderating variable with partial effects from trait anxiety, to a larger extent, followed by negative affect, state anxiety and low interpersonal resources in explaining emotional mal-adjustment in infertile people.
The moderating effect of the variable gender suggests that infertile women have higher risk of emotional maladjustment. Therefore, being a female can predispose to suffer emotional maladjustment, which is in agreement with studies such as Huppelschoten et al. (2013) that found that 63.8% of infertile females and 45.6% of infertile males had, at least, one risk factor for developing emotional mal-adjustment. It is no coincidence that most infertility literature is focused on women, since they are who receive medical treatment and are most likely to develop emotional disorders during assisted reproduction treatment (Chiaffarino et al., 2011; Culley, Hudson, & Lohan, 2013).
Regarding the psychological variables evaluated, trait anxiety has a greater predictor effect. Psychological factors, such as trait-anxiety and depression, have proved to be predictors of quality of life in chronic diseases such as diabetes mellitus type 1 (Machado, Anarte, & Ruiz de Adana, 2010), so it is shown that people with chronic levels of activation are emotionally vulnerable when faced with diseases that compromise physical and reproductive health, especially in infertile women.
In the analyzed regression model it can be seen how negative affect and state-anxiety are also actively involved in predicting emotional maladjustment in the early stages of diagnosis and treatment of infertility. Thus, emotions that make up negative affect such as anger, guilt, fear, and nervousness, may be a risk factor for emotional maladjustment if the most suitable care and management are not received. Similar results are reported by Pápay, Rigó, and Nagybányai (2013) who, in a multiple regression analysis, found that it is negative affect and avoidant coping which positively predict the distress or emotional discomfort associated with infertility.
Also, note that low interpersonal resources predict emotional maladjustment in this study’s sample, a fact in agreement with abundant literature in different areas of health and that also support its protective effect (Barrón, 1996; Östberg & Lennartsson, 2007). In the case of infertility, the couple may be the first and closest social support, as reflected in marital satisfaction (Darwiche et al., 2013), although it is important that it is not the only interpersonal resource. Mahajan et al. (2009) found that interpersonal resources accounted for 28.4% of the variance of the adjustment to infertility, satisfaction of the couple being among them.
As for the variable alexithymia, despite maintaining a clear positive correlation with emotional maladjustment, it is not predictive as it is the maladjustment itself that triggers the alexithymia found in infertility (Conrad, Schilling, Langenbuch, Haidl, & Liedtke, 2001; Shi et al., 2006). In fact, alexithymia is proposed as a defense for suffering, which at first can reduce it while ultimately creating different psychosomatic problems due to the failure to resolve the denied problem (Berry & Pennenbaker, 1993; Lumley, Neely, & Burger, 2007).
It can even reduce the chances of getting pregnant because of the physiological responses produced by repression and denial of emotional stress (de Klerket al., 2008).
Conclusions
We can conclude that it will be important to assess the emotional maladjustment at first contact with Assisted Human Reproduction Units, in order to prevent treat trait anxiety, state anxiety, and negative affect as well as to enhance interpersonal resources, especially in women.
In relation to gender, the predictor difference should not exclude the masculine facet from research. Infertility is about couples and the man can be a potential in the couple, representing an invaluable interpersonal resource for the women (Del Castillo, Arnal, Moreno-Rosset, Ramírez-Uclés, & Urries, 2014). In this line, Pápay et al. (2013) found that satisfaction and partner communication predict negative distress or psychological distress associated with infertility.
Thus, family and social relationships, in addition to the dampening effect of emotional distress (Lechner, Bolman, & Van Dalen, 2007), provide us space to refresh ourselves, to leave behind the issue that concerns us and to contact more positive emotions. Greenglass and Fiksenbaum (2009) note the existence of a relationship between social support, positive affect, and a high level of wellbeing.
As a limitation of this study, we note the size of the sample and that further research with a larger sample of women and men is necessary to allow us to continue investigating on the prediction of emotional maladjustment in infertility and the moderating effect of gender. The challenge is not to improve emotional adjustment in all patients with fertility problems but to identify in advance who is at risk of developing serious emotional maladjustment and to offer treatment tailored to their individual vulnerabilities (Verhaak, Lintsen, Evers, & Braat, 2010).
The need for the important role played by a psychologist has been recognized in Assisted Reproduction Units (Moreno-Rosset, Antequera, Jenaro, & Gómez, 2009). A proper psychological assessment allowing early detection of people at emotional risk will allow the treatment of anxiety and negative affect associated with infertility. Likewise, the support of loved ones and especially the partner will ease emotional adjustment in infertility.
Conflict of Interest
The authors of this article declare no conflict of interest.
Financial Support
This article was funded as part of the actions to aid the dissemination of the UNED Research Promotion Plan.
Manuscript received: 28/11/2014
Revision received: 23/12/2014
Accepted: 13/01/2015
Doi: http://dx.doi.org/10.1016/j.clysa.2015.01.002
*Correspondence concerning this article should be sent to
Isabel M. Ramírez Uclés.
Departamento de Personalidad, Evaluación y Tratamiento Psicológico.
Universidad Nacional de Educación a Distancia (UNED).
C/ Juan del Rosal, 10.
28040-MADRID.
E-mail: iramirez@psi.uned.es
References
Antequera-Jurado, R., Moreno-Rosset, C., Jenaro, C., & Ávila-Espada, A. (2008). Principal Psychological Disorders associated with infertility. Papeles del Psicólogo, 2, 167-175. Retrieved from http://www.papelesdelpsicologo.es/english/1583.pdf
Bagby, R. M., Parker, J. D. A., & Taylor, G. J. (1994).The twenty-item Toronto Alexithymia Scale-I. Item selection and cross-validation of the factor structure. Journal of Psychosomatic Research, 38, 23-32.
Bagby, R. M., Taylor, G. J., & Parker, J. D. A. (1994). The twenty-item Toronto Alexithymia Scale-II. Convergent, discriminant, and concurrent validity. Journal of Psychosomatic Research, 38, 33-40.
Barrón, A. (1996). Apoyo Social: aspectos teóricos y aplicaciones [Social support: theoretical aspects and applications]. Madrid: Siglo XXI.
Berry, D. S., & Pennebaker, J. W. (1993). Nonverbal and verbal emotional expression and health. Psychotherapy and psychosomatics, 59, 11-19.
Chiaffarino, F., Baldini, M. P., Scarduelli, C., Bommarito, F., Ambrosio, S., D’Orsi, C., … Ragni, G. (2011). Prevalence and incidence of depressive and anxious symptoms in
couples undergoing assisted reproductive treatment in an Italian infertility department. European Journal of Obstetrics & Gynecology and Reproductive Biology, 158, 235-241.
Conrad, R., Schilling, G., Langenbuch, M., Haidl, G., & Liedtke, R. (2001). Alexithymia in male infertility. Human Reproduction, 16, 587-592.
Coughlan, C., Walters, S., & Ledger, W. (2014). A comparison of psychological stress among women with and without reproductive failure. International Journal of Gynecology & Obstetrics, 124, 143-147.
Culley, L., Hudson, N., & Lohan, M. (2013) Where are all the men? The marginalization of men in social scientific research on infertility. Reproductive BioMedicine Online, 27, 225-235.
Darwiche, J., Favez, N., Maillard, F., Germond, M., Guex, P., Despland, J. N., & De Roten, Y. (2013). Couples resolution of an infertility diagnosis before undergoing in vitro fertilization. Swiss Journal of Psychology, 72, 91-102.
De Klerk, C., Hunfeld, J. A. M., Heijnen, E. M., Eijkemans, M. J., Fauser, B. C, Passchier, J., & Macklon, N. S. (2008). Low negative affect prior to treatment is associated with a decreased chance of live birth from a first IVF cycle. Human Reproduction, 23, 112-116.
Del Castillo, M., Arnal, B., Moreno-Rosset, C., Ramírez-Uclés, I., & Urries, A. (2014). ¿Existen diferencias de género en la reacción emocional frente a la infertilidad? [Are there gender differences in emotional reactions to infertility?] (Dissertation). Presented at the symposium “Advances in Reproductive Psychology”. III Congreso Iberoamericano de Psicología de la Salud [3rd Ibero American Congress on Health Psychology]. Sevilla, Spain.
Del Castillo, Moreno-Rosset, C., Martín, M. D., & Ramírez-Uclés, I. (2009). Gender differences in affect, emotional maladjustment and adaptive resources in infertile couples: a positive approach. Annuary of Clinical and Health Psychology, 5, 39-46. Retrieved from http://institucional.us.es/apcs/php/index.php?option=com_content &view=article&id=57&Itemid=11
El Kissi, Y., Amamou, B.,Hidar, S.,Idrissi, K., Khairi, H., & Hadj Ali, B. B. (2014). Quality of life of infertile Tunisian couples and differences acording to gender. International Journal of Gynecology and Obstetrics, 125, 134-137.
Eugster, A., & Vingerhoets, A. J. (1999). Psychological aspects of in vitro fertilization: a review. Social Science & Medicine, 48, 575-589.
Feder, L. (1980). Preconceptive ambivalence and external reality. International Journal of Psychoanalysis, 61, 161-78.
Goldschmidt, O., & Jürgensen, O. (1985). Psychoanalytic study of functionally sterile couples. Case histories and critical review. Psyche, 39, 538-552.
Greenglass, E. R., & Fiksenbaum L. (2009). Proactive coping, positive affect, and well-being. Human Reproduction, 14, 29-39.
Greil, A. L. (1997). Infertility and psychological distress: a critical review of the literature. Social Science and Medicine, 45, 1679-1704.
Hermann, D., Scherg, H., Verres, R., von Hagens, C., Strowitzki, T., & Wischmann, T. (2011). Resilience in infertile couples acts as a protective factor against infertility-specific distress and impaired quality of life. Journal of Assisted Reproduction and Genetics, 28, 1111-1117.
Hernández, M., & Cruzado, J. A. (2013). La atención psicológica a pacientes con cáncer: de la evaluación al tratamiento [Psychological care of cancer patients: from evaluation to treatment]. 1 premio de la XIX edición del Premio de Psicología Aplicada “Rafael Burgaleta” 2012. Clínica y Salud, 24, 1-54.
Huppelschoten, A. G., van Dongen, A.J., Verhaak, C. M., Smeenk, J. M., Kremer, J. A., & Nelen, W. L. (2013). Differences in quality of life and emotional status between infertile women and their partners. Human Reproduction, 28, 2168-2176.
Lechner, L., Bolman C., & van Dalen, A. (2007). Definite involuntary childlessness: Associations between coping, social support and psychological distress. Human Reproduction, 22, 288-294.
Lumley, M. A., Neely, L. C., & Burger, A. J. (2007). The assessment of alexithymia in medical settings: implications for understanding and treating health problems. Journal of personality assessment, 89, 230-246.
Machado, A., Anarte, M. T., & Ruiz de Adana, M. S. (2010). Predictores de calidad de vida en pacientes con Diabetes Mellitus Tipo 1 [Predictors of quality of life in patients with Type 1 Diabetes Mellitus]. Clínica y Salud, 21, 35-47.
Mahajan, N. N., Turnbull, D. A., Davies, M. J., Jindal, U. N., Briggs, N. E., & Taplin, J. E. (2009). Adjustment to infertility: the role of intrapersonal and interpersonal resources/vulnerabilities. Human Reproduction, 24, 906-912.
Mahajan, N. N., Turnbull, D. A., Davies, M. J., Jindal, U. N., Briggs, N. E., & Taplin, J. E. (2010). Changes in affect and state anxiety across an in vitro fertilization/ intracytoplasmic sperm injection cycle. Fertility and Sterility, 93, 517-526.
Martínez-Sánchez, F. (1996). Adaptación Española de la Escala de Alexitimia de
Toronto (TAS-20). [Spanish adaptation of the Toronto Alexithymia Scale (TAS-20)]. Clínica y Salud, 7, 19-32.
Martínez-Sánchez, F., & Ortiz, B. (2000). La evaluación de la alexitimia [Evaluating alexithymia]. In M. Casullo & D. Páez, D. (Eds.), Alexitimia y cultura (pp. 35-51). Buenos Aires: Paidós.
Moreno-Rosset, C., Antequera, R., & Jenaro, C. (2008). DERA. Cuestionario de Desajuste Emocional y Recursos Adaptativos en infertilidad [DERA. Emotional Maladjustment and Adaptive Resources in Infertility Questionnaire]. Premio TEA ediciones 2007. Madrid: Ediciones TEA.
Moreno-Rosset, C., Antequera, R., & Jenaro, C. (2009). Validación del Cuestionario de Desajuste Emocional y Recursos Adaptativos en Infertilidad (DERA) [Validation of the Emotional Maladjustment and Adaptive Resources in infertility questionnaire - DERA]. Psicothema, 21, 118-123.
Moreno-Rosset, C., Antequera, R., Jenaro, C., & Gómez, Y. (2009). Reproductive Psychology: the need for a psychologist in Human Reproduction Units. Clínica y Salud, 20, 79-90.
Moreno-Rosset, C., del Castillo Aparicio, M., Ramírez-Uclés, I., & Martín Díaz. D. M. (2011). Estados emocionales y afectivos en infertilidad: un estudio comparativo con personas fértiles [Emotional and affective states in infertility: a comparative study with fertile people]. Psicología Conductual, 19, 683-703.
Nereu, M. B., Neves, S., & Casado, M. I. (2013). Estrategias de relajación durante el periodo de gestación. Beneficios para la salud [Relaxation strategies during the gestation period. Health Benefits]. Clínica y Salud, 24, 77-83.
Östberg, V., & Lennartsson, C. (2007). Getting by with a little help: The importance of various types of social support for health problems. Scandinavian Journal of Public Health, 35, 197-204.
Pápay, N., Rigó, A., & Nagybányai, O. (2013). A meddõségspecifikus distress alakulása a megküzdési stratégiák és egyéb pszichoszociális változók függvényében [Level of infertility-specific distress in function of coping strategies and other psychological variables]. Magyar Pszichológiai Szemle, 68, 399-418.
Phillips, E., Elander, J., & Montague, J. (2014). Managing multiple goals during fertility treatment: An interpretative phenomenological analysis. Journal of Health Psychology, 19, 531-543.
Rodríguez-Marín, J., Terol, M. C, Lopez-Roig, S., & Pastor, M. A. (1992). Evaluación del afrontamiento del estrés: propiedades psicométricas del cuestionario de formas de afrontamiento de acontecimientos estresantes [Evaluation of coping with stress: psychometric properties of the questionnaire on ways of coping with stressful events]. Revista de Psicología de la Salud, 4, 59-84.
Sandín, B., Chorot, P., Lostao, L., Joiner, T. E., Santed, M. A., & Valiente, R. (1999). Escala PANAS de afecto positivo y negativo: validación factorial y convergencia transcultural [The PANAS scale on positive and negative affect: factorial validation and cross-cultural convergence]. Psicothema, 11, 37-51.
Schalet, B. D., Cook, K. F., Choi, S. W., & Cella, D. (2014). Establishing a common metric for self-reported anxiety: Linking the MASQ, PANAS, and GAD-7 to PROMIS Anxiety. Journal of Anxiety Disorders, 28, 88-96.
Shi, X., Wu, P., & Zhu, X. (2006). Alexithymia and its features in patients with infertility. Chinese Journal of Clinical Psychology, 14, 403-404.
Spielberg, C. D., Gorsuch, R. L., & Lushene, R. E. (1970). Manual for the State/Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologist Press [versión española, Madrid: Ediciones TEA, 2008].
Van Dongen, A. J., Kremer, J. A., Van Sluisveld, N., Verhaak, C. M., & Nelen, W. L. (2012). Feasibility of screening patients for emotional risk factors before in vitro fertilization in daily clinical practice: a process evaluation. Human Reproduction, 27, 3493-3501.
Verhaak, C. M., Lintsen, A. M., Evers, A. W., & Braat, D. (2010). Who is at risk of emotional problems and how do you know? Screening of women going for IVF treatment. Human Reproduction, 25, 1234-1240.
Verhaak, C. M., Smeenk, J. M., Evers, A. W., Kremer, J. A., Kraaimaat, F. W., & Braat, D. (2007). Women’s emotional adjustment to IVF: A systematic review of 25 years of research. Human Reproduction Update, 13, 27-36.
Watson, D., Clark, L. A., & Tellegen, A. (1988). Development and validation of brief measures of positive and negative affect: the PANAS scales. Journal of Personality and Social Psychology, 54, 1063-1070.
Yu, Y., Peng, L., Chen, L., Long, L., He, W., Li, M., & Wang, T. (2014). Resilience and social support promote posttraumatic growth of women with infertility: The mediating role of positive coping. Psychiatry research, 215, 401-405.