The use of guidelines for goal-oriented resuscitation in patients with severe sepsis and septic shock has a positive impact on multiple organ failure and mortality outcomes. However, in patients over 65, adherence to the guidelines may be less stringent because of considerations of lower functional, cardiac, pulmonary and renal reserve. This study compares adherence to the guidelines and compliance with resuscitation goals by the healthcare staff in populations over and under 65 years of age.
ObjectiveTo determine adherence to the guidelines by the healthcare staff in the treatment of severe sepsis and septic shock in the group over 65 years of age, compared with patients under 65.
Materials and methodsObservational, analytical, cross-sectional study of patients under and over 65 years of age admitted to the Intensive Care Unit (ICU) after having been diagnosed with severe sepsis and septic shock. Frequency of adherence to the guidelines was determined and a comparison of the different resuscitation goals in relation to adherence to the guidelines was made.
ResultsExcept for adherence to early initiation of antibiotic therapy, there was better adherence to the other goals in the patients under 65 when compared to patients over 65. Adherence to the guidelines declined progressively as the number of goals increased.
ConclusionsThere was a lower adherence to resuscitation guidelines in the group of patients over 65 with severe sepsis and septic shock when compared with the group of patients under 65.
El uso de guías de reanimación por metas en los pacientes con sepsis severa y choque séptico, genera un impacto benéfico en los desenlaces de disfunción orgánica múltiple y de la mortalidad, sin embargo en los pacientes mayores de 65 años, la adherencia a las guías puede ser menor, por la menor reserva funcional, cardíaca, pulmonar y renal. En el presente estudio comparamos la adherencia a la guía y el cumplimiento de las metas de reanimación por parte del personal de salud en la población mayor y menor de 65 años.
ObjetivoDeterminar la adherencia a las guías para el tratamiento de la sepsis severa y choque séptico por parte del personal de salud en el grupo mayor de 65 años comparado con el grupo de pacientes menores de 65 años.
Materiales y métodosEstudio observacional analítico de corte transversal de los pacientes menores y mayores de 65 años ingresados a la Unidad de Cuidados Intensivos (UCI), con diagnóstico de sepsis severa y choque séptico, se determinó la frecuencia de adherencia a la guía para cada grupo de edades y se compararon las diferentes metas de reanimación en relación a la adherencia.
ResultadosExcepto por la adherencia del inicio temprano de la antibiótico terapia, las demás metas presentaron una mejor adherencia, en el grupo de pacientes menores de 65 años cuando se compararon con los pacientes mayores de 65 años, la adherencia para ambos grupos disminuyo progresivamente a medida que se consideraron mayor número de metas.
ConclusionesExiste una menor adherencia a las guías de reanimación, en el grupo de grupo de pacientes mayores de 65 años con sepsis severa y choque séptico cuando se compara con el grupo de pacientes menores de 65 años.
The elderly population has increased as a result of a demographic transition driven by lower fertility and an increase in life expectancy.1
Despite the fact that the elderly account for only one-fifth of the general population, they represent two-thirds of patients admitted to the hospital with a diagnosis of sepsis.2 The incidence of severe sepsis is much higher among the elderly when compared with younger patients, and this difference is greater particularly in the group between 75 and 79 years of age, and the incidence of sepsis among patients over 65 is almost 13 times higher than in younger patients (26.2 cases per 1000 inhabitants).3 Studies of the diagnosis and treatment of sepsis usually exclude subjects with multiple comorbidities or old age groups. However, given longer life expectancy, the elderly population subgroup will be admitted to the ICU with a higher frequency, and their management poses a significant challenge for intensive care physicians.2
Clinical practice guidelines for the treatment of sepsis published in recent years provide a series of recommendations which have shown to have a positive impact on outcomes in septic patients.4–6 On the other hand, its has been documented that non-adherence to the guidelines results in worse outcomes.3 However, there is no detailed information to date regarding adherence to these guidelines in the subgroup of patients over 65 years of age. This prompted us to explore adherence to resuscitation guidelines in the treatment of severe sepsis and septic shock, as well as differences in adherence by the healthcare staff in the group over 65 compared with patients under 65 years of age.
MethodsFollowing approval from the ethics committee at Clínica Shaio, electronic records for the period between January 2009 and December 2014 were reviewed in order to identify all the cases diagnosed with severe sepsis and septic shock admitted to the ICU in accordance with the criteria of the American College of Chest Physicians (ACP) and the Society of Critical Care Medicine (SCCM).4 Overall, 463 patients over 65 years of age and 523 patients under 65 were identified during the study period, and 200 patients were selected randomly in each group using random number generation in an Excel sheet based on the clinical record numbers for each group. Patients with incomplete information or who met the exclusion criteria were replaced systematically with the next patient on the list who met the inclusion criteria.
The estimated sample size was 200 patients in each group in order to determine a percentage of adherence of close to 60% based on prior studies,7 a 20% difference between age groups, and a power of 80%.
The data recorded included gender, age, Chronic Health Evaluation II (APACHE II),8 origin of the sepsis, and comorbidities, as well as achievement of the resuscitation goals (lactate level measurements, sampling for blood culture before initiating antibiotics, administration of broad spectrum antibiotics, administration of 30ml/kg of crystalloids for hypotension, or lactate >4mmol/l within the first 3h, and mean arterial pressure >65mmHg, vasopressor administration in the presence of persistent hypotension, central venous pressure >8mm/Hg, central venous oxygen saturation >70%, and urinary output >0.5cc/kg/h) within the first 6h.5,9–11
The variables included were analysed using the STATA 12.0 statistical software, and frequencies were obtained for categorical and nominal variables, whereas central trend and scatter were obtained for continuous variables. After determining adherence to the sepsis guidelines in each group, a test of difference between proportions was used to compare the frequencies obtained in each group, applying a level of significance of 0.05 and a power of 80%.
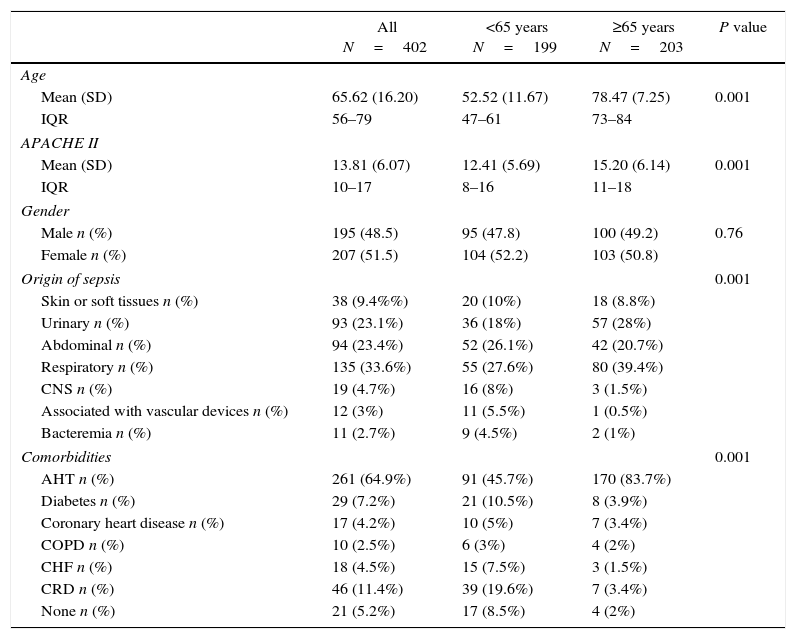
ResultsOverall, 402 patients were included, and the degree of severity assessed using the APACHE II scale showed a mean score of 12 vs. 15 (p<0.001) in patients under 65 years of age compared to those over 65, respectively. Regarding the origin of sepsis in the two groups, there was a highest proportion of sepsis of respiratory origin (33.6%), followed by urinary origin in the group of patients over 65 (28%) and abdominal sepsis in the group of patients under 65 (26.1%). As was to be expected, comorbidities were more frequent in the older age group (98 vs. 91%), and the breakdown by conditions showed that there was a higher proportion of arterial hypertension in both groups, with no difference by gender distribution (Table 1).
General characteristics of the population.
| All N=402 | <65 years N=199 | ≥65 years N=203 | P value | |
|---|---|---|---|---|
| Age | ||||
| Mean (SD) | 65.62 (16.20) | 52.52 (11.67) | 78.47 (7.25) | 0.001 |
| IQR | 56–79 | 47–61 | 73–84 | |
| APACHE II | ||||
| Mean (SD) | 13.81 (6.07) | 12.41 (5.69) | 15.20 (6.14) | 0.001 |
| IQR | 10–17 | 8–16 | 11–18 | |
| Gender | ||||
| Male n (%) | 195 (48.5) | 95 (47.8) | 100 (49.2) | 0.76 |
| Female n (%) | 207 (51.5) | 104 (52.2) | 103 (50.8) | |
| Origin of sepsis | 0.001 | |||
| Skin or soft tissues n (%) | 38 (9.4%%) | 20 (10%) | 18 (8.8%) | |
| Urinary n (%) | 93 (23.1%) | 36 (18%) | 57 (28%) | |
| Abdominal n (%) | 94 (23.4%) | 52 (26.1%) | 42 (20.7%) | |
| Respiratory n (%) | 135 (33.6%) | 55 (27.6%) | 80 (39.4%) | |
| CNS n (%) | 19 (4.7%) | 16 (8%) | 3 (1.5%) | |
| Associated with vascular devices n (%) | 12 (3%) | 11 (5.5%) | 1 (0.5%) | |
| Bacteremia n (%) | 11 (2.7%) | 9 (4.5%) | 2 (1%) | |
| Comorbidities | 0.001 | |||
| AHT n (%) | 261 (64.9%) | 91 (45.7%) | 170 (83.7%) | |
| Diabetes n (%) | 29 (7.2%) | 21 (10.5%) | 8 (3.9%) | |
| Coronary heart disease n (%) | 17 (4.2%) | 10 (5%) | 7 (3.4%) | |
| COPD n (%) | 10 (2.5%) | 6 (3%) | 4 (2%) | |
| CHF n (%) | 18 (4.5%) | 15 (7.5%) | 3 (1.5%) | |
| CRD n (%) | 46 (11.4%) | 39 (19.6%) | 7 (3.4%) | |
| None n (%) | 21 (5.2%) | 17 (8.5%) | 4 (2%) | |
AHT, systemic arterial hypertension; COPD, chronic obstructive pulmonary disease; CHF, congestive heart failure; CRD, chronic renal disease.
Source: The authors.
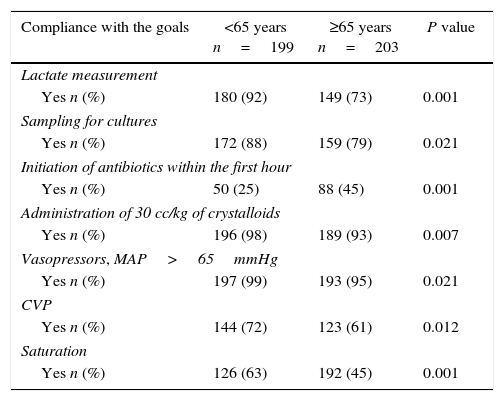
When the criterion of compliance with all the 9 goals was applied to measure adherence to the guidelines, a percentage as low as 10% was found for patients under 65 and as low as 10.8% for subjects over 65 years of age (p=0.757), mainly due to the fact that the goal with the lowest adherence was initiation of antibiotic therapy within the first hour; the percentage of adherence for the remaining eight goals was higher, as shown in Table 2.
Adherence to resuscitation goals by the healthcare staff in the ICU by age group.
| Compliance with the goals | <65 years n=199 | ≥65 years n=203 | P value |
|---|---|---|---|
| Lactate measurement | |||
| Yes n (%) | 180 (92) | 149 (73) | 0.001 |
| Sampling for cultures | |||
| Yes n (%) | 172 (88) | 159 (79) | 0.021 |
| Initiation of antibiotics within the first hour | |||
| Yes n (%) | 50 (25) | 88 (45) | 0.001 |
| Administration of 30 cc/kg of crystalloids | |||
| Yes n (%) | 196 (98) | 189 (93) | 0.007 |
| Vasopressors, MAP>65mmHg | |||
| Yes n (%) | 197 (99) | 193 (95) | 0.021 |
| CVP | |||
| Yes n (%) | 144 (72) | 123 (61) | 0.012 |
| Saturation | |||
| Yes n (%) | 126 (63) | 192 (45) | 0.001 |
Source: Authors.
However, adherence to the initiation of therapy with broad spectrum antibiotics was higher in the group over 65 years of age (43% vs. 25%, respectively) (p<0.001), whereas the second lowest in both groups was adherence to the goal of venous oxygen saturation equal to or greater than 70% within the first 6h, and it was lower in the group over 65 years (45.3% vs. 63.3%) with a statistically significant difference (p<0.001) consistent with the lower use of invasive monitoring methods and lower administration of blood products and inotropes in this population group.
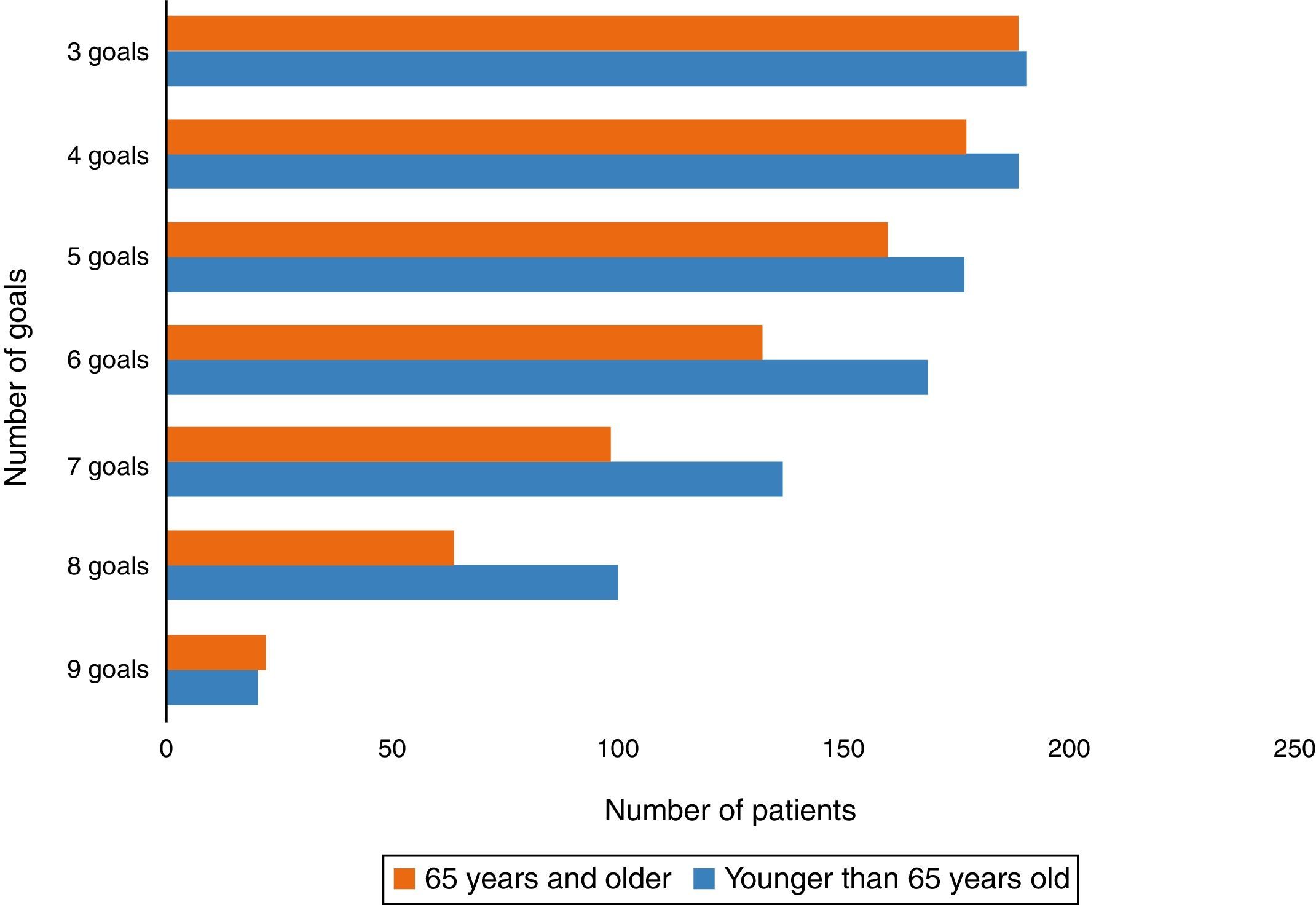
Regarding the number of goals met and adherence to the guidelines, Fig. 1 shows that the smaller the number of goals to be met the higher the adherence, reaching 95% in the group under 65 and 93.1% in the group of patients over 65, with 3 goals being met (p=0.083). For adherence to 4–8 goals there was a significant difference between the two groups (p<0.001) with a lower rate of compliance in the group over 65 years of age.
DiscussionMany of the strategies used for early treatment of sepsis and septic shock in adult patients over 65 years of age are limited by the fear of complications that therapies might bring about when administered to patients with lower cardiovascular, pulmonary or renal reserve, leading to the consideration that adherence to protocols may be lower in this population.
On the other hand, of almost 33% of elderly patients in the ICU discharged from specialised care institutions, almost half are readmitted, and 25–65% die within the next 6 months.12,13 Consequently, the lower life expectancy could also influence adherence on the part of the practitioners.
In this study, a significantly higher percentage of patients over 65 had at least one concomitant disease associated with the diagnosis of sepsis and septic shock as compared to patients under 65, which may also explain the less aggressive therapeutic measures used in the management of this group based on the assumption of a poorer outcome and a poor prognosis in the short and medium-term. These findings have already been described in studies by Lemay AC and Carbajal-Guerrero.14,15
This study found higher adherence to the initiation of antibiotic therapy in patients over 65, and the difference is consistent with a higher number of urinary and respiratory tract infections in this population. This finding could be explained on the basis of the earlier identification of sepsis given its more florid and pathognomonic clinical manifestation, compared to other sources of infection, and this could explain delay in the initiation of antibiotic therapy in the group of patients under 65 years of age.
Despite the fact that adherence by the healthcare staff to resuscitation guidelines in sepsis has resulted in a significant reduction in mortality and there has been a reduction in the percentage of non-compliance in different studies conducted over the years, it is noteworthy that adherence to the guidelines by the healthcare staff in the intensive care unit was lower in both groups regardless of age as the number of goals increased. In fact, in contrast with the 73% reported by Miller et al.,16 and the 58% reported by Mikkelsen et al.,17 the percentage of non-compliance in our study was approximately 10%, highlighting that there is still a lot to be done in terms of implementing strategies designed to standardise protocols and therapeutic measures with the aim of optimising compliance with these goals. Likewise, a question arises regarding the difficulty of transferring knowledge to practice with the early recognition of this condition, as shown by Quintero et al.18 who found results similar and event worse than ours in that no more than 8 goals were met by any one patient in the study.
Specifically in terms of adherence by the healthcare staff in the intensive care unit to the goal of initiating antibiotic therapy within the first hour after sepsis is recognised, unfortunately, compared to other studies,19 in the two groups of our population, it was shown to be less than 50%.
ConclusionsAlthough positive results with the implementation of goal-directed guidelines in terms of reduced mortality in patients with severe sepsis and septic shock has been widely shown,20,21 low adherence by the healthcare staff in the intensive care unit still prevails, with the resulting low compliance with resuscitation goals in patients under 65 years as well as in patients over 65 admitted to the intensive care unit.
There is a statistically significant difference in adherence by the healthcare staff in the intensive care unit to the sepsis treatment guidelines, which is lower in patients over 65. This finding may be associated with the preconceived notion of unfavourable outcomes and complications associated with invasive monitoring and treatment procedures because of their lower functional reserve, added to the higher number of comorbidities. This has a negative impact on timely initiation of treatment for septic shock and severe sepsis in the elderly population.
Although one of the goals with the highest impact on outcomes for patients with sepsis is the initiation of broad spectrum antibiotics within the first hour after diagnosis, adherence to this measure and compliance with the goal are still under 50% in both age groups.
There is a need to optimise actions aimed at the early recognition and timely and adequate implementation of stringent protocols for the management of sepsis in all population groups regardless of age and associated comorbidities.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FinancingThe authors did not receive sponsorship to carry out this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Negret-Delgado MdP, Puentes-Corredor S, Oliveros H, Poveda-Henao CM, Pareja-Navarro PA, Boada-Becerra NA. Adherencia a la guía de manejo de sepsis severa y choque séptico en pacientes mayores de 65 años que ingresan a UCI. Rev Colomb Anestesiol. 2016;44:299–304.