Cystic fibrosis (CF) is an inherited autosomal recessive disorder appearing in approximately 1:2000 live births in the Caucasian population, responsible for early mortality in affected patients, often before they reach reproductive age. It was first described in the 1930s, and it was associated with a dismal prognosis. Improvements in the treatment of these patients have resulted in improved quality of life and longer life expectancy beyond sexual maturity. Since the first report of pregnancy in a patient with cystic fibrosis in 1960, the rates of conception have increased dramatically. Lung morbidity requires priority pain management during labor in order to reduce the burden imposed by pain on the cardiorespiratory system. Analgesia delivered over the epidural catheter reduces and eliminates pain, enhancing comfort and making a line available for regional anesthesia if required. This eliminates the need for orotracheal intubation and the deleterious effect on the weakened respiratory system.
La fibrosis quística (FQ) es un trastorno con herencia autosómica recesiva que aparece en aproximadamente 1:2.000 nacidos vivos en la población caucásica, responsable de una mortalidad precoz de los pacientes afectados, frecuentemente antes de alcanzar la edad reproductiva. La primera descripción de FQ en la literatura data de 1930, asociada a un pronóstico sombrío. La mejora en el manejo de estos pacientes ha llevado a una mejor calidad de vida asociada a una elevación en la esperanza de vida, permitiendo llegar con más frecuencia a la edad reproductiva. Se han descrito varios casos a partir del primer reporte de un caso de una parturienta portadora de FQ, en 1960. La morbilidad que origina la FQ a nivel pulmonar hace que el manejo del dolor durante el trabajo de parto y el parto sea prioritario, con el objetivo de reducir la sobrecarga que el dolor produce sobre el sistema cardiorrespiratorio. La administración de analgesia a través del catéter epidural reduce y elimina el dolor, permitiendo un parto más cómodo para la paciente y dejando disponible una vía para administrar anestesia regional, en caso de ser necesaria, evitando así la intubación orotraqueal y el efecto deletéreo que tendría sobre un sistema respiratorio debilitado.
Cystic fibrosis (CF) is one of the most frequent genetic disorders. In the past, it was considered a disease of childhood, and seldom were pregnant patients found. However, with the huge treatment breakthroughs, quality of life and life expectancy have improved and so have the numbers of pregnant patients with CF.1,2
CF is an autosomal recessive inherited disorder with an incidence of 1:2000 and 1:5000 among Europeans. The genetic mutation gives rise to a defect in the transmembrane conduction regulation because of a disruption in a chlorine channel protein in the epithelial cells of mucosal surfaces. In childhood, it manifests as a respiratory disease, although malabsorption is often the most debilitating disorder.3 Early reports of pregnancy in patients with CF show a dismal perspective, although some suggest that patients usually tolerate pregnancy well and that cardiac function deterioration is rare, except in women with severe pre-existing disease.4–7
Clinical caseWe present a case of a 34-year-old gravida I patient with term pregnancy who came to the emergency service of our hospital in labor. The history revealed that the patient was diagnosed with CF at 27 years of age because of repeated episodes of sinusitis and chronic coughing, a positive sweat test and the identification of a G542X/3272-26A>6 gene mutation. She also had heterozygous alpha 1-antitrypsine deficit, osteoporosis and a history of cholelithiasis. Moreover, as a result of her primary disease, the patient had exocrine pancreatic insufficiency. Her regular medications included salmeterol xinafoate one puff every 12h; salbutamol twice a day; colistin for chronic respiratory Scedosporium and Aspergillus fumigatus complex and occasional isolation of atypical mycobateria in sputum, one million units inhaled every 12h; mometasone twice a day; pancreatic enzymes 10,000 three times a day; calcium (Ideos®) 2 pills a day; vitamin A+E one pill a day plus vitamin D, two drops per day. Spirometry had been performed at her last pulmonology assessment, with the following findings: forced vital capacity (FVC liters/%) 2.98/88, forced expiratory volume in one second (FEV1 liters/%) 2.17/75, Tiffenau index 73%, SaO2 97%. On admission, tests did not reveal significant abnormalities; the chest X-ray showed evidence of bilateral bronchiectasis with no apparent occupation and inflation areas.
Given the patient's request for epidural analgesia for labor and, having checked the clinical record, the technique was used with loss of air resistance, placement of the epidural catheter and performance of a test dose using 3ml of 0.25% bupivacaine+epinephrine 1:200,000, which was negative. Consequently, we proceeded to inject an initial dose of 10ml of 0.25% plus fentanyl 10μg and initiated a continuous infusion of 0.125% levobupivacaine at a rate of 7ml/h with the option of additional patient-controlled boluses of 10ml of the anesthetic solution, the usual protocol at our tertiary hospital.8
Ten minutes after the administration of the first analgesic bolus, the patient was pain-free and did not exhibit any form of motor blockade. Analgesic level to cold stimulus was T8. Vital signs were: non-invasive blood pressure 110/80mmHg, heart rate 88 l/m and ambient air oxygen saturation 93%. The patient cooperated and remained pain-free throughout labor, requiring one additional bolus of medication during the advanced phase; 5h after placing the epidural catheter, the patient delivered a live boy who weighed 2800×g with an Apgar score of 9/10. The epidural catheter was removed after delivery and the patient was transferred to the post-partum unit.
DiscussionPregnancy creates physiological changes that may pose difficulties with anesthesia, in particular with airway management,9 thus requiring special precautions. This complexity is even greater when pregnancy is associated with a condition like CF, which compromises several systems of special concern in anesthesia, as is the case of the cardiopulmonary system.10,11
Pregnant patients with CF present obstructive patterns on pulmonary function tests, most commonly associated with chronic infections caused by difficult germs,12 making orotracheal intubation unwise.13
One of the primary objectives of the anesthesiologist during the peripartum period is to maintain optimum cardiorespiratory function because the pain from uterine contractions increases oxygen consumption and ventilatory requirements. For this reason, effective pain relief must be provided from the start of labor.14 Epidural analgesia is effective at controlling pain, avoids hemodynamic variations secondary to the pain from uterine contractions, and reduces circulating catecholamines and metabolic demands associated with labor.15 It also enables fast anesthetic blockade in the event an emergency C-section is needed, thus avoiding general anesthesia.16
Low-concentration bupivacaine and its byproduct levobupivacaine solutions with opioid supplementation provide good-quality analgesia with a very low incidence of hypotension, motor blockade or respiratory compromise.17 Aside from maintaining the sensitive level under T8, compromise of the ventilatory function resulting from excess motor block is avoided. The sitting position is also recommended to the greatest extent possible, as well as fluid restriction.18
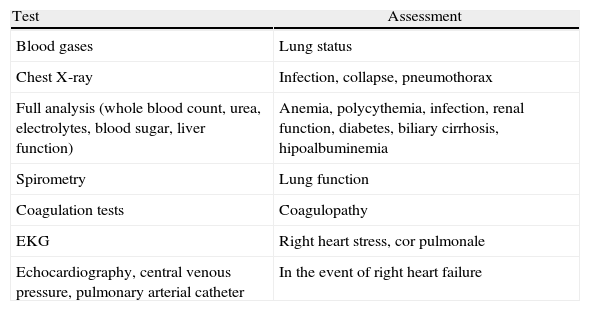
Finally, a pregnant woman with CF who comes to the delivery room requires a careful examination of the airway, pulmonary status, nutritional status, and recent diagnostic tests (see Table 1), not ruling out the possibility of general anesthesia.
Recommended tests for women with CF in labor.
| Test | Assessment |
| Blood gases | Lung status |
| Chest X-ray | Infection, collapse, pneumothorax |
| Full analysis (whole blood count, urea, electrolytes, blood sugar, liver function) | Anemia, polycythemia, infection, renal function, diabetes, biliary cirrhosis, hipoalbuminemia |
| Spirometry | Lung function |
| Coagulation tests | Coagulopathy |
| EKG | Right heart stress, cor pulmonale |
| Echocardiography, central venous pressure, pulmonary arterial catheter | In the event of right heart failure |
Taken from Howell.3
We believe that epidural analgesia must be considered as first choice management in pregnant women with CF. Adequate epidural block results in less metabolic stress associated with labor, and improves cardiorespiratory function throughout the process of dilatation and delivery, also allowing sufficient anesthetic depth in the event of an emergency C-section.
FundingNone.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Maggi G, et al. Manejo analgésico de la parturienta con fibrosis quística. Rev Colomb Anestesiol. 2013. http://dx.doi.org/10.1016/j.rca.2013.05.007.