Immediate postoperative pain has been underestimated and managed inadequately.
ObjectivesTo assess perceived pain 4h after surgery in patients at the San Jorge University Hospital in the city of Pereira.
Materials and methodsCross-sectional study in patients over 18 years of age was conducted between September 2nd and October 28th, 2011. Postoperative pain intensity was assessed using the Visual Analog Scale, 4h after completing the procedure. Social, demographic, clinical and pharmacological variables were considered. The analysis was done using the SPSS 20.0 for Windows.
ResultsOf the 213 postoperative patients studied, 114 (53.6%) were women and 99 (46.4%) were men, with a mean age of 47.1±20.0 years. At 4h, 51.4% of patients did not have pain control. There was a statistically significant association between lack of control and age, living in the urban area, type of surgery, non-adherence to the dose, and monotherapy analgesia.
DiscussionInadequate pain control requires revisiting its management, ideally on the basis of clinical practice guidelines and using analgesic drugs at adequate doses and intervals.
El dolor en el posquirúrgico inmediato ha sido subvalorado y manejado inadecuadamente.
ObjetivosEvaluar la percepción del dolor a las 4 h del postoperatorio de pacientes del Hospital Universitario San Jorge de Pereira (Colombia).
Materiales y métodosEstudio de corte transversal en pacientes mayores de 18 años entre el 2 de septiembre y el 28 de octubre de 2011. Se valoró la intensidad del dolor postoperatorio mediante escala visual analógica a las 4 h del procedimiento. Se consideraron variables sociodemográficas, clínicas y farmacológicas. El análisis se hizo con SPSS 20.0 para Windows.
ResultadosSe evaluaron 213 pacientes en postoperatorio, 114 (53,6%) mujeres y 99 (46,4%) hombres, con edad promedio de 47,1 ± 20,0 años. El 51,4% de los pacientes no tenía controlado el dolor a las 4 h. Las variables edad, residencia urbana, tipo de cirugía, incumplimiento de la dosis y monoterapia analgésica se asociaron de manera estadísticamente significativa con la falta de control.
DiscusiónEl inadecuado control del dolor obliga a replantear su manejo idealmente con guías de práctica clínica y con el empleo de medicamentos analgésicos a las dosis e intervalos adecuados.
According to the International Association for the Study of Pain (I.A.S.P.), pain is an unpleasant sensory and emotional experience associated with existing or potential tissue injury.1 Dramatic progress has been made in controlling postoperative pain and there are now multiple experts and publications in this field.2 Despite significant interest in improving postoperative pain management, evidence shows that world prevalence of moderately intense pain in hospitalized patients ranges between 26.0%, and 33.0%, whereas prevalence of severe pain has been estimated to be between 8.0% and 13.0%.3Postoperative complications caused by pain in the main organ systems have been well-described. Tissue injury triggers a series of responses that may cause ventilation abnormalities (5.0–25.0% of patients), local circulation disorders, gastrointestinal and urinary disorders, and even lead to infarction or heart failure, not to mention other abnormalities in carbohydrate, lipid and protein metabolism, as well as diencephalic and cortical responses, anxiety, fear and depression, that occur when pain is not well managed.4–6
It is now known that adequate control of acute postoperative pain is one of the cornerstones in achieving fast postoperative recovery. Administratively, this results in shorter hospital stays and lower costs, and from the medical standpoint, it implies reduced morbidity and mortality.7,8 Ever since the American Pain Society declared pain to be the “fifth vital sign”, several initiatives have been undertaken to improve its control, including the implementation of a numerical scoring scale called the Visual Analog Scale (VAS) consisting of 10 integer numbers for the subjective measurement of pain intensity.9,10 A pain score of 4 or more requires a comprehensive pain assessment and rapid intervention by the healthcare provider.11,12
Although no drug regimen has been able to completely eliminate postoperative morbidity and mortality, adequate pain management leads to early ambulation, which, together with vomiting and ileus control, oral feeding, and preoperative antibiotic therapy, is the mainstay for comprehensive postoperative management.13 The pharmacological armamentarium for pain management available at the present time is quite broad and includes several groups such as opioids, analgesics, non-steroidal anti-inflammatory agents (NSAIDS), and local anesthetics. It is recommended to provide two analgesics with a different mechanism of action in order to achieve more effective analgesia and reduce adverse reactions with the use of a lower dose of each drug.14
The goal of this study was to determine perceived pain intensity in the postoperative period by means of pain assessments at 4h using the VAS, and to determine the social, demographic, clinical and pharmacological variables associated with pain control or lack of control in patients taken to surgery at the San Jorge University Hospital in Pereira (HUSJ), in order to optimize management.
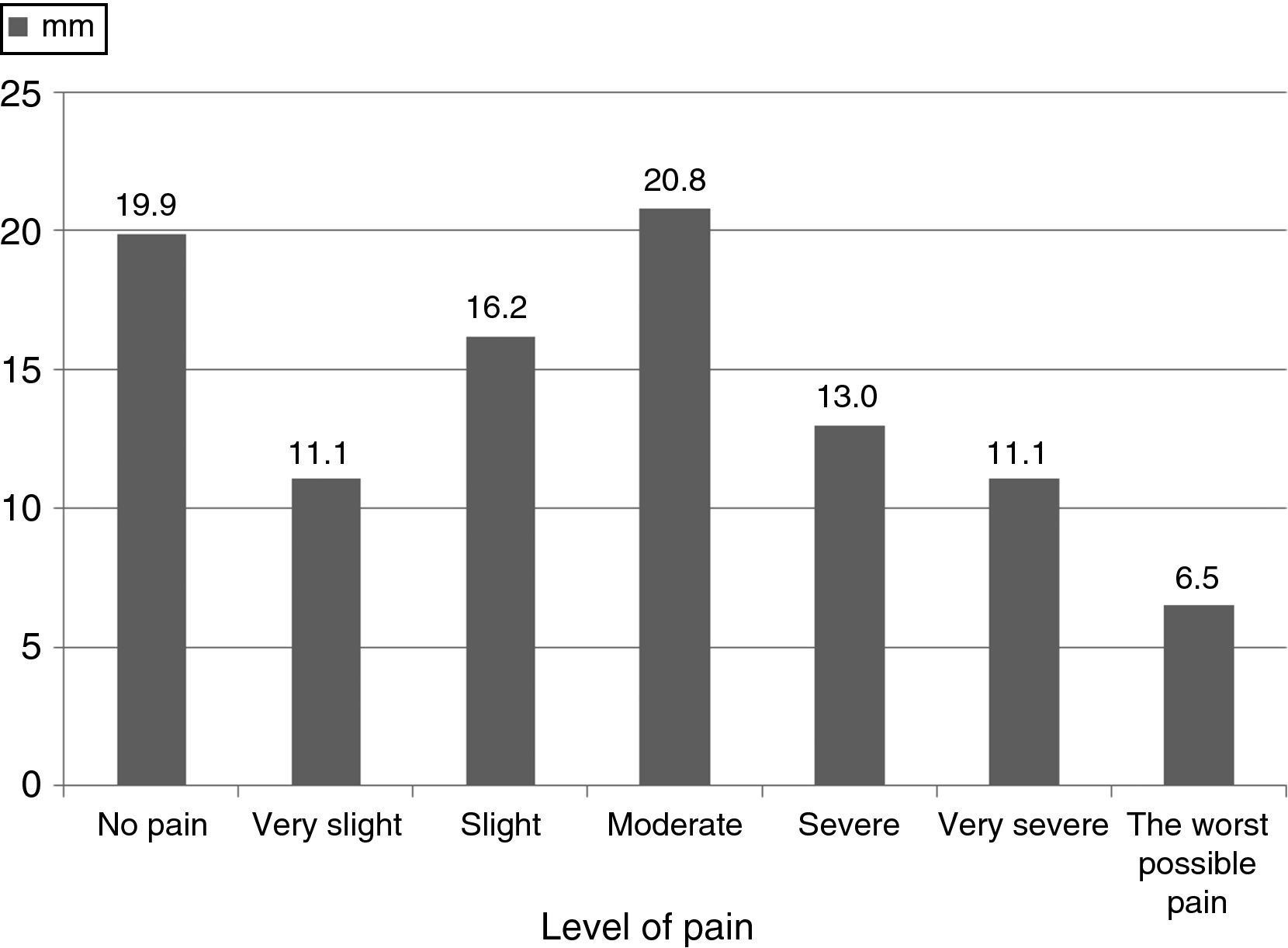
Materials and methodsA cross-sectional study was conducted at HUSJ in a population of patients over 18 years of age undergoing surgery between 7:00am and 6:00pm, from September 2nd to October 28th, 2011. Assessment of postoperative pain intensity was done using the VAS in millimeters (mm), in which five categories were established. Values of 0 and 100 are absolute and represent independent categories, and the following reference values were used: 0mm absence of pain, 1–19mm very mild pain, 20–39mm mild pain, 40–59mm intermediate pain, 60–79mm severe pain, 80–99mm very severe pain, and 100mm the worst possible pain; scores over 40mm were used for undefined pain. Consequently, pain was considered to be under control when scores were lower than or equal to 39mm.10,15–17
Assessment was done 4h after completion of the procedure with a view for assessing immediate postoperative pain management. Patients who could not take the test because of neurologic deficits, disabling motor disorders, mental retardation and severe mental diseases were excluded. The information was obtained through patient interviews by duly trained final-year medical students of Universidad Tecnológica in Pereira. Access to patient clinical records and surgical notes was also obtained by means of an informed consent. The data collection tool was developed by the researchers and included the following variables, besides the VAS:
Social, demographic and toxicological variables: Age, gender, health insurance regime (subsidized or contributive), socio-economic bracket (low, medium, high), education (primary, secondary, higher), place of residence (urban or rural), cigarette smoking, use of psychoactive substances, NSAIDS, steroids and anti-depressants.
Clinical variables: Type of surgical procedure (general, brain, urologic, plastic, otolaryngological, gynecological surgery, etc.), intra- and post-operative complications, type of anesthesia (general inhaled, intravenous, conductive, local, etc.), estimated surgical risk (high, moderate and low). For this latter variable, low risk included minimally invasive surgery with blood losses under a 200cm3; moderate risk included moderately invasive procedures with fluid exchange and potential blood losses of up to 1000cm3, and/or moderate mortality/morbidity; and high risk included highly invasive procedures such as radical or extensive upper abdominal, thoracic or brain surgeries with potential blood losses greater than 1000cm3 and significant associated mortality/morbidity.
Pharmacological variables: Analgesics prescribed immediately after surgery and up to 4h, were grouped according to pharmacological class and their use either as monotherapy or in combination, dose, dosing interval for each, drug-related adverse reactions, and use of analgesic premedication. Morphine, meperidine and fentanyl were used as strong opioids and tramadol was used as a weak opioid.
The protocol was approved by the Ethics Committee of the Health Sciences School at Universidad Tecnológica in Pereira, under the category of “Low-to-minimum risk research”, in accordance with Resolution No. 008430 of 1993 of the Colombian Health Ministry, which sets forth the scientific, technical and administrative standards for health research. The analysis was conducted using the SPSS software, version 2.0 for Windows (IBM, USA). The Student t test or ANOVA were used for comparing quantitative variables, and the χ2 test was used for comparing categorical variables. Logistic regression models were applied using pain control as the dependent variable, and those that were significant in the bivariate analysis were used as independent variables. A statistical significance level of p<0.05 was established.
ResultsOf a total of 213 postoperative patients who were assessed, 114 (53.6%) were women and 99 (46.4%) were men, with a mean age of 47.1±20.0 years (range: 18–86 years). Table 1 summarizes the social, demographic and clinical characteristics of the patients included in the study. Pain measurements using the VAS were assessed in 213, with a mean pain score of 40.0mm, where 111 (51.4%) patients had no pain control (VAS≥40mm) and 102 (47.2%) had pain control; moreover, it was found that 25 patients (11.7%) required analgesia during their hospital stay as a result of pain intensity. In addition, there were nine patients with no analgesic prescription, including one case of exploratory laparotomy and one C-section.
Social, demographic, medical and surgical characteristics of 213 surgical patients, 2011.
| Social and demographic characteristics | n=213 | (%) |
| Gender (males/females) | 99/114 | 46.4/53.6 |
| Age (mean±SD, years) | 47.1±20.0 | |
| Marital status: Single/partner | 44/168 | 20.4/77.8 |
| Health Insurance Regime: Contributive/Subsidized/NA | 13/197 | 6.0/91.2/2.8 |
| Education: Primary/Secondary/Higher | 129/75/9 | 59.7/34.7/4.1 |
| Residence: Urban/Rural | 156/57 | 72.2/26.4 |
| Socio-economic bracket: 1/2/3/4/5 | 127/66/13/2/1 | 58.8/30.6/6.0/0.9/0.5 |
| Personal history (consumption) | ||
| Cigarette smoking | 66 | 30.6 |
| Psychoactive substances | 13 | 6 |
| Alcohol | 47 | 21.8 |
| Pharmacological history | ||
| NSAIDS | 46 | 21.3 |
| Anti-depressants | 4 | 1.9 |
| Glucocorticoids | 7 | 3.2 |
| Type of surgery | ||
| Plastic | 10 | 4.7 |
| Gynecological | 27 | 12.7 |
| Orthopedic | 82 | 38.5 |
| General | 61 | 28.6 |
| Urology | 17 | 8.0 |
| Laparoscopic | 3 | 1.4 |
| Neurosurgery | 6 | 2.8 |
| Peripheral vascular | 4 | 1.9 |
| Otolaryngological | 3 | 1.4 |
| Anesthetic premedication | ||
| Yes/No | 8/205 | 3.8/96.2 |
| Type of anesthesia | ||
| General intravenous | 21 | 9.7 |
| Conductive | 83 | 39.9 |
| General inhaled | 91 | 42.4 |
| Regional | 7 | 3.2 |
| Local | 10 | 4.4 |
| N/A | 1 | 0.40 |
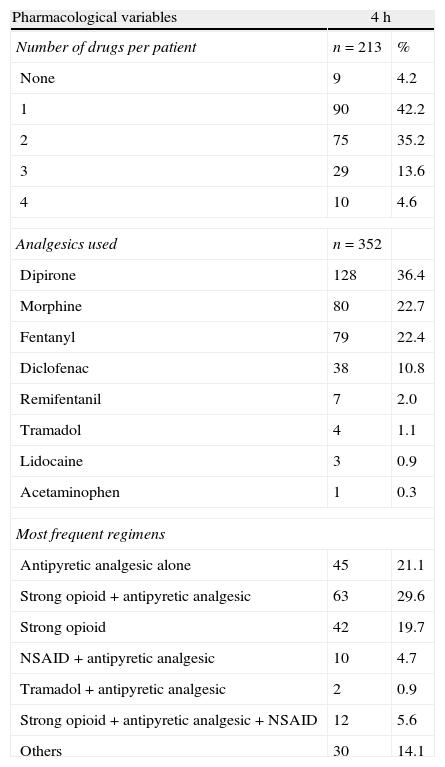
Fig. 1 shows patient distribution by pain range found on assessment, and Table 2 groups analgesics, dose and number of medications received by each patient and their associations, arranged by frequency of use for pain management, where dipirone was the most frequently used analgesic in monotherapy and in combination, followed by morphine and fentanyl.
Drugs and regimens most commonly used in postoperative patients, 2011.
| Pharmacological variables | 4h | |
| Number of drugs per patient | n=213 | % |
| None | 9 | 4.2 |
| 1 | 90 | 42.2 |
| 2 | 75 | 35.2 |
| 3 | 29 | 13.6 |
| 4 | 10 | 4.6 |
| Analgesics used | n=352 | |
| Dipirone | 128 | 36.4 |
| Morphine | 80 | 22.7 |
| Fentanyl | 79 | 22.4 |
| Diclofenac | 38 | 10.8 |
| Remifentanil | 7 | 2.0 |
| Tramadol | 4 | 1.1 |
| Lidocaine | 3 | 0.9 |
| Acetaminophen | 1 | 0.3 |
| Most frequent regimens | ||
| Antipyretic analgesic alone | 45 | 21.1 |
| Strong opioid+antipyretic analgesic | 63 | 29.6 |
| Strong opioid | 42 | 19.7 |
| NSAID+antipyretic analgesic | 10 | 4.7 |
| Tramadol+antipyretic analgesic | 2 | 0.9 |
| Strong opioid+antipyretic analgesic+NSAID | 12 | 5.6 |
| Others | 30 | 14.1 |
Table 3 shows the results of the bivariate analysis that enables a comparison of subgroups of patients with pain control and those with no pain control. It was found that marital status, health insurance regime, education, cigarette smoking, use of alcohol, psychoactive substances, NSAIDS or anti-depressants, surgical risk, use of anesthetic premedication, onset of GI bleeding, nausea and concurrent comorbidities such as diabetes mellitus, ischemic heart disease, depression, epilepsy, COPD, and renal failure were variables with no statistically significant association with the lack of pain control. If was found that gender, vomiting, age between 18 and 44, urban place of residence and the combined use of a strong opioid plus an antipyretic analgesic were variables with a statistically significant association with lack of pain control; and age between 45 and 64 years, urologic or peripheral vascular surgeries, and adherence to the dosing instructions were variables with a statistically significant association with pain control.
Bivariate analysis of pain control at 4h versus the main social, demographic, pharmacological and clinical variables of surgical patients, 2011.
| Characteristics | Pain control at 4h | No pain control at 4h | p* value | RR | 95%** CILower–upper | ||
| Number | % | Number | % | ||||
| Gender | |||||||
| Male | 57 | 57.6 | 42 | 42.4 | 0.005 | 0.460 | 0.267–0.795 |
| Female | 45 | 39.5 | 69 | 60.5 | |||
| Ages | |||||||
| Young adult (18–44) | 36 | 36.4 | 63 | 63.6 | 0.03 | 0.442 | 0.255–0.764 |
| Middle age (45–64) | 39 | 62.9 | 23 | 37.1 | 0.03 | 2.449 | 1.335–4.495 |
| Elderly (65+) | 25 | 48.1 | 27 | 51.9 | 0.769 | 1.099 | 0.586–2.060 |
| Required rescue analgesia | |||||||
| Yes | 2 | 8.0 | 23 | 92.0 | |||
| No | 100 | 53.2 | 88 | 46.8 | <0.001 | 0.079 | 0.018–0.345 |
| Vomiting | |||||||
| Yes | 8 | 27.6 | 21 | 72.4 | |||
| No | 94 | 51.1 | 90 | 48.9 | 0.023 | 0.377 | 0.159–0.894 |
| Place of residence | |||||||
| Urban | 68 | 43.6 | 88 | 56.4 | |||
| Rural | 34 | 59.6 | 23 | 40.4 | 0.028 | 0.505 | 0.273–0.935 |
| Surgical specialty | |||||||
| Urologic | 16 | 94.1 | 1 | 5.9 | <0.001 | 21.0 | 2.735–161.627 |
| Peripheral vascular | 4 | 100 | 0 | 0 | 0.033 | 0.462 | 0.400–0.534 |
| General | 25 | 40.3 | 37 | 59.7 | 0.197 | 0.676 | 0.372–1.228 |
| Orthopedics | 32 | 39.0 | 50 | 61.0 | 0.059 | 0.585 | 0.335–1.023 |
| Obstetrics and gynecology | 10 | 34.5 | 19 | 65.5 | 0.14 | 0.543 | 0.240–1.231 |
| Type of anesthesia | |||||||
| Conductive | 37 | 44.0 | 47 | 56.0 | 0.456 | 0.811 | 0.468–1.406 |
| General intravenous | 10 | 45.5 | 12 | 54.5 | 0.861 | 0.924 | 0.381–2.239 |
| General inhaled | 47 | 51.1 | 45 | 48.9 | 0.327 | 1.310 | 0.763–2.251 |
| Adherence to analgesic dose | |||||||
| Yes | 59 | 48.8 | 62 | 51.2 | |||
| No | 43 | 45.3 | 52 | 54.7 | 0.609 | 1.151 | 0.671–1.972 |
| Adherence to dosing schedule | |||||||
| Yes | 11 | 73.3 | 4 | 26.7 | |||
| No | 88 | 44.5 | 110 | 55.5 | 0.036 | 3.324 | 1.024–10.792 |
| Analgesic regimens | |||||||
| Antipyretic analgesic alone | 24 | 53.3 | 21 | 46.7 | 0.356 | 1.363 | 0.705–2.632 |
| NSAID+antipyretic analgesic | 6 | 60.0 | 4 | 40.0 | 0.407 | 1.719 | 0.471–6.272 |
| Strong opioid+antipyretic analgesic | 23 | 36.5 | 40 | 63.5 | 0.043 | 0.539 | 0.295–0.984 |
| Strong opioid+antipyretic analgesic+NSAID | 5 | 41.7 | 7 | 58.3 | 0.692 | 0.788 | 0.242–2.564 |
| Strong opioid | 22 | 52.4 | 20 | 47.6 | 0.456 | 1.293 | 0.658–2.538 |
In the multivariate analysis, the dependent variable was the lack of pain control and the independent variables were those that showed some significant association in the bivariate analysis. It was found that having an age different from the range between 44 and 64 years (OR: 0.4; 95% CI: 0.148–0.973, p=0.044), living in an urban area (OR: 2.2; 95% CI: 1.135–4.283, p=0.02), and having undergone a procedure other than urologic surgery (OR: 0.05; 95% CI: 0.006–0.4, p=0.005) were the independent variables with a statistically significant association with the lack of pain control.
DiscussionThe importance of adequate management of postoperative pain and the need to set up specialized multi-disciplinary centers with anesthetists, general practitioners and nurses trained in the use of analgesic drugs, and the provision of rigorous pain monitoring and control have been demonstrated in the world literature.14,18 This study found a high prevalence of uncontrolled postoperative pain at 4h, a result that was very different from that found by a meta-analysis of more than 20,000 patients around the world of 11% of cases with postoperative pain, but very similar to Spanish and Colombian publications that report low pain control ranging between 40.0% and 69.3% of postoperative patients assessed.3,19–24 The wide use of drugs as monotherapy, contrary to the ASA guidelines that propose the use of 2 medications with a different mechanism of action at appropriate doses and dosing schedules, may account for the low levels of pain control.14,25,26
The use of dipirone, alone or in combination with opioids, and its association with the lack of pain control is consistent with the results of similar studies conducted in Colombia in which monotherapy was the most widely used with inadequate pain control.19,23 Results of Spanish studies show that the most frequent prescriptions are opioids alone or in association with NSAIDS.20,27 Almost all the patients who required rescue analgesia continued to experience pain, which is evidence of the failure to use more effective analgesia or analgesics at higher doses in patients with very intense pain perception. Some of the international studies have also shown the ineffectiveness of rescue analgesia.19,20
Opioid administration under a suboptimal regimen may be due to the lack of knowledge of the pharmacokinetics of these drugs, and to the fear of adverse reactions. This practice already reported by other authors does not achieve pain relief and maintains the risk of adverse reactions, including delirium in the elderly.20,25,28 It is worth noting that the finding of patients with no analgesic prescription is inconsistent with similar studies in which all the patients received analgesic management. This may be an indication of the indifference of healthcare personnel regarding pain, and lack of knowledge of patient rights.19–22,25,26,29,30
Differences in terms of pain perception and control have already been reported in other studies, and it has been found that males in Spain report more intense pain.23,29 Living in an urban area was associated with lack of pain control when compared with the rural area, something that is not reported in the literature in association with postoperative pain. This relationship that may have cultural components should be explored in more depth.
The specialties performing surgery most frequently at HUSJ were orthopedics, general surgery, obstetrics and gynecology, and it was in those procedures where uncontrolled pain was also more prevalent. Considering that there was greater evidence of uncontrolled pain in orthopedic, general surgery and obstetric and gynecological procedures, they are shown to involve determining factors in pain perception such as extensive tissue damage and the involvement of several systems. It has already been reported that the type of intervention, the surgical technique and the anesthetic management are major determining factors of pain intensity and duration.19,31 In the analysis by type of surgery, it was found that urologic and peripheral vascular surgeries were associated with improved pain control, contrary to the results found by another Colombian study in which those procedures were associated with lack of pain control.19
The main limitations found in this study are due to the fact that, added to the lack of entries in some clinical records, the VAS measures only one dimension as it examines the sensory component only, excluding the patient's affective and cognitive components.20 The wide variety of regimens and drugs used for pain management imposes a limitation on the ability to interpret the results, and highlights the importance of incorporating effective and easy-to-use postoperative pain management guidelines.26
We consider that the lack of postoperative pain control is evident at HUSJ. It is an issue associated with the female gender, the onset of vomiting, age between 18 and 44 years, living in the urban area of the municipality of Pereira or the department of Risaralda, and the combined use of a strong opioid plus an antipyretic analgesic, prescribed at inadequate intervals.
There is a need to revisit pain management in this hospital and make adjustments on the basis of international guidelines, or internally developed guidelines, with a view at ensuring adequate control of acute postoperative pain. This may be accomplished by focusing on the importance of postoperative pain control, and making appropriate use of analgesic medications, in doses and schedules tailored to the needs of individual patients. It would also be important to consider creating an acute pain unit, which has proven to be highly effective in comprehensive patient management and control.3,14,18,32 The use of clinical practice guidelines for adequate analgesic management has been shown to reduce pain and its complications significantly.26
FundingThis research has received funds by the Universidad Tecnológica de Pereira.
Conflicts of interestThe authors declare not to have any conflicts of interest.
Please cite this article as: Machado Alba JE, et al. ¿Estamos controlando el dolor postquirúrgico? Rev Colomb Anestesiol. 2013;41:132–8.