Adverse events are the source of significant care-related morbidity and mortality in surgical patients.
ObjectiveTo characterize and analyze anaesthesia-related adverse events in closed ethical and legal cases, with the involvement of the Colombian Society of Anaesthesia and Resuscitation (Sociedad Colombiana de Anestesiología y Reanimación – S.C.A.R.E.) between 1993 and 2012.
Materials and methodsRetrospective analysis of medical liability cases involving anaesthetists, managed with the support of the Special Fund for Mutual Legal Assistance (FEPASDE).
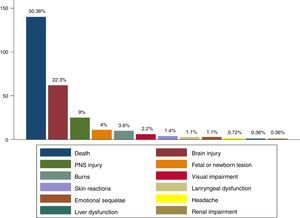
ResultsOverall, 278 proceedings involving anaesthesia-related adverse events were analyzed. The majority (67%) occurred in association with planned surgical procedures (general surgery, orthopaedic surgery, plastic surgery, and obstetrics and gynaecology) performed under general anaesthesia in ASA I patients taken to surgery in Level II complexity settings. A substantial percentage of adverse events (18%) occurred in the Post-Anaesthetic Care Unit (PACU). The most frequent adverse events were cardiovascular and respiratory (55.4% and 36.7% respectively). The most predominant outcomes were death (50.3%) and cerebral insult (22.3%). The analysis found flaws in the completion of the pre-anaesthetic assessment and informed consent forms, compliance with guidelines, standards or protocols, communication with the patient or the family after the event, and communication among the members of the healthcare team.
ConclusionsIn the cases reviewed, the majority of adverse events happened in low risk patients, in low complexity institutions. The PACU was a sensitive setting for the occurrence of adverse events. It is important to consider environmental factors when analysing adverse events.
Los eventos adversos generan una porción considerable de la morbimortalidad asociada a la atención del paciente quirúrgico.
ObjetivoCaracterizar y analizar los eventos adversos asociados a procesos éticos y jurídicos cerrados de anestesiólogos, adelantados por la Sociedad Colombiana de Anestesiología y Reanimación (S.C.A.R.E.) entre 1993–2012.
Materiales y MétodosEstudio retrospectivo que analiza información procesos de responsabilidad médica de anestesiólogos, gestionados por el Fondo Especial Para Auxilio Solidario de Demandas (FEPASDE).
ResultadosSe analizaron 278 procesos con evento adverso relacionado con la anestesia, la mayoría (67%), ocurrieron en procedimientos quirúrgicos programados (en intervenciones de cirugía general, ortopedia, cirugía plástica y gineco-obstetricia), realizados bajo anestesia general, en pacientes ASA I, atendidos en segundo nivel de complejidad. Un porcentaje relevante de eventos adversos (18%) ocurrieron en la Unidad de Cuidados Postanestésicos (UCPA). Los eventos adversos más frecuentes fueron cardiovasculares y respiratorios (55,4% y 36,7% respectivamente). Los desenlaces que predominaron fueron muerte (50,3%) y lesión cerebral (22,3%). Se encontraron fallas en el diligenciamiento de la valoración preanestésica y consentimiento informado, adherencia a guías, normas o protocolos, comunicación con el paciente o su familia posterior al evento y comunicación entre el equipo de salud.
ConclusionesEn los procesos revisados, la mayoría de eventos adversos se presentaron en pacientes de bajo riesgo y en instituciones de bajo nivel de complejidad. La UCPA fue un sitio vulnerable para la presentación de eventos adversos. Es importante considerar factores relacionados con el entorno en el análisis de los eventos adversos.
Since the report “To Err is Human”1 was published, patient safety has been at the forefront in healthcare. Guidelines and standards for application in clinical practice have been developed,2 but many of them are based on low-level evidence because of the sheer impossibility to conduct randomized trials to demonstrate the benefit of a recommendation “universally” considered as necessary. Moreover, the low incidence of some events makes it unfeasible to achieve the necessary sample number required to arrive at sound conclusions. This situation highlights the importance of analysing adverse events (AEs).3,4
Closed claims analysis is a useful method for the study of low-frequency adverse events because it reveals patterns and associated factors amenable to interventions for improving patient safety.5
The World Health Organization has issued an appeal to conduct research on patient safety with the aim of comparing results among countries.6 In Colombia, except for the study by Galindo,7,8 there is no recent research about medical liability proceedings involving anaesthetists, and there are no data about the main reasons for legal action regarding anaesthesia-related adverse events.
The purpose of this research is to characterize and analyze adverse events involved in closed legal claims and ethical proceedings against anaesthetists, managed by the Colombian Society of Anaesthesia and Resuscitation (Sociedad Colombiana de Anestesiología y Reanimación – S.C.A.R.E.) with assistance from FEPASDE between 1993 and 2012, with a view at building recommendations that may result in strategies to reduce AEs in anaesthesia and the associated legal and ethical claims.
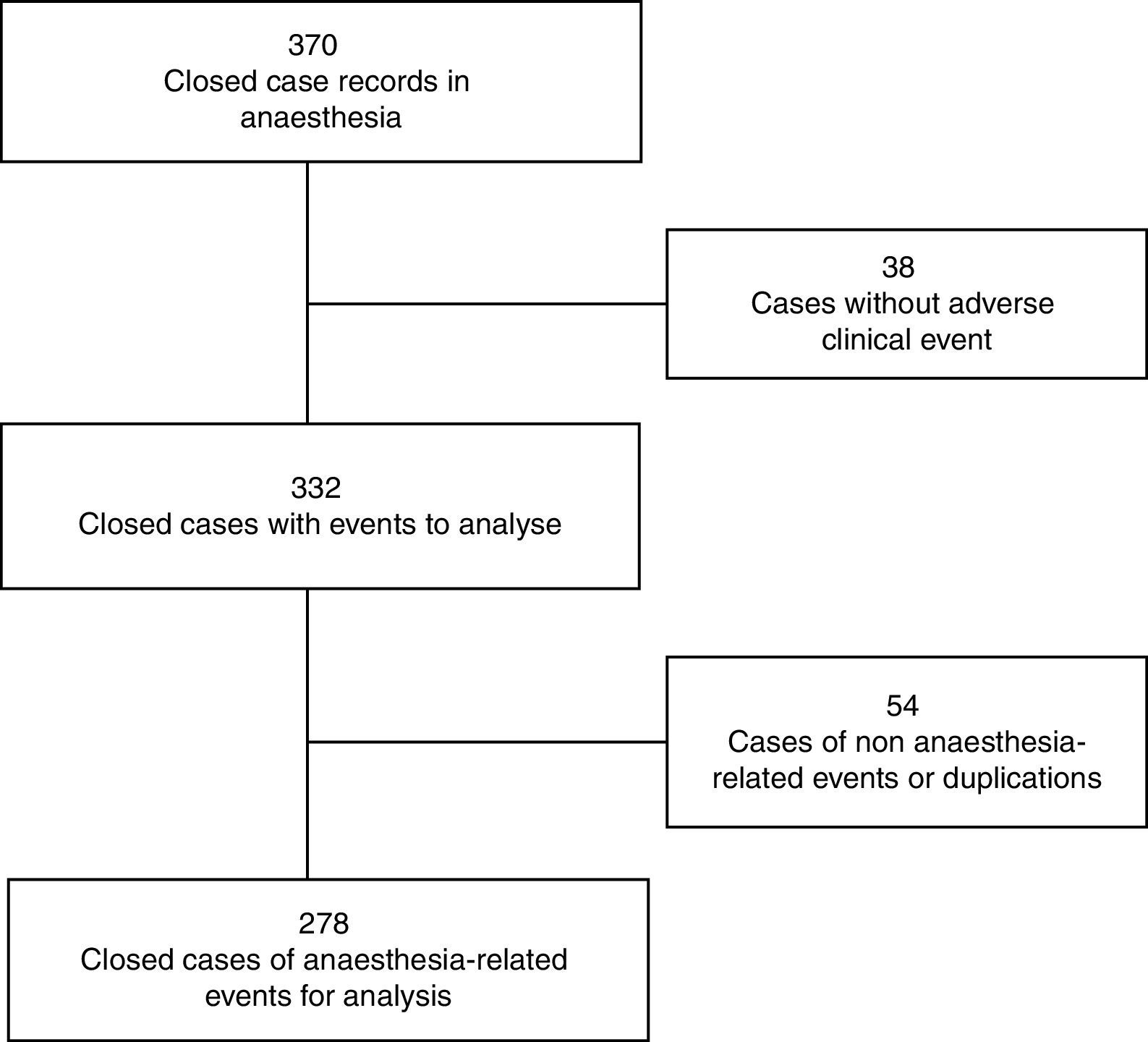
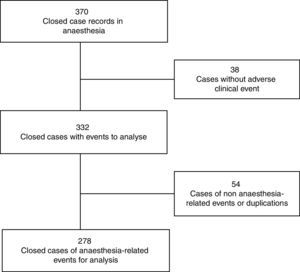
Materials and methodsAnalysis of a retrospective cohort of closed ethical and legal liability cases against anaesthetists who received assistance from FEPASDE between 1993 and 2012. The analysis included all the cases with a ruling in which anaesthesia-related AEs were identified (Fig. 1). A two-phase strategy was designed: definition of guidelines for characterizing AEs based on the framework provided by the International Classification for Patient Safety9; and the analysis of related factors using the model provided by the London Protocol for adverse event analysis.10
Data were extracted using software designed for that purpose. A pilot test was conducted with a group of anaesthetists in order to optimize the wording of the questions, modify unclear items and assess completion time. The cases were rebuilt from the available legal information and were analyzed from the medical standpoint, regardless of the final rulings. Each reviewer was asked to determine if the AEs could have been avoided (in accordance with the score used in the Canadian Adverse Events Study), and to recommend steps to prevent their occurrence.
The data were analyzed using the licenced Stata® software, version 12. Absolute and relative frequencies are reported for categorical variables; mean and standard deviation or median with interquartile range (IQR) are reported for quantitative variables; the Student t test or Mann–Whitney U test were used for quantitative variable comparison and the Chi square or Fisher test for categorical variables, when relevant.
Cases were stratified into two periods: the first between 1993 and 2000 and the second between 2001 and 2012, in order to identify changes in the described characteristics throughout time.
A p value <0.05 was used to establish significance.
ResultsCharacteristics of the patients that suffered anaesthesia-related adverse eventsThe majority of patients were females (66.6%). Half of the patients were between 20 and 44 years of age; 10 patients were under 1 year of age (3.6%) and, of these, 5 were under six months of age. Half of the patients were ASA 1 and 34.4% were ASA 2.
In terms of associated diseases, 181 patients (65.1%) had no comorbidities. Among those who did, the most frequent were blood hypertension, diabetes mellitus, morbid obesity and obstructive pulmonary disease.
Clinical history included prior surgery (30.6%), allergies (6.8%), and difficult airway (3.24%). At the time of the AE, 12.2% (n=34) of the patients were pregnant.
Characteristics of the anaesthetistsFor the anaesthetists, mean age was 44.6 (±10.73) years. At the time of the AE occurrence, 50% were under 43 (IQR 14) while 5% were over 66. The majority of the anaesthetists involved in the AE had training as general anaesthetists (95.9%), 2.6% were subspecialists, and 50% had practiced anaesthesia for more than nine years (IQR 11 years).
In 21% of cases, the anaesthetist in charge of the assessment was not the same giving the anaesthesia. Moreover, there is evidence of change of anaesthetists during the procedure in 22 cases (7.9%).
In 55% of cases, the involvement of other professionals in the AE was evidenced. The surgeon was found to be the person most frequently involved in the event, followed by a different anaesthetist.
Characteristics related to the adverse eventType of procedureOf the total number of events, 91.3% were related to surgical procedures. Non-surgical procedures included pain management (16.6%), cardio-cerebral-pulmonary resuscitation (16.6%), and obstetric analgesia (12.5%).
Although the number of non-surgical procedures is higher for the second time period (after 2001), this difference is not statistically significant when compared to the first time period (p=0.1).
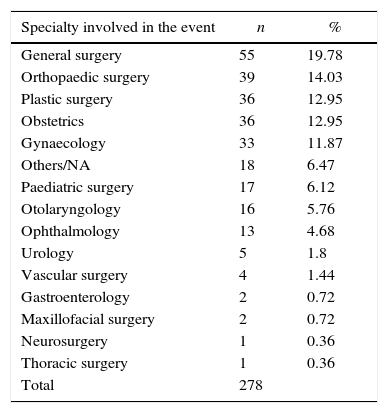
The surgical specialties most frequently associated with the AE were general surgery, orthopaedic surgery, plastic surgery, obstetrics and gynaecology (Table 1); intensive care, as a specialty, was implicated in 18 cases (6.5% of the total).
Specialty involved in the adverse event.
| Specialty involved in the event | n | % |
|---|---|---|
| General surgery | 55 | 19.78 |
| Orthopaedic surgery | 39 | 14.03 |
| Plastic surgery | 36 | 12.95 |
| Obstetrics | 36 | 12.95 |
| Gynaecology | 33 | 11.87 |
| Others/NA | 18 | 6.47 |
| Paediatric surgery | 17 | 6.12 |
| Otolaryngology | 16 | 5.76 |
| Ophthalmology | 13 | 4.68 |
| Urology | 5 | 1.8 |
| Vascular surgery | 4 | 1.44 |
| Gastroenterology | 2 | 0.72 |
| Maxillofacial surgery | 2 | 0.72 |
| Neurosurgery | 1 | 0.36 |
| Thoracic surgery | 1 | 0.36 |
| Total | 278 |
Two thirds of the AEs (67.2%) were associated with planned procedures (with or without hospital admission), and only one third with emergency procedures (32.8%).
In 68% of the cases, AEs were associated with surgical procedures lasting less than 3hours, almost half of them being less than one hour long.
Of the procedures, 56% were performed under general anaesthesia, 35.6% under regional anaesthesia (including neuroaxial anaesthesia and blocks). In 13 cases (4.68%), there was an unplanned change of anaesthetic technique.
Although the number of claims associated with general anaesthesia dropped during the second time period (2001–2012) and there was an increase in the number of claims due to catheter epidural anaesthesia, differences between these two time periods are not statistically significant (p=0.076).
There was a substantial percentage (ranging between 47% and 87.5%) of unrecorded data for conductive anaesthesia in relation to the number of punctures, needle calibre or catheter size.
The frequency of AEs associated with anaesthetic blocks is low (5.4% of cases), the most common being interscalene block (26.7%), peribulbar block (20%) and supraclavicular block (13.3%). The clinical method for localizing and placing the block was the predominant method when compared with others (nerve stimulation and ultrasound). There is a high percentage of unrecorded data regarding the technique (41.7%).
Supine decubitus was the predominant position (75.2%), followed by prone decubitus (3.6%), gynaecological position (3.24%) and lateral decubitus (2.9%). Intraoperative position changes were documented in 15 cases (mainly in plastic surgery) and in 4 of them, the AE occurred immediately after the change in patient position.
Events were classified in accordance with the specific physiological systems affected, the most frequently affected being the cardiovascular (55.4%) and respiratory systems (36.7%).
The predominant cardiovascular AE was cardiac arrest in 55.4% of all cases, accounting for 82.5% of all cardiovascular events; a large difference was found in terms of the frequency of other events (bradycardia 1.4%, hypotension 10.1%, and shock 9.3%).
Among respiratory AEs, respiratory depression (14%) and hypoxaemia (13.3%) were the most frequent. Frequency of airway-related cases was under 4% for all potential occurrences.
The most frequent events related with the central nervous system were seizures (38%). There were three cases of meningeal involvement (one with a diagnosed infection). No cases of intraoperative awakening were documented. Of events associated with the peripheral nervous system, 82% were cases of neuropathy or peripheral nerve injury.
Adverse drug reactions accounted for 3.6% of all cases and 25% of drug-related AEs. In 17%, either a medication dose or type error is documented. There were no cases associated with blood product transfusions, although there was one near miss (with no adverse event) associated with the wrong application of red blood cells.
The most important equipment-related AE was electrocautery burn, found in 9 cases (60%), two of which had skin sequelae. Malfunctioning of the anaesthetic gas system was described in two cases as a result of central problems in one, and anaesthesia machine failure in the second one.
The majority of unplanned ICU admissions were due to post-resuscitation conditions (47%), followed by haemorrhagic shock (11%), severe bradycardia (7%), neurologic deterioration (7%), and respiratory depression (5%). For each category of severe bronchospasm, pulmonary oedema, aspiration or other complications, the frequency of admission to the ICU was less than 4%.
Comparison by time period showed an increase in the proportion of cardiovascular and respiratory AEs for the second time period (from 2000 to 2012) and a reduction in central nervous system AEs; however, there was no statistically significant difference for any of them. While an increase in drug-related and regional anaesthesia-related cases of AEs was observed, there was a reduction in equipment-related cases.
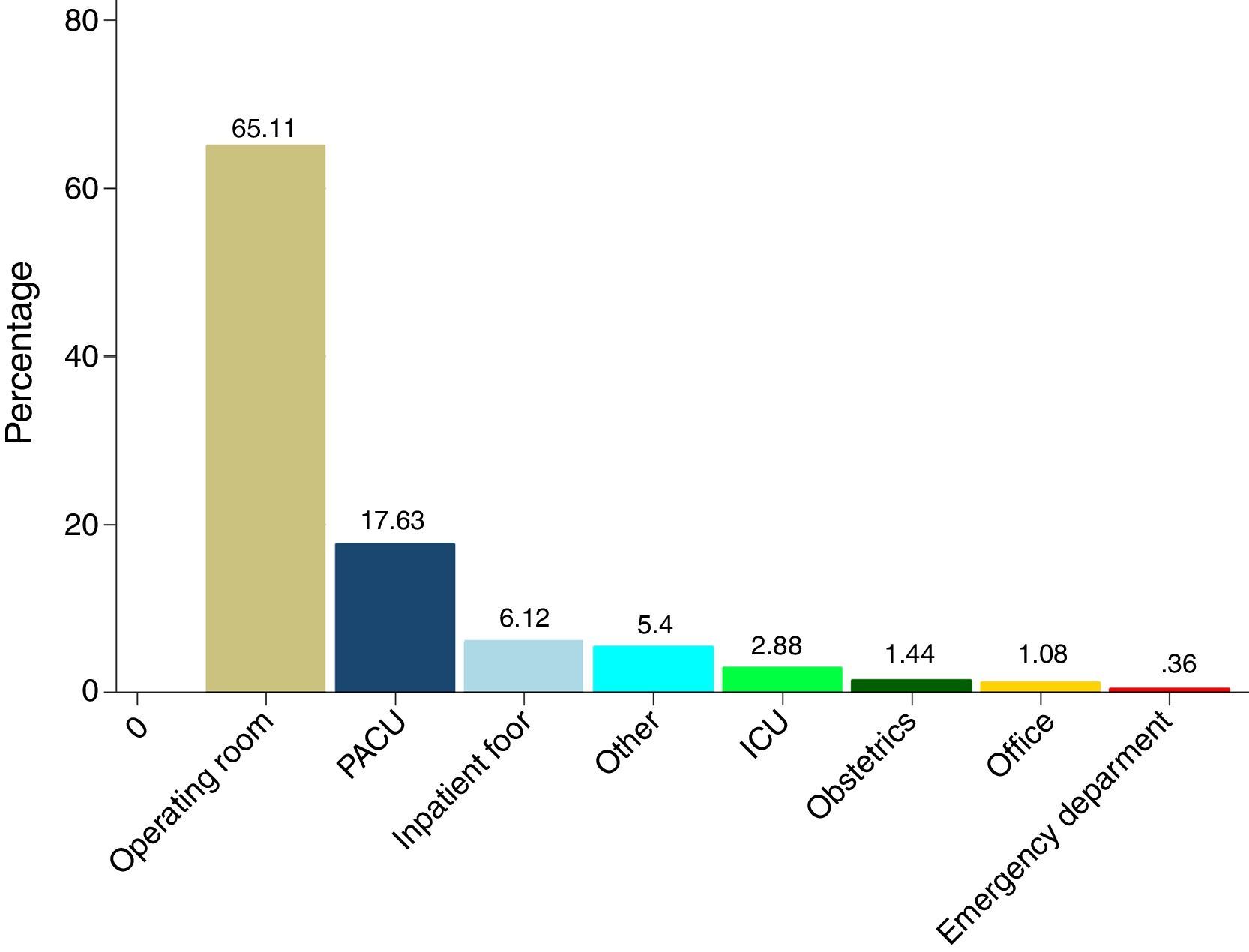
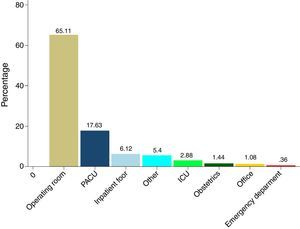
Temporal and spatial characterization of the eventsThe majority of AEs took place in the operating room (Fig. 2), with 45% mortality; an important percentage of adverse events (17.6%) occurred in the Post-Anaesthetic Care Unit (PACU), with 50% mortality. There were four cases in the obstetrics area, with fatal outcomes in three.
Regarding the time of the day, 70.5% of the AEs took place during the day, 40% in the morning (7 a.m. to 1 p.m.).
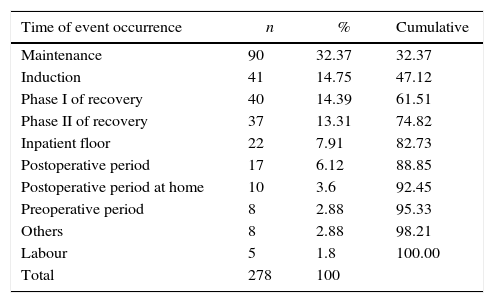
Regarding the timing of the occurrence, adverse events were more frequent (32.3%) during maintenance of anaesthesia (Table 2).
Time of adverse event occurrence.
| Time of event occurrence | n | % | Cumulative |
|---|---|---|---|
| Maintenance | 90 | 32.37 | 32.37 |
| Induction | 41 | 14.75 | 47.12 |
| Phase I of recovery | 40 | 14.39 | 61.51 |
| Phase II of recovery | 37 | 13.31 | 74.82 |
| Inpatient floor | 22 | 7.91 | 82.73 |
| Postoperative period | 17 | 6.12 | 88.85 |
| Postoperative period at home | 10 | 3.6 | 92.45 |
| Preoperative period | 8 | 2.88 | 95.33 |
| Others | 8 | 2.88 | 98.21 |
| Labour | 5 | 1.8 | 100.00 |
| Total | 278 | 100 |
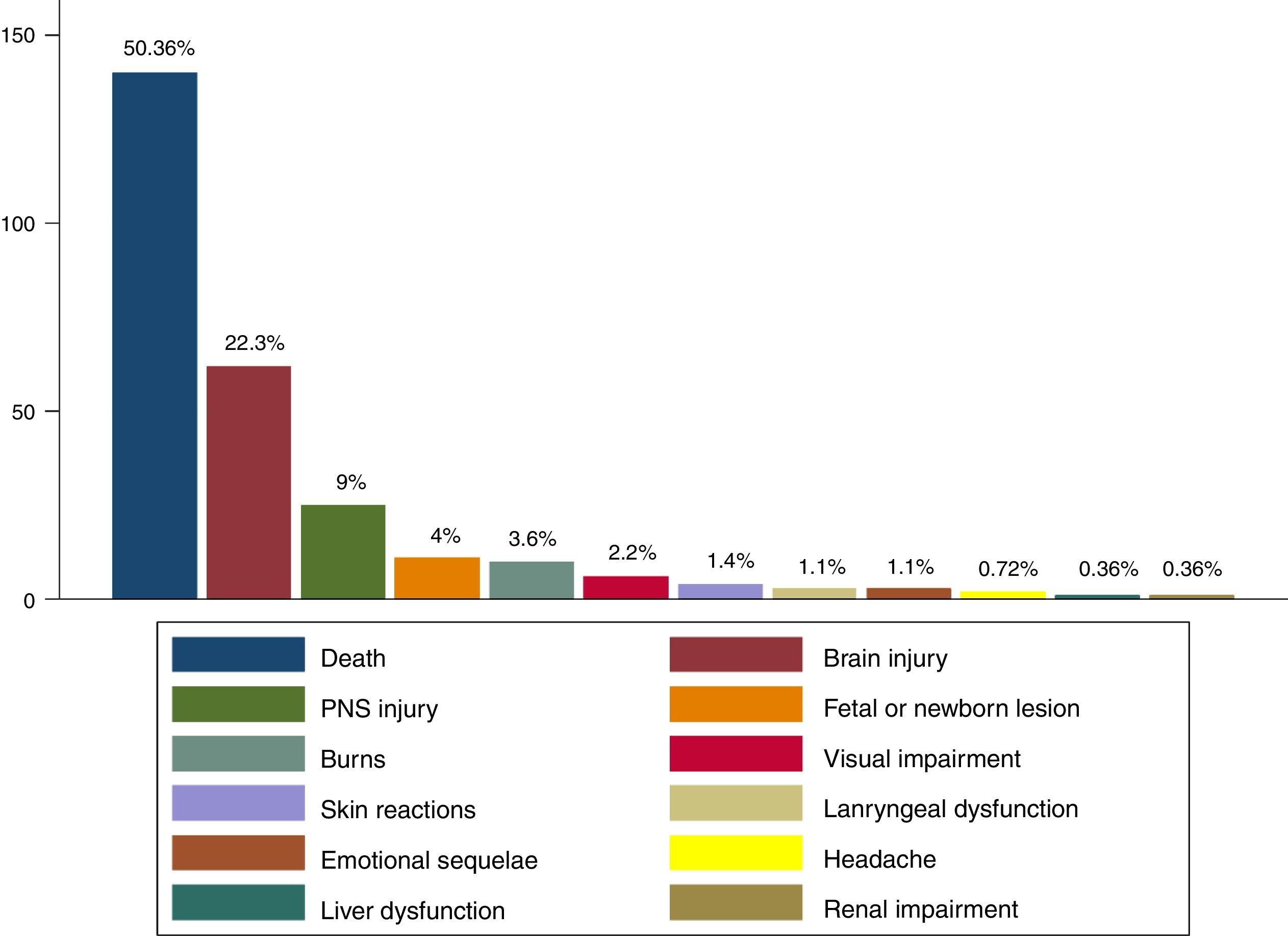
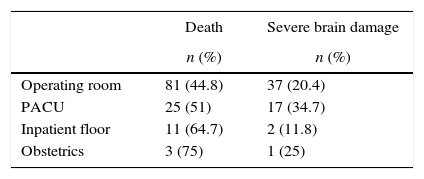
Death was the main outcome among all anaesthesia-related AEs (Fig. 3), and was found to have occurred in 51% of the events that took place in the PACU (Table 3). Of the brain injuries, 77% were severe.
Other factorsThe clinical record and the informed consent were evaluated for completeness. Adequate quality entries were found only in half of the clinical records. Flaws were found in one fourth of the cases for each form of documentation.
Communication deficiencies among the members of the health team were identified in 17% of cases and, overall, patient communication was documented in 8.3% of cases. In contrast, records of communication with the family or the patient after the event were found in 43.5% of cases.
It was considered important to assess the occurrence of administrative errors, and these were demonstrated to be present to some degree in 26% of cases.
Lack of adherence to standards, guidelines or protocols was found in 42.5% of cases. Specifically for minimal safety standards for the practice of anaesthesia, non-adherence to the standards effective at the time was identified in 30.2% of the cases of adverse events.
AEs were considered preventable in 38.5% of cases (n=107). In 27 of these cases, the recommendation consisted of adequate pre-anaesthesia assessment focused on risk prevention, and a thorough assessment by the attendant surgeon; in 17 cases, the recommendations required improved patient monitoring and care in the PACU, including admission with a better Aldrete score, and the presence of an anaesthetist in the recovery room; in 14 cases, the recommendation required the adoption of, and adherence to, guidelines, standards or management protocols.
DiscussionSince the report “To Err is Human”1 was published, patient safety has become a key concept in healthcare. The social and financial impact caused by healthcare-related injuries was described in that report. This analysis found a significant percentage of patients in their productive years who required treatment and rehabilitation, resulting in additional cost for the system, not to mention the disability and the number of years of healthy life lost.
Although there are different methods for studying AEs,11–13 specifically in anaesthesia, where the frequency of certain complications is low, cohort studies are not very feasible, and self-reporting systems for AEs are seldom used.
Despite its limitations, the study of closed claims is a cost-effective way to gather information about anaesthesia-related events. It is a method that provides important information regarding complications and their associated factors, as demonstrated by the ASA Closed Claims Project.5
This study found that anaesthesia-related AEs are more frequent in patients considered low risk, with little or no comorbidity, receiving care in low complexity institutions. Although confirmed in other reports,14,15 this finding reinforces the appeal to maintain care standards for patients and procedures in settings conducive to a false sense of confidence regarding a low probability of perioperative complications.
The majority of procedures associated with claims are planned surgeries, despite the fact that emergency procedures imply a higher risk of complications and adverse events. This phenomenon has been documented in other publications as well.16 A potential explanation, besides the growth and increased complexity of outpatient surgery, is a higher state of awareness of potential complications in emergency procedures on the part of the anaesthetists as well as of patients and families. However, lower adherence to standards of care because of the low-risk perception regarding these procedures could play a relevant role.
Regarding the age of the anaesthetists involved, the rate of claims against less experienced or older anaesthetists is not higher (as may have been expected), something already described by Galindo.8
Although not as marked as in the ASA closed claims study,14 the increasing number of claims related to non-surgical procedures may account for a growing activity of anaesthetists outside the operating room, in areas such as pain management, intensive care units, obstetric analgesia and monitored anaesthetic care. Consequently, an increase in the number of claims in those settings is to be expected.
In this study, the frequency of events associated with massive bleeding is low, unlike the findings of the ASA closed case study, where it was the most frequent cardiovascular event.14,17
Respiratory depression and hypoxaemia appear as the most common respiratory events, in contrast with the information available from ASA where the most common events associated with the respiratory system were difficult intubation, inadequate ventilation and aspiration.14
In the temporal and spatial analysis of the event, the PACU emerges as a sensitive setting for the occurrence of adverse events, emphasizing that mortality in those cases is higher (54% mortality for events occurring in the recovery room or in postoperative inpatient floors), a finding that is consistent with other reports.18,19 Critical processes have been identified in the recovery room, including patient handover from the operating room,20,21 workload, and training of the nursing staff.22 A recent observational study conducted in Europe reports higher mortality in units staffed with nurses with less training and a larger number of patients to care for.23
Compared to the American closed claims analysis, the main outcomes, though similar in terms of ranking, are higher in frequency of occurrence (the percentage of deaths over the total number of claims was 26% and 50% for the ASA study and for this series, respectively). This implies a more serious final outcome for the adverse events, giving rise to questions about the factors that are behind this behaviour and which may be the subject for further research.
The analysis of environment-related factors shows frequent failure on the part of the healthcare staff to adhere to guidelines, standards and protocols, as has been described in the Australian study.15 There are also noticeable flaws in communication between the healthcare staff and the patient and/or family during the preoperative as well as the postoperative period. These factors have already been described as potential contributors to adverse events24 and malpractice lawsuits.25 Moreover, for specific settings like the PACU, deficient communication processes have been identified during patient handover.26 Emphasis has been made on the importance of communication within the framework of teamwork as an essential component for safety in the operating room,27 as well as on effective intervention strategies designed to improve teamwork in the operating theatre and in the setting of obstetrics.
In terms of administrative processes, the most common situation was the delay in performing the procedure or referring the patient to another level of care (generally to the ICU). Another frequent situation is related to the types of hiring practices for healthcare staff.
This study has limitations because of its retrospective nature. The clinical records being the source of information, it was not possible to obtain data regarding certain topics, for example regional anaesthesia. Additionally, closed claims analysis must be interpreted carefully. The frequencies reported do not represent incidence or prevalence, and cannot be extrapolated to the general population, given the lack of information about the total number of events and the total number of anaesthetic procedures. Moreover, there is bias towards more serious or catastrophic events, which have a higher probability of resulting in legal claims.
ConclusionsConsistent with the literature, the processes analyzed in our setting illustrate a situation in which the majority of events occur in patients and conditions considered low risk.
Although the place with the higher frequency of events is the operating room, the post-anaesthetic care unit is a highly sensitive setting, with the added issue of a higher rate of catastrophic outcomes.
Emphasis is made on the need to improve communication processes among the members of the healthcare staff and between them and the patient, an on the need to follow standards, guidelines and protocols.
The information derived from this study gives rise to new questions for research and a need for a more detailed analysis of specific outcomes (cardiac arrest) or specific patient groups (obstetric/paediatric population) with a view at obtaining additional information and identifying risk factors that warrant intervention.
Ethical responsibilityThe authors declare that this research was conducted in accordance with the ethical principles of the Helsinki Declaration, the World Medical Association and Resolution 8430 of 1993, and was reviewed by the bioethics committee.
Confidentiality of the dataThe authors declare that protocols on the disclosure of patient information were abided by.
FundingColombian Society of Anaesthesia and Resuscitation (Sociedad Colombiana de Anestesiología y Reanimación- S.C.A.R.E.).
Conflict of interestThe authors declare not having any conflict of interest.
Please cite this article as: Bocanegra-Rivera JC, Arias-Botero JH. Caracterización y análisis de eventos adversos en procesos cerrados de anestesiólogos apoderados por la Sociedad Colombiana de Anestesiología y Reanimación (S.C.A.R.E.) en Colombia entre 1993–2012. Rev Colomb Anestesiol. 2016;44:201–208.