Objective: Description of a case of respiratory depression during the late post-operative period in an obstetrics patient who received regional subarachnoidal anesthesia using a local anesthetic and intrathecal morphine.
Methods: The clinical case review, during the monthly review meeting at the Anesthesiology Unit of the National University of Colombia, discusses a clinical case of interest, in accordance with a sequence of topics, e.g.: third delay, when the patient is admitted and the clinical history is taken; fourth delay, when the patient is scheduled for surgery and the anesthesiologist performs the pre-anesthesia assessment, including the anesthetic evaluation and management, monitoring analysis, potential complications and their management, etc.
Result: Each case must generate a clinical discussion based on evidence in the literature and must be part of a competencies approach, including knowledge, know-how and communication skills. This particular case illustrates a sequence of errors that resulted in incidents and even adverse events. The physical evaluation and the considerations pertaining to the anesthetic and surgical procedures must be carefully recorded in the anesthesia record. Likewise, it is important to foresee conditions such as respiratory depression, which is one of the side effects of opioid administration and requires close monitoring and appropriate management.
© 2012 Sociedad Colombiana de Anestesiología y Reanimación. Published by Elsevier. All rights reserved.
Objetivo: Describir el caso de depresión respiratoria en el período postoperatorio tardío, el cual se dio en una paciente obstétrica, quien recibió anestesia regional subaracnoidea con anestésico local y morfina intratecal.
Métodos: Discusión de un caso clínico. La secuencia del caso, durante la revisión del servicio mensual en la unidad de Anestesiología de la Universidad Nacional de Colombia, requiere de diferentes discusiones en la medida en que se pasa de un tema de revisión a otro, verbigracia: tercera demora, cuando la paciente ingresa y se le realiza la historia clínica; cuarta demora, cuando se programa para cirugía y el anestesiólogo realiza la valoración preanestésica, las consideraciones de evaluación y manejo anestésico, el análisis de la monitoría, la anticipación a las complicaciones, el manejo de las mismas, etc.
Resultado: Cada caso debe propiciar la discusión clínica sustentada en la literatura y debe hacer parte de las competencias en el saber y el saber hacer, ser y comunicar. Este caso particular ilustra una secuencia de errores cometidos, los cuales desembocan en incidentes e incluso en eventos adversos. La evaluación física, las consideraciones del procedimiento anestésicoquirúrgico, así como los datos de la monitoría, deben ser consignados rigurosamente en el registro anestésico. De la misma manera, hay que prever condiciones como la depresión respiratoria, uno de los efectos colaterales de los opioides, el cual requiere de una vigilancia estrecha y un manejo apropiado.
© 2012 Sociedad Colombiana de Anestesiología y Reanimación. Publicado por Elsevier. Todos los derechos resevados.
Twenty-four year-old female seen on March 19, 2011 because of pain in the right iliac fossa of one day of evolution, associated with small vaginal bleeding. The pelvic ultrasound report included heterogenous fluid in the pelvic cavity, a right adnexal mass, right ovarian cyst rupture versus right ectopic pregnancy. The patient was referred to a Level II hospital where she was admitted with no symptoms.
The patient did not report urinary symptoms, fever or general malaise on systems review. Positive history findings included a C-section performed 10 years before because of unfavorable cervix, menarche at 11 years of age, regular 30-day cycles lasting 3 days, last menstruation on February 28, 2011, and date of the last delivery December 31, 2000, with the following obstetrical diagnosis: Gravida 1, Para 1, Live birth 1, C-section 1.
On physical examination, the patient was in good general condition, with a blood pressure of 134/72 (mean of 97), heart rate 110 per minute, respiratory rate 18 per minute, ambient oxygen saturation 94%, body temperature 37°C. The patient reported pain on palpation in the right iliac fossa, but there was no defensive muscle reaction or signs of peritoneal irritation, and Blumberg's sign was negative. The finding on vaginal palpation was a central closed cervix with no pain on mobilization.
A pregnancy test came back positive, leading to the request for a BHCG test in order to assess the viability of the pregnancy and determine the need to admit the patient. The result of the BHCG test came back on the next day at 352.5 mIU/ml (in non-pregnant women, values are under 5 mIU/ml), consistent with a four-week pregnancy. A new transvaginal ultrasound was performed and three hours later the patient reported abdominal pain with mild genital bleeding.
Vital signs after that finding were the following: blood pressure 109/60, heart rate 73 per minute, respiratory rate 20 per minute, oxygen saturation 97%. The patient showed signs of peritoneal irritation on abdominal palpation and evidence of scarce, non-fetid hematic lochia. The ultrasound revealed a right ruptured ectopic pregnancy that resulted in the decision to perform a laparotomy.
DiscussionThe obstetric and gynecology service should have considered the possibility of finding an ectopic pregnancy on the initial ultrasound, given the risk of rupture of this lesion, which then became evident on ultrasound. Upon admission, it was considered that the patient required hematocrit or hemoglobin (Hb) assessment due to the probability of intra-abdominal bleeding. However, some of the professors were of the opinion that this test was not important and decided to ask for blood products and proceed with an emergency surgery. The consensus conclusion regarding this point was that laboratory tests (Hb or Hct) should have been done due to the patient's clinical status and the possibility of potential complications.
Expectant medical management of this condition must follow established clinical criteria, and the decision on the therapeutic approach is up to the treating specialist only.1 Aside from the clinical assessment, it is important to perform all the laboratory tests required in order for the anesthetist to approach in a comprehensive manner.2
The second issue that lends itself to discussion in this case is the pre-anesthetic assessment, which resulted in the following information:
- -
Surgical pathology: ectopic pregnancy.
- -
Anesthetic and surgical history: uncomplicated C-section under regional anesthesia.
- -
Obstetrics history: Gravida 2, Para 1, C-section 1.
- -
Full stomach: no.
- -
Physical examination: Blood pressure 134/72, heart rate 84 per minute, respiratory rate 20 per minute. Good general condition. Short cervix: no. Mental-thyroid distance >6 cm. Cardiopulmonary: no abnormalities. Abdomen: soft, increased uterine size, ASA 2.
The diagnosis did not consider the fact that the ectopic pregnancy had already been classified as ruptured, meaning that both the physical status and the surgical risk classifications were necessarily higher and, consequently, the selected anesthetic plan could have changed. On the other hand the ASA nomenclature in Roman numerals was wrong.3 As an abdominal-pelvic disease, the classification should have been considered as a full stomach;4 moreover, the fasting period was not recorded, although the time elapsed between the decision to operate and the pre-anesthetic assessment in the operating room was 8 hours. No record was found of a complete airway assessment, and in the context of an emergency case, had general anesthesia been required, the unpredictability of any necessary measures would have been high given the risk of finding a difficult airway.5
The consensus regarding this aspect was to classify the status as ASA 3U.
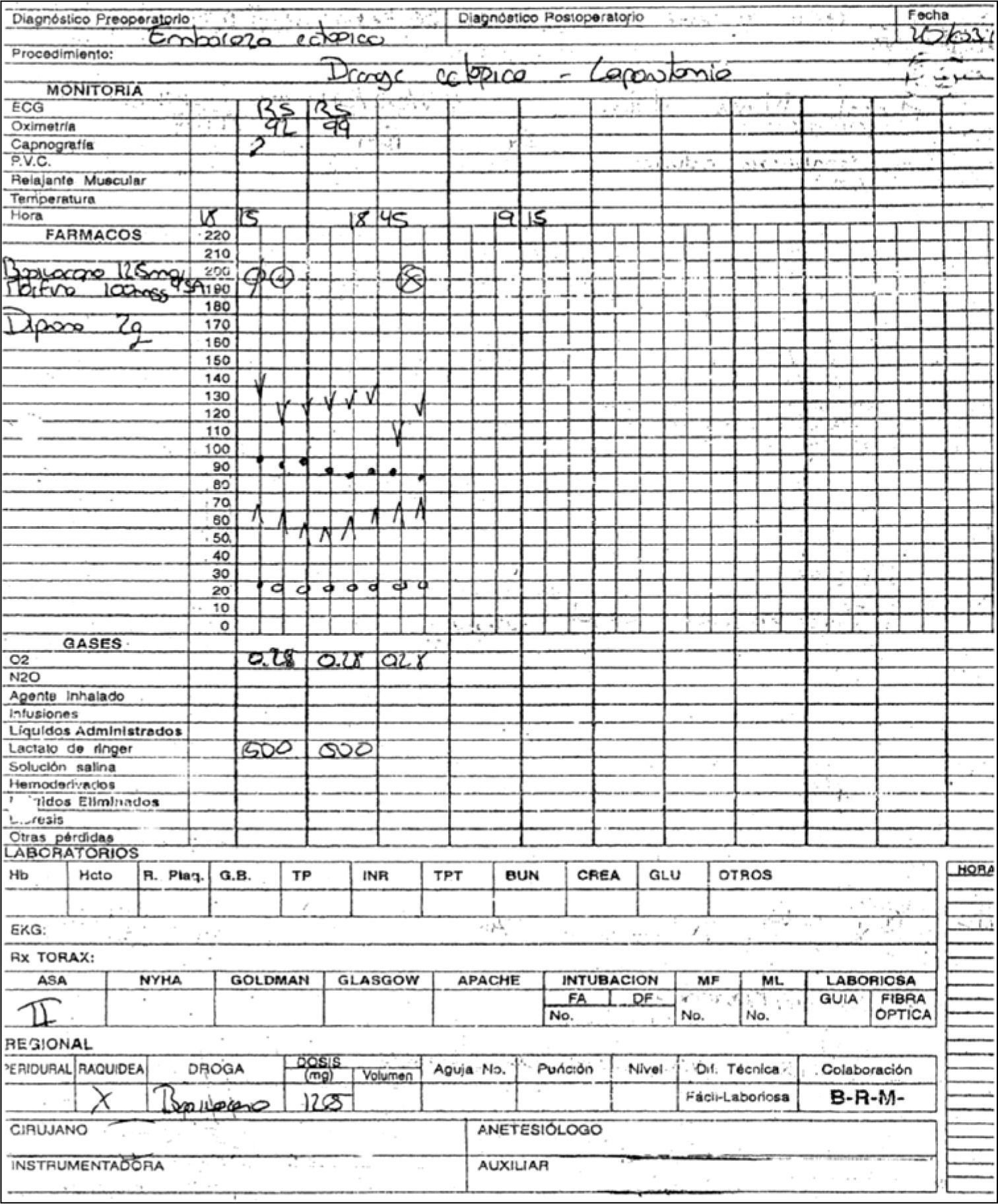
Regarding the anesthetic management, the following was noted: The decision was made to use the regional subarachnoid technique. Following L3-L4 asepsis and antisepsis, a single puncture was performed yielding a crystal clear fluid, after which the patient was given 12.5 mg of bupivacaine and 100 μg of morphine, providing an adequate level of anesthesia (table 4, fig. 1. Anesthesia record).
The patient was hemodynamically stable during surgery and received dipyrone 2 g IV for analgesia.
A ruptured ectopic pregnancy with 200 ml of blood in the cavity was found during surgery, resulting in an uncomplicated resection. Afterward, the patient was moved to the recovery room with residual motor block and pain under control.
Two 14 or 16 gauge IV lines were not secured at the start of the procedure. The anesthetic plan did not consider the risk of bleeding according to the pathology (hemoperitoneum) or the procedure-related risk which, together with the high sympathetic block, increased the probability of hemodynamic involvement.
Despite the fact that the literature does not offer sufficient evidence regarding this type of pathology in order to help select one anesthetic technique over another,6-10 the Anesthesia Unit has always considered, by protocol, that general anesthesia is the safest technique in cases of ruptured ectopic pregnancy with a risk of hemodynamic compromise.
Two hours after the procedure, the patient was hemodynamically stable with a blood pressure of 112/60 (mean of 78), heart rate of 80 per minute, heart rate 16 per minute, oxygen saturation 96%, with no signs of systemic inflammatory response or apparent bleeding. Consequently, she was transferred to the ward with and order for analgesic management consisting of 2 g of dipyrone every 6 hours, diclofenac 75 mg IM every 12 hours, normal diet and periodic monitoring for bleeding and vital signs.
Ten hours after transfer, the patient was found unconscious, cyanotic, diaphoretic, hypotensive, bradycardic and in very bad general condition, blood pressure 90/45, heart rate 94 per minute, respiratory rate 0 per minute, oxygen saturation 78% and body temperature of 35 °C. The Glasgow score was 3/15, and additional findings included cyanotic mucosal tissues, abundant oropharyngeal secretions, symmetrical pulses, absent respiratory work, tachycardic heart sounds, and no murmurs.
The surgical wound was covered with clean dressings and external genitalia showed no evidence of active bleeding.
Placement of a urinary catheter yielded clear urine and the patient was taken to the operating room for resuscitation by the anesthesiologist on call. Controlled manual ventilation was started after suctioning for secretion removal, together with intravenous fluid infusion. The patient responded with spontaneous breathing and improved consciousness.
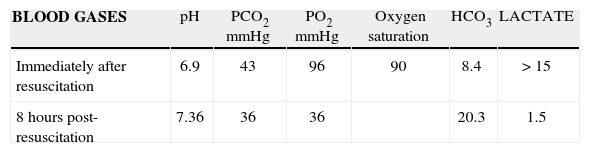
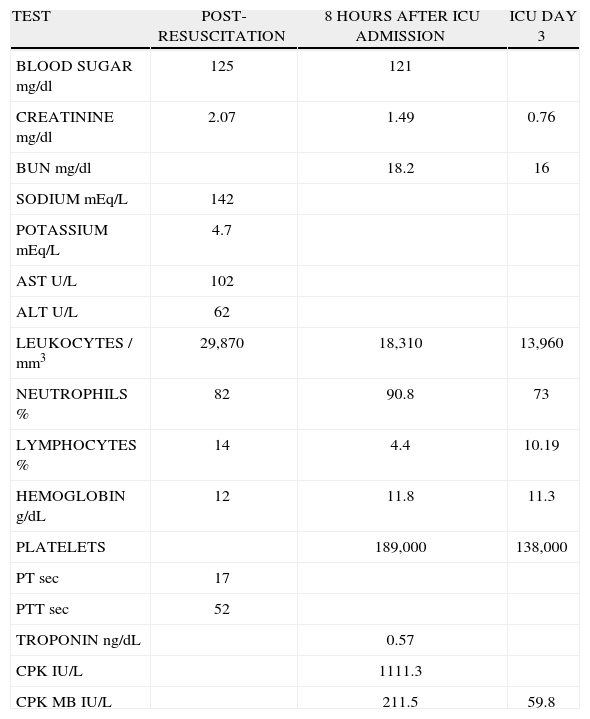
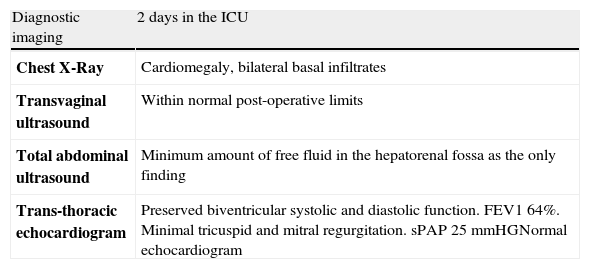
Blood gases were consistent with metabolic acidosis and severe hyperlactatemia (table 1). The patient was transferred to the Intensive Care Unit where she recovered satisfactorily, with improvement of the acidosis and a reduction of lactate levels and no oxygenation, ventilation or electrolyte disorders. Pulmonary thromboembolism (PTE), massive bleeding or infection were ruled out; an increase in urea and creatinine was documented, with a return to normal after two days (tables 2 and 3).
Evaluation of para-clinical tests
| TEST | POST-RESUSCITATION | 8 HOURS AFTER ICU ADMISSION | ICU DAY 3 |
| BLOOD SUGAR mg/dl | 125 | 121 | |
| CREATININE mg/dl | 2.07 | 1.49 | 0.76 |
| BUN mg/dl | 18.2 | 16 | |
| SODIUM mEq/L | 142 | ||
| POTASSIUM mEq/L | 4.7 | ||
| AST U/L | 102 | ||
| ALT U/L | 62 | ||
| LEUKOCYTES / mm3 | 29,870 | 18,310 | 13,960 |
| NEUTROPHILS % | 82 | 90.8 | 73 |
| LYMPHOCYTES % | 14 | 4.4 | 10.19 |
| HEMOGLOBIN g/dL | 12 | 11.8 | 11.3 |
| PLATELETS | 189,000 | 138,000 | |
| PT sec | 17 | ||
| PTT sec | 52 | ||
| TROPONIN ng/dL | 0.57 | ||
| CPK IU/L | 1111.3 | ||
| CPK MB IU/L | 211.5 | 59.8 |
Para-clinical tests in the ICU
| Diagnostic imaging | 2 days in the ICU |
| Chest X-Ray | Cardiomegaly, bilateral basal infiltrates |
| Transvaginal ultrasound | Within normal post-operative limits |
| Total abdominal ultrasound | Minimum amount of free fluid in the hepatorenal fossa as the only finding |
| Trans-thoracic echocardiogram | Preserved biventricular systolic and diastolic function. FEV1 64%. Minimal tricuspid and mitral regurgitation. sPAP 25 mmHGNormal echocardiogram |
After four days in the ICU, the patient was discharged with no medications, considering that she had been treated for a severe post-operative hypoxic condition that had responded to ventilation management and had left no sequelae.
Considerations during the immediate post-operative period focused on the monitoring of vital signs. No order sets were specified and no records were found over a 10-hour period in the nursing notes. Blood gas measurements were done after airway management and ventilation support, which could explain the moderately low PCO2.
Elevated lactate values could have been secondary to a relative hypovolemic status in a patient undergoing a C-section under regional anesthesia and who received 1000 ml of Ringer's lactate intraoperatively (see anesthesia record), with no information concerning fluid management during the post-operative period. This explanation is supported by the finding of hypotension and tachycardia during the episode of respiratory depression in a patient who was found to have elevated urea and creatinine values in the ICU. Considering that intrathecal morphine migrates rostrally and may give rise to respiratory depression even after 18 hours of administration,11, 12 the recommendation is to reserve its use only to healthcare settings with pain management services or, in their absence, under explicit orders of the anesthetist for respiratory rate monitoring according to a specific schedule.13
The decision to place the urinary catheter before tending to the respiratory depression, and to transfer the patient under respiratory arrest so that she could receive assistance from a "specialist" without following the resuscitation guidelines is quite striking, considering that the guidelines emphasize the implementation of the chain of survival right at the site of the event.14, 15
Transfer to the intensive care unit is the fifth link in the chain of survival and is designed to provide a comprehensive assessment and rule out other differential diagnoses for opioid-related respiratory depression, even more so when cardiac enzyme (CPK) levels may suggest not only myocardial tissue injury but also renal, pulmonary, muscle and other tissue involvement, as a result of prolonged hypoxia.16, 17
Respiratory depression following neuroaxial morphine administration is bi-phasic: it may be early, occurring within 30 to 90 minutes after administration, probably as a result of systemic absorption, or late, within 6 to 18 hours due to rostral dissemination (given its hydrophilic characteristics) to the cerebrospinal fluid and the brainstem.11 The incidence rate described in the literature varies and ranges between 0% and 0.9%: Kotelko et al. report no cases in 276 patients receiving 5 mg epidurally; McMorland et al. report an incidence of 0.07% in 3,000 patients; Fuller et al. report 0.25% in 4,480 patients using epidural doses ranging between 2 mg and 5 mg; Leicht et al. found an incidence of 0.4% in 1000 patients receiving an epidural dose of 5 mg; Abouleish et al. (who define respiratory depression from the moment oxygen saturation drops below 85% and respiratory rate is less than 10 breaths/minute) report a 0.9% incidence in 856 patients with intrathecal administration of 200 μg;11, 12 and, finally, Shapiro et al. report and incidence of 0.26% in 1,524 patients with epidural morphine.18
ConclusionThis case illustrates the importance of clinical monitoring of patients from the moment of admission, and of identifying risk factors, classifying the physical status, and assessing the risk-benefit balance in order to implement the best anesthetic and surgical management, and ensure the most adequate outcome after anesthesia, particularly in patients exposed to neuroaxial opioids. These pharmacological agents are extremely valuable for multimodal post-operative pain management, but they may produce severe side effects, such as respiratory depression.
Competing InterestsNone declared.
Funding sources: The authors' own resources.