The classical approach to evaluate the correction of the tetralogy of Fallot (TOF) consists in calculating the ratio between the right systolic and systemic pressure; however, with the advent of transesophageal echocardiography, new approaches have been developed.
We shall present a case of a 15-year-old patient with TOF who underwent correction and the management was based on the intraoperative echocardiography.
We will also address the role of the echocardiographic parameters in the evaluation of the correction of the TOF.
La forma clásica de evaluación de la corrección de la tetralogía de Fallot (TDF) consiste en el cálculo de la relación entre las presiones sistólica ventricular derecha y sistémica. Sin embargo, el advenimiento del ecocardiograma transesofágico ha desarrollado nuevos enfoques al respecto.
Presentaremos el caso de un paciente de 15 años con TDF el cual fue llevado a corrección, y cuyo manejo se basó en el ecocardiograma intraoperatorio.
También discutiremos el papel de los parámetros ecocardiográficos en la evaluación de la corrección de la TDF.
Transesophageal echocardiography has become an invaluable tool to the cardiovascular anesthesiologist because it provides detailed information about the anatomy and cardiac function. It has become the standard of care in valve replacement surgery, aortic and coronary artery surgery.1
Its use has also been validated in congenital heart surgery, and has shown to be useful not just for evaluating the corrections, but also as a guideline in hemodynamic therapy.2
The TOF is characterized by the presence of a ventricular septal defect (VSD), valvular or sub-valvular obstruction of the right ventricular outflow tract (RVOT), dextroposition of the aorta with overriding, and right ventricle hypertrophy. The broad spectrum of this malformation, the dynamic physiological changes, including the effects of the anesthetic agents, makes it a really challenging lesion. A case is presented where the surgical approach was based on the intraoperative transesophageal echocardiography.
A 15-year-old patient was referred to us for the correction of a TOF. The patient was scheduled for closure of the VSD with patch and expansion of the RVOTF.
Following an uneventful anesthetic induction and initiation of mechanical ventilation, a transesophageal echocardiographic probe was placed; as part of complete study, we evaluated the following characteristics, specifically prior to the correction and once again after the cardiopulmonary bypass3:
- •
Determination of the peak and mean gradient between the right ventricle and the pulmonary artery.
- •
Color Doppler examination of the inter-ventricular septum to outline the defect and assess the patch closure.
- •
Right Ventricular Ejection Fraction (RVEF) in a mid-esophageal 4-chamber view.
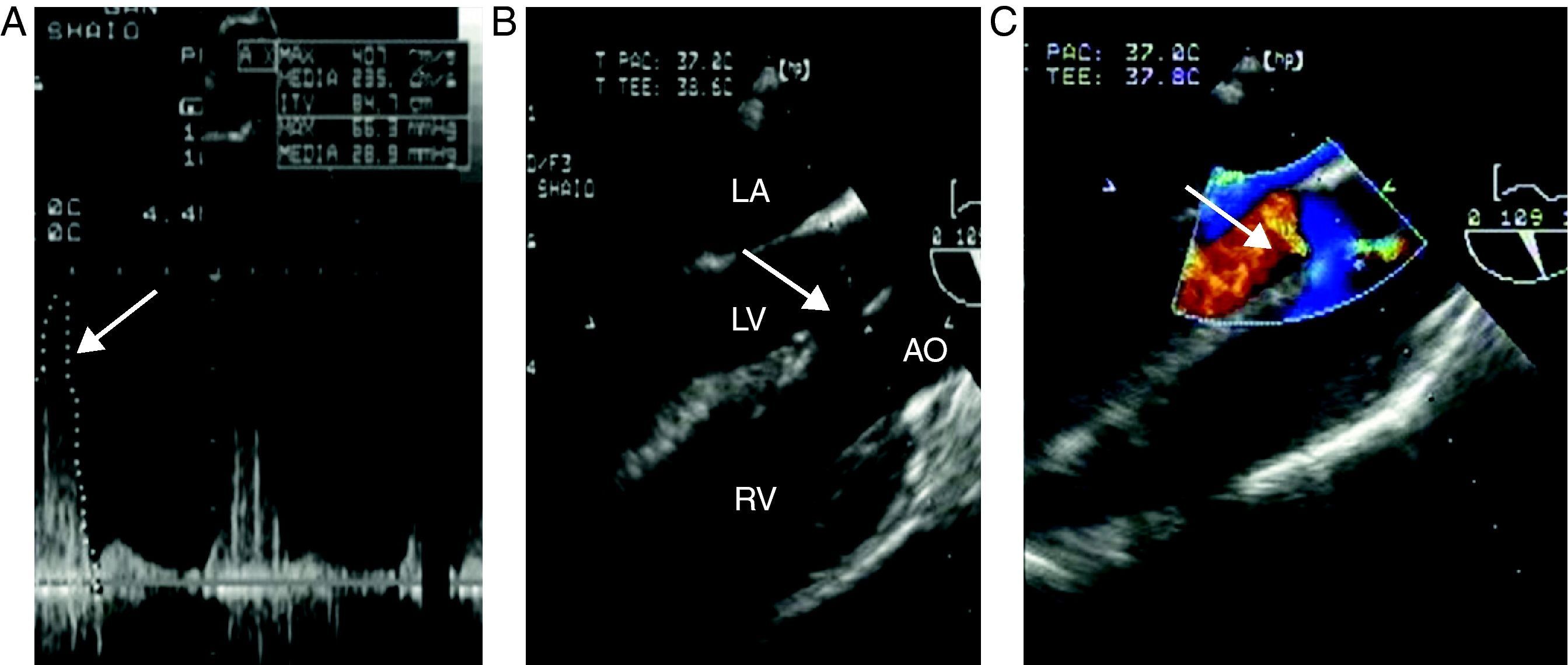
Our echocardiographic examination showed the classical findings of a TOF: extensive ventricular septal communication with right to left shunt, severe hypertrophy of the right ventricle with mild RVEF depression calculated at 35%, RV outlet tract obstruction with peak and mean gradients of 66 and 29mmHg, respectively (Fig. 1).
Pre-correction. (A) Continuous Doppler of the RVOTF with peak and mean gradient of 66mmHg and 29mmHg, respectively, in a deep trans-gastric of the right ventricle (Deep TG RV). The arrow indicated the peak gradient (B). Long axis of the aortic valve in the mid-esophagus (ME AV LAX) showing the classical characteristics of the TOF; overriding aorta and broad VSD. The arrow points the VSD. (C) Color Doppler interrogation of the previous view, showing right to left shunting trhough the VSD, the arrow points the flow. LA, left atrium; LV, left ventricle; RV, right ventricle; AO, aorta.
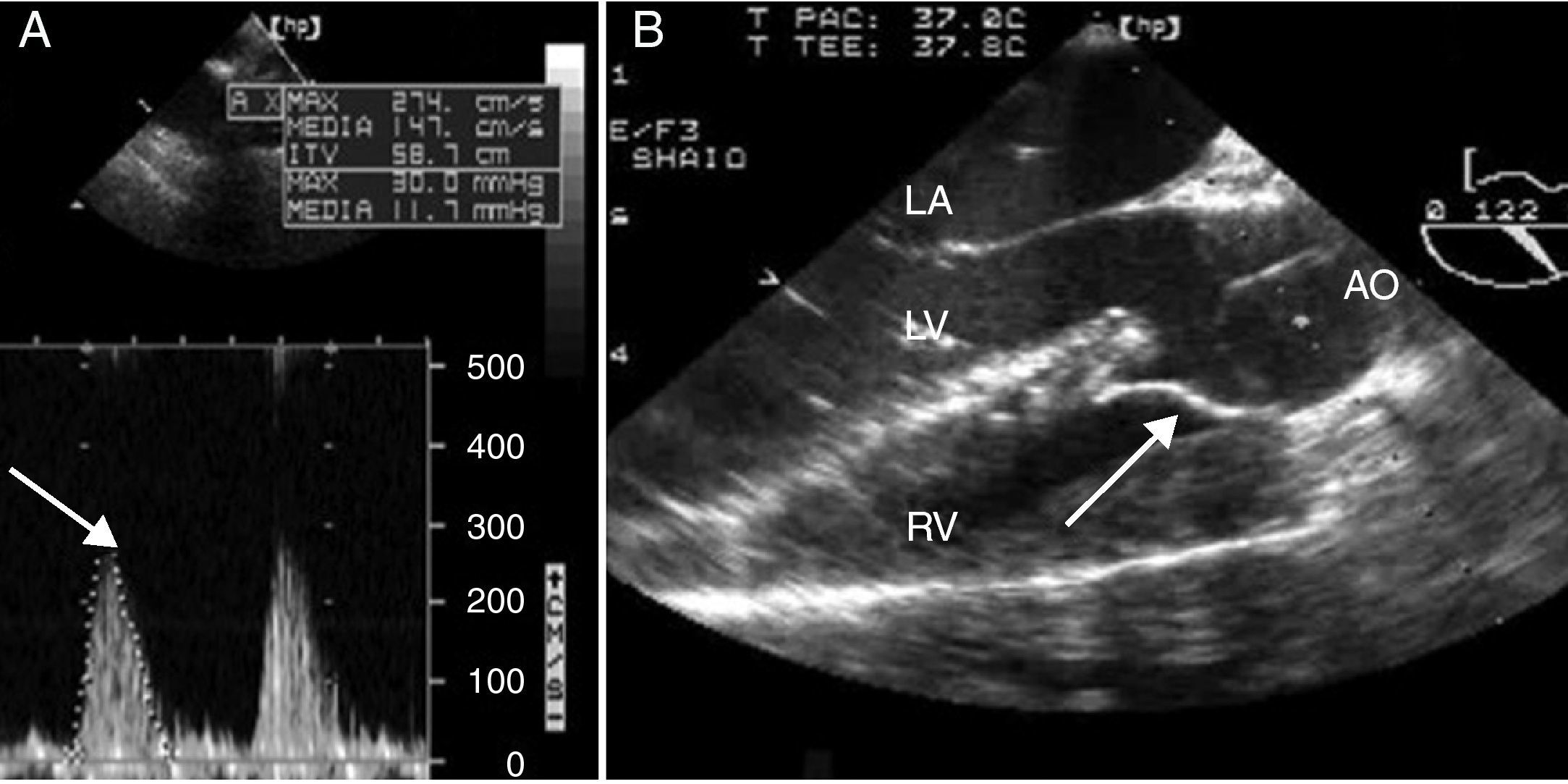
The patient was operated on using a transatrial, transpulmonary approach and 100min of pump time; following the correction, but prior to decannulation, a control echocardiogram was done, with the following results: ventricular patch with no residual shunt, left alignment of the aorta, reduced peak and mean RV outlet tract obstruction to 29 and 11mmHg, mild pulmonary failure, unchanged RVEF (Fig. 2).
Corrected. (A) Continuous Doppler of the RVOT with peak and mean gradients of 30 and 11mmHg in a deep trans-gastric of the right ventricle (Deep TG RV). The arrow indicates the peak gradient (B). Long axis of the aortic valve in the mid-esophagus (ME AV LAX) indicating the correction of the aorta aligned to the right with the patch. The arrow indicated the patch. LA, left atrium; LV, left ventricle, RV, right ventricle, AO, aorta.
The correction was considered adequate,4 and the patient was transferred to the Pediatric Intensive Care Unit (PICU) for two days and was discharged from hospital after six days of being admitted.
In our case report, the right ventricular function and the evaluation of the RVOTF were the two most important echocardiographic measurements in the management of the patient.
The right ventricle is a complex structure that contrary to the left ventricle cannot be described with conventional geometric models and this makes the evaluation of the ventricular function more difficult.
There are several echocardiographic parameters to assess the systolic function of the right ventricle, such as the right Tei index, displacement of the tricuspid ring, fractional area change and volumetric methods; however, none have been validated in the same manner as the ejection fraction for the left ventricle.
Any of these measurements could have been used in our patient; what is really important is the comparison between before and after the correction. The obstruction of the RVOTF determines the severity of the symptoms in this particular heart disease and hence determining the RVOTF gradient during the post-repair period is key to only to prevent a low cardiac output in the immediate postop, but during re-operations in the long term.
The classical approach to estimate the RVOTF gradient is to calculate the ratio between the right ventricle systolic pressure divided into the systemic systolic pressure; if the result is equal or less than 0.75, the correction is considered acceptable.4
The advent of intraoperative transesophageal echocardiography has led to the exact determination of the peak and mean RVOTF gradient using the continuous Doppler method according to Bernoulli's principle that establishes the relationship between flow acceleration and the increase in pressure through an orifice. In the case of correcting a TOF, a mean gradient above 54mmHg is an indication for revision of surgery.4
The instant mean gradient represents a more physiological measurement than the relationship between the systolic pressure of the right ventricle and the systemic pressure, because this relationship will be affected by multiple factors; i.e., in the case of systemic hypotension the ratio increases but does not represent a change in the degree of obstruction of the RVOTF.
To conclude, we would like to highlight the benefits of trans-esophageal echocardiography for evaluating the correction of the TOF.
FundingAuthors’ own funds.
Conflict of interestNone declared.
Please cite this article as: Orozco Vinasco DM, et al. Corrección de tetralogía de Fallot: papel del ecocardiograma transesofágico intraoperatorio. Rev Colomb Anestesiol. 2012;40:332–4.