Degenerative disc disease is a prevalent and disabling disease. When the conservative treatment fails to obtain pain relief, epidural steroids are an alternative frequently used worldwide.
ObjectivesTo evaluate the efficacy and safety of epidural methylprednisolone in patients with radicular pain.
MethodologyDescriptive longitudinal retrospective study in patients with chronic radicular pain who received fluoroscopy-guided interventional treatment, between July 2010 and December 2011 at Instituto Colombiano del Dolor (Medellín-Colombia), to determine the efficacy and safety of epidural methylprednisolone in clinical practice. Pain relief was followed using the visual analogue scale, during at least 8 weeks.
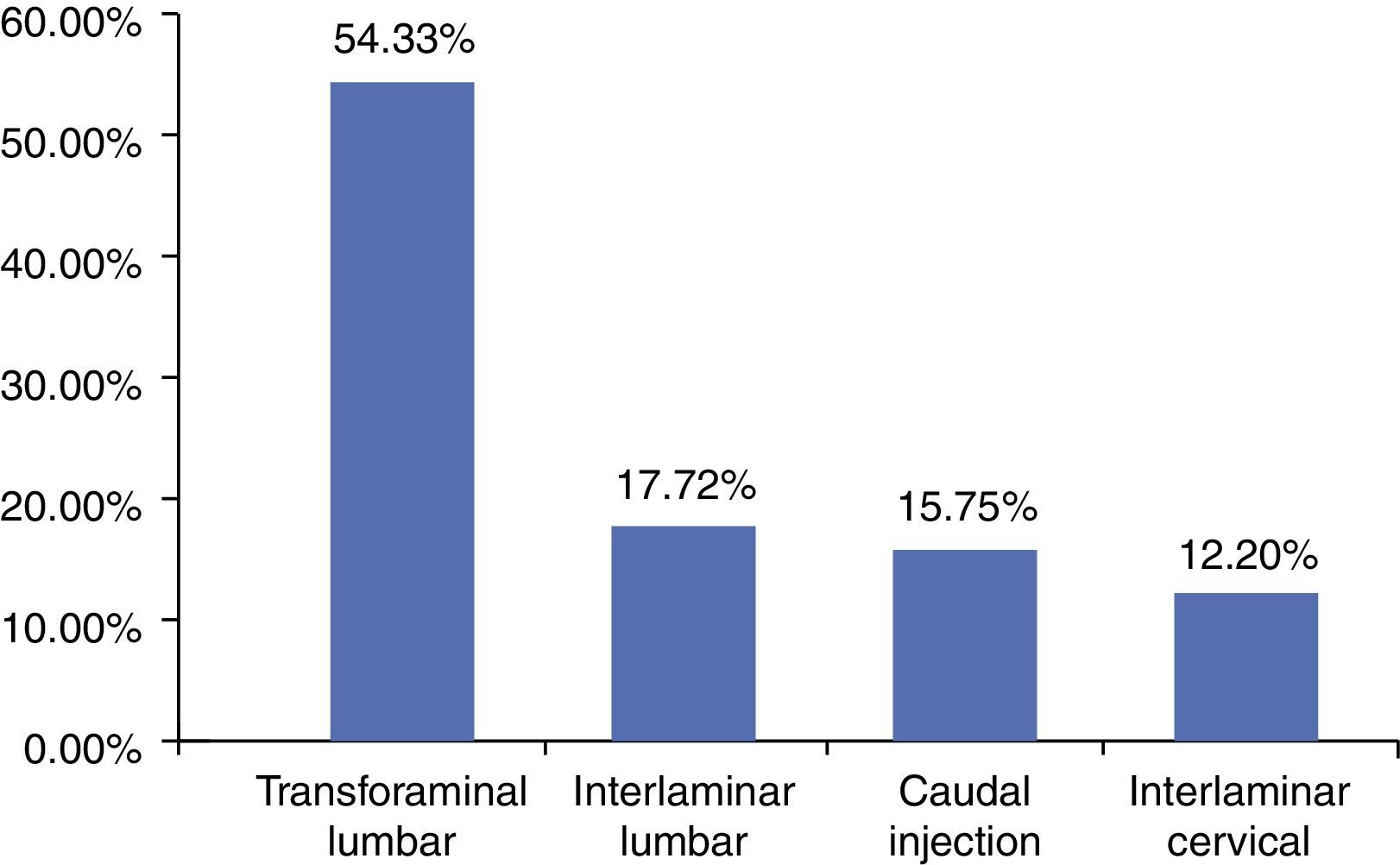
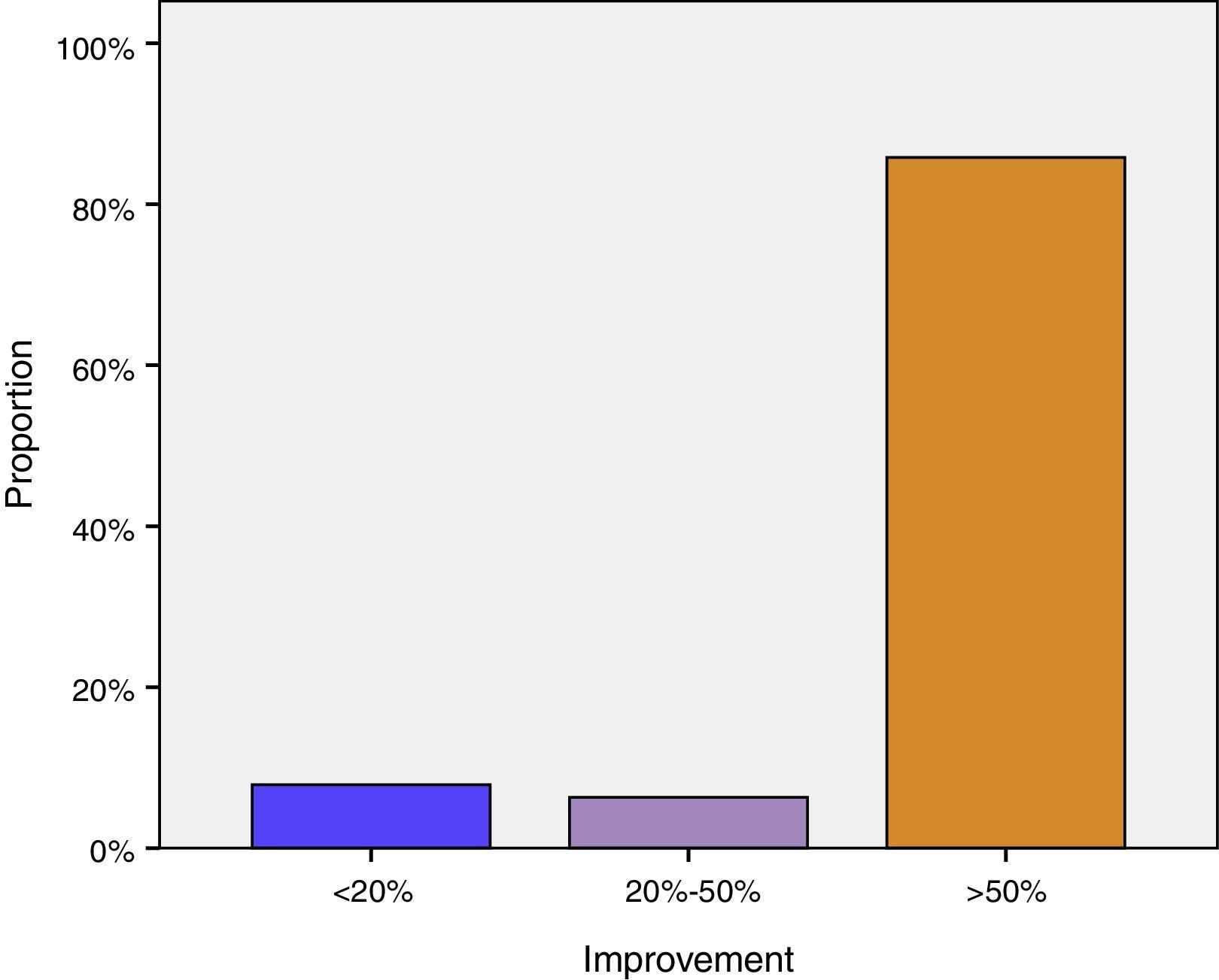
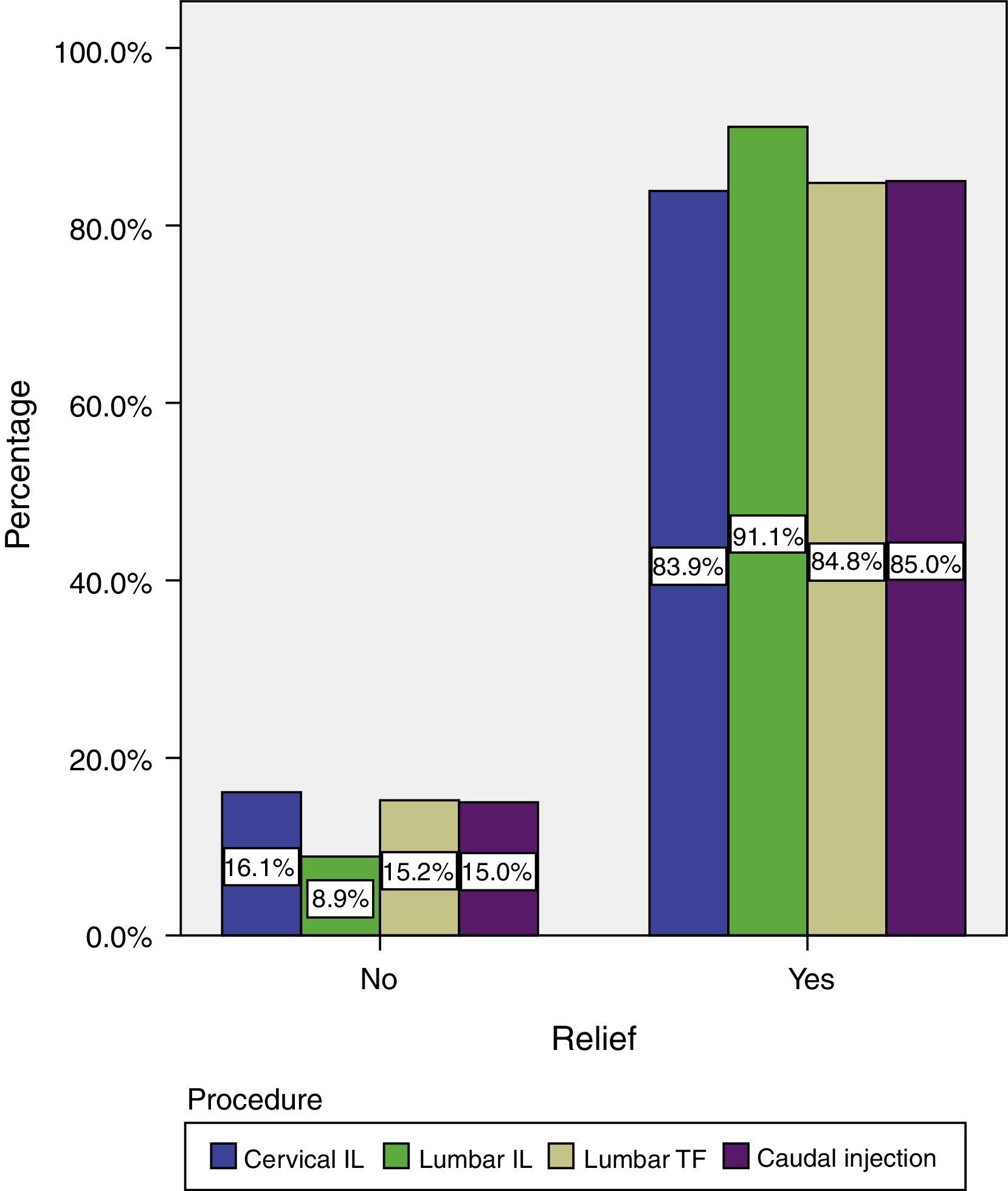
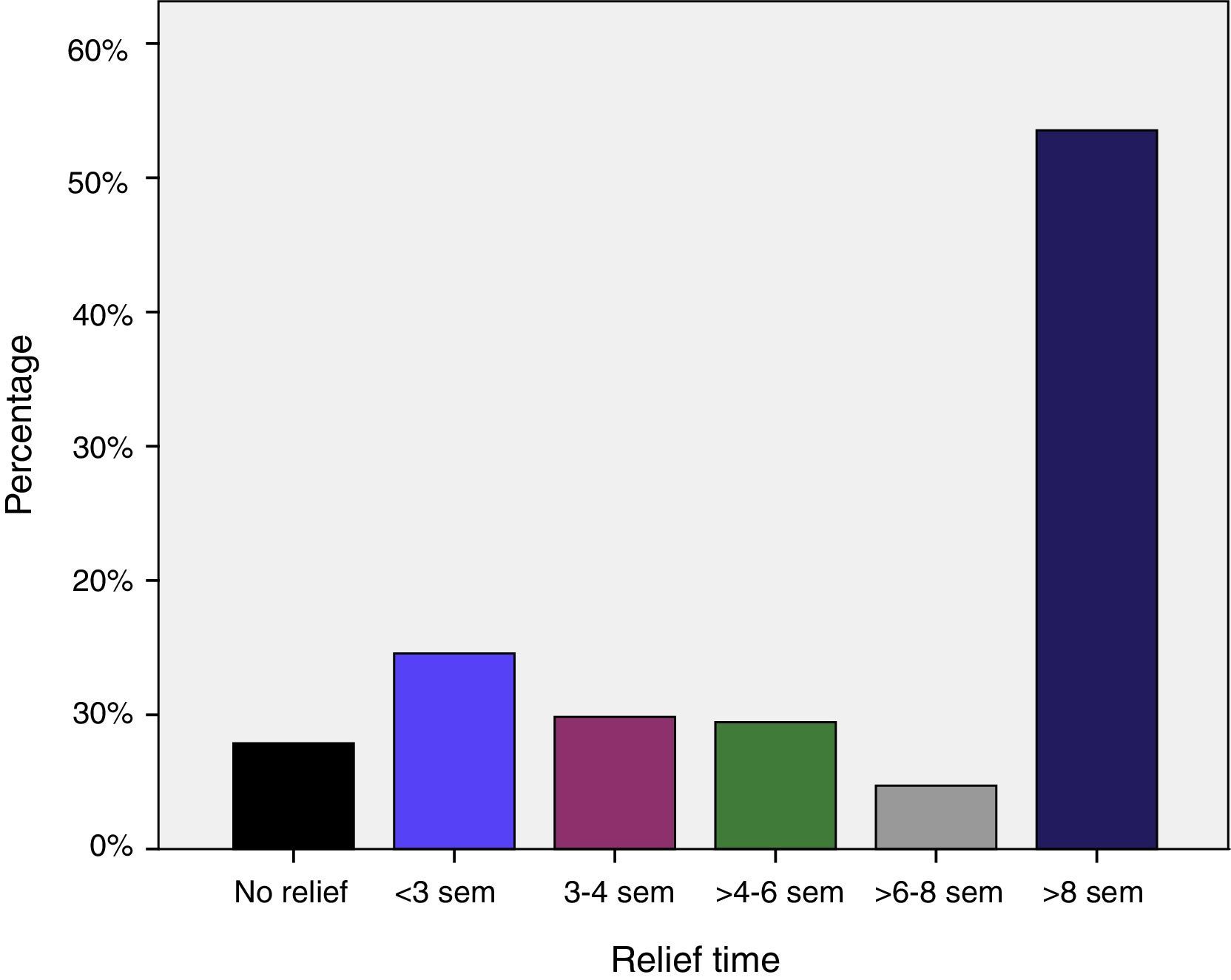
Results254 patients were analyzed. The mean age of the patients was 52.8 years (SD±15); 52.8% were men. The main diagnosis was lower-limb radicular pain (87.7%). The most frequent procedures were transforaminal lumbar injection (54.3%) and interlaminar lumbar injection (17.7%). The proportion of patients with more than 50% pain relief 50% was 85.8%. There were no differences in efficacy between the procedures. Pain improvement lasted more than 8 weeks in 55% of patients. The incidence of complications was lower than 1%.
ConclusionsWhen radicular pain is refractory to conservative treatment based on pharmacological and physical therapy, epidural methylprednisolone is an effective and safe method in our setting.
La enfermedad discal degenerativa es una enfermedad muy prevalente e incapacitante. Cuando el manejo conservador falla los esteroides epidurales son una alternativa de uso frecuente en todo el mundo.
ObjetivosEvaluar la eficacia y seguridad de la metilprednisolona epidural en pacientes con dolor radicular.
MetodologíaEstudio descriptivo longitudinal retrospectivo, en pacientes con dolor radicular crónico que recibieron tratamiento intervencionista guiado por fluoroscopia en el Instituto Colombiano del Dolor (Medellín-Colombia) en el período comprendido entre julio de 2010 y diciembre de 2011, para determinar la eficacia clínica y seguridad de la metilprednisolona epidural. Se realizó seguimiento del control del dolor medido por escala visual análoga por al menos 8 semanas.
ResultadosSe analizaron 254 pacientes. La edad promedio de los pacientes intervenidos fue de 52,8 años (DE±15), el 52,8% fueron hombres. El principal diagnóstico fue el dolor radicular en los miembros inferiores (87,7%). Los procedimientos más frecuentes fueron; inyección transforaminal lumbar (54,3%) e inyección interlaminar lumbar (17,7%). El 85.8% de los pacientes presentó disminución del dolor mayor al 50%. No hubo diferencias en la eficacia entre los diferentes bloqueos. En el 55% de los pacientes el tiempo de mejoría fue superior a 8 semanas. La incidencia de complicaciones fue menor al 1%.
ConclusionesCuando el dolor radicular es refractario al tratamiento conservador basado en terapia farmacológica y física, la metilprednisolona epidural es un método eficaz y seguro disponible en nuestro medio.
Chronic pain is one of the main reasons for visits to the emergency services as well as for general and specialized medical consultations. It has a significant impact on quality of life, leading to multiple instances of absence from work, and has a high impact on healthcare costs.1–5
Spinal pain is one of the most common forms of chronic pain.6 Between 70% and 80% of the population will suffer from lumbar pain during their lifetime. It is estimated that prevalence ranges between 12% and 15%, although it may be as high as 28–40%, depending on the different studies.8–11 National statistics for the United States show that chronic lumbar pain is the most frequent cause of functional limitation in people over 45 years of age, the second cause of visits to medical doctors, fifth cause of admission and third reason for surgery.8,12,13 Cervical and dorsal pain has also increased as a result of longer life expectancy.14
The aetiology of cervical, dorsal and lumbar pain is quite broad, including muscle disorders, disc disease,15 bone diseases, primary or metastatic vertebral tumours,16,17 spinal cord, cone or cauda equina tumours, intra-abdominal or retroperitoneal tumours, vertebral fractures or dislocations, ankylosing spondylitis, lumbar arthrosis, vertebral-epidural infections or abscesses, diabetic neuropathy, congenital abnormalities, among others.18–21
Vertebral and disc disease may produce mechanical nerve-root compression, while the local inflammatory effects of cytokines lead to reduced blood flow, intravascular coagulation and reduced nerve conduction velocity, affecting spinal nerve transmission and creating pain with a dermatome pattern called radicular pain.7,22,23
Discussed in the literature since 1950,18 following the initial experiences by Jean Enthuse Sicard and Fernand Cathelin, epidural steroid injections are the cornerstone in the treatment of axial as well as radicular chronic pain.
Steroids are a therapeutic option when conservative treatment has failed, pain relief being the result of reduced oedema and improved microcirculation.24,25
Because of their inhibitory effect on different cytokines, steroids have a potent anti-inflammatory effect and also variable results in terms of membrane stabilization, hyperpolarization of spinal neurons and c-fibre transmission inhibition. Epidural steroids are preferred over oral and intravenous steroids because they act on more specific targets.7
The epidural space may be accessed through the caudal, interlaminar and transforaminal approaches. It is recommended, within the basic care standards, that all procedures be guided by fluoroscopy in order to increase safety and the probability of success.18
For this reason, a study addressing the question “Is epidural methylprednisolone effective and safe in radicular pain?” is described below.
ObjectivesGeneral objectiveTo assess the efficacy and safety of epidural methylprednisolone in patients with radicular pain.
Specific objectives- -
To describe the social and demographic characteristics of the patients included in the study.
- -
To describe the main diagnoses that led to the performance of analgesic procedures.
- -
To describe the main analgesic procedures performed.
- -
To evaluate the proportion of patients who responded to the analgesic procedure.
- -
The evaluate percentage pain improvement after the analgesic procedure.
- -
To evaluate the proportion of patients who responded to the analgesic procedure by type of epidural analgesia utilized.
- -
To evaluate the duration of the analgesic effect after the procedure.
- -
To evaluate the adverse effects associated with the analgesic procedure.
Longitudinal retrospective descriptive study undertaken after obtaining the approval from the ethics committee of the Instituto Colombiano del Dolor (Medellín-Colombia) once it was also endorsed and approved by the ethics committee of Universidad Pontificia Bolivariana, considering that the study was classified as a no-risk research pursuant to Ministry of Health Resolution 8430 of 1993. The study was conducted in patients with chronic radicular pain who underwent interventional treatment under fluoroscopic guidance at Instituto Colombiano del Dolor (Medellín-Colombia) between July 2010 and December 2011. The analysis included the clinical records of 441 patients undergoing interventional analgesic procedures with some form of epidural approach and a follow-up period of no less than 8 weeks.
The following were the inclusion criteria: (1) radicular pain, (2) age 18 years and over, (3) use of fluoroscopy to guide the blockade.
The following were the exclusion criteria: (1) multiple procedures, (2) labour lawsuit, (3) prior spinal surgery, (4) diagnosis of fibromyalgia, (5) diagnosis of complex regional pain syndrome, (6) non-radicular pain, (7) age under 18, (8) follow-up during at least 8 weeks.
Steroid infiltration into the epidural space was done using one of the following approaches: interlaminar, caudal or transforaminal.
The technique used for performing epidural analgesia under fluoroscopic guidance in the patients included in this report was conducted in accordance with the protocols of the Instituto Colombiano del Dolor (Medellín-Colombia). The interlaminar technique with a Touhy 17 gauge needle was used for the epidural approaches, using loss of resistance to air or saline solution as confirmation, and verification of adequate placement with the help of contrast medium. Volumes of 10mL were used. The local anaesthetic used was 0.5% bupivacaine without epinephrine (10mg) and the particulate steroid was methylprednisolone acetate (80mg). The same doses were used for the caudal approach.
Transforaminal blocks were performed through a subpedicular approach using a 22-gauge spinal needle and contrast medium for confirmation. The doses used at the institution are 40mg of the same steroid plus 10mg of bupivacaine (3mL total volume). All patients were placed in prone recumbent position.
The magnitude of pain was assessed using the visual analogue scale (VAS) (with scores ranging from 0 to 10: 0, absence of pain; 1–4, mild pain; 5–7, moderate pain; and 8–10, severe pain) at 3, 4, 6 and 8 weeks.
- -
Age: Years at the time of performing the procedure.
- -
Gender: patient gender.
- -
Diagnosis: Diagnoses of patients with radicular pain were grouped according to the affected limb, as follows: right upper limb, left upper limb or both upper limbs; and right lower limb, left lower limb or both lower limbs.
- -
Procedure performed: Type of epidural analgesia, including interlaminar cervical, thoracic or lumbar; transforaminal cervical, thoracic or lumbar; and caudal.
- -
Improvement of pain after the procedure: Reduction of the pain score on the VAS after the procedure, classified as less than 20% improvement, 20–50% improvement, and more than 50% improvement.
- -
Response to the analgesic procedure: Significant relief was defined as a 50% reduction on the VAS when compared to the level of pain before the procedure.
- -
Duration of the analgesic effect after the procedure: Time in weeks during which the patient continues to experience pain relief after the procedure.
- -
Complications: The complications described include post-puncture headache – requiring or not a blood patch – bleeding, nervous, infectious and metabolic complications.
Data were obtained from secondary sources on the basis of the notes written in the clinical records. Records of patients with a follow-up of at least 8 weeks were considered.
The information was stored in a Microsoft Excel® database, and the statistical analysis was performed using the SPSS 18 package. A descriptive analysis of all the variables of the study was done on the basis of calculated proportions, central trend and scatter measurements. An association was also established between some qualitative variables using Pearson's Chi-square test. Statistical significance was set at less than 5%, with 95% confidence intervals.
ResultsOverall, 441 fluoroscopy-guided interventional analgesic procedures were performed at the Instituto Colombiano del Dolor (Medellín-Colombia) between July 2010 and December 2011. Of the patients, 68 were excluded because they had been undergone multiple procedures (facet block having been the most frequent), 14 due to lawsuits, 37 because of prior spinal surgery, 30 because of non-radicular pain and one individual under 18 years of age. Overall, 254 patients were analyzed.
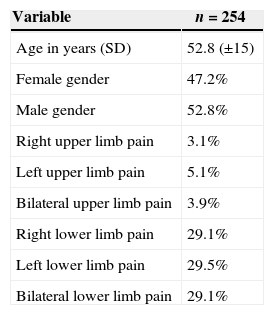
The mean age was 52.8 years (SD±15), and 52.8% of the patients were males. The main diagnosis was lower limb radicular pain (Table 1).
General characteristics of the patients assessed.
| Variable | n=254 |
|---|---|
| Age in years (SD) | 52.8 (±15) |
| Female gender | 47.2% |
| Male gender | 52.8% |
| Right upper limb pain | 3.1% |
| Left upper limb pain | 5.1% |
| Bilateral upper limb pain | 3.9% |
| Right lower limb pain | 29.1% |
| Left lower limb pain | 29.5% |
| Bilateral lower limb pain | 29.1% |
SD, standard deviation.
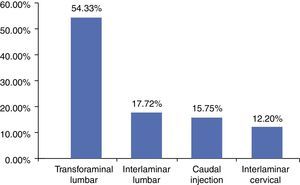
The main procedures were transforaminal lumbar injection (54.3%) and interlaminar lumbar injection (17.7%) (Fig. 1).
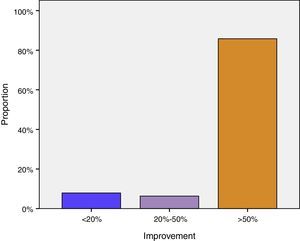
The proportion of patients with more than 50% pain improvement was 85.8%. Improvement in 6.3% of patients ranged between 20% and 49%, and only 7.9% reported less than 20% improvement in pain intensity after the analgesic procedure (Fig. 2).
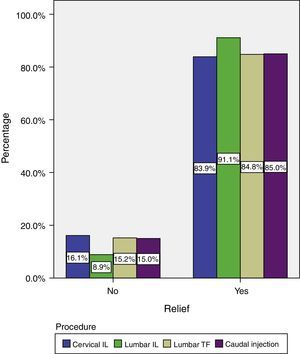
The best analgesic response was obtained in the group that received the interlaminar lumbar injection (91%). However, there were no statistically significant differences among the four types of blocks (p=0.7) (Fig. 3).
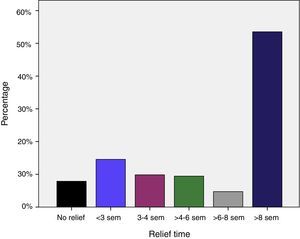
The majority of patients experienced pain relief for more than eight weeks (Fig. 4).
There were two complications (0.78% incidence): one patient who received cervical interlaminar injection had post-puncture headache, which improved with conventional analgesic management and did not require a blood patch; and one patient who received a lumbar transforaminal injection developed a localized puncture-site infection which was resolved satisfactorily with a 7-day antibiotic regimen.
DiscussionCurrent studies on the efficacy of epidural steroids are questionable given the absence of control and the lack of quality of the majority of them. The reason for the varying results of these studies is the absence of guidelines supporting dose, type of steroid, frequency of administration, or injection volume. Moreover, most of these studies were done without fluoroscopic guidance or contrast medium.6–8
Most of the studies report the use of epidural steroids for isolated lumbosacral radiculopathy, although others have addressed less specific pain such as that caused by lumbar stenosis.8
The use of epidural steroids has been assessed in observational studies. However, in our population, there are no follow-up reports of cohorts as the one proposed in this study. Additionally, the published literature is limited to different spinal segments, while this study addresses all spinal levels.
Success rates in the literature range from 18% to 90% depending on the methodology, the outcome assessed, patient selection and the technique used. This case series reported a high proportion of patients with improved pain scores, probably associated with patient selection and the use of fluoroscopy.
Interlaminar injections have shown strong evidence in favour of short-term improvement (less than 6 weeks)26–28 but weak evidence for long-term improvement (more than 6 weeks).6,7,29,30 Epidural injections are recommended in patients with both subacute (6 to 8 weeks) as well as chronic (more than 12 weeks) pain secondary to radiculopathy in the cervical and lumbar regions.1,7,31,32 Findings were indeterminate in cervical and axial lumbar pain, and in lumbar stenosis,6 hence the lack of sufficient evidence to support or refute the use of steroids in patients with no radicular pain.33 Transforaminal cervical procedures are not recommended and the total annual dose of steroids must be limited in order to avoid complications.7 The results of this study show short-term as well as long-term improvement, with no significant differences depending on the type of procedure.
Although outcomes also vary, Riew et al. reported lower rates of surgery following these types of procedures.34
The incidence of complications following these procedures varies among the various studies from 0.07% to 0.5%,35 similar to the findings of this study.
Although infrequent, adverse events may be catastrophic; knowledge of the local anatomy and the use of fluoroscopic guidance are key in preventing complications.18,36
Complications may occur as a result of the procedure itself or due to the injected drugs.
Complications associated with the procedure include post-lumbar puncture headache, with an incidence as low as 7.5% but which may also be as high as 75% depending on variables such as the technique, needle size and experience.37 The incidence ranges between 1.4 and 6% for lumbar interlaminar injection, 3.1% for transforaminal lumbar injection, 2.6% for thoracic interlaminar injection and up to 21% after caudal injection. Headache resolves spontaneously within seven days in 72% of patients and after six weeks in 85%.38–40
The incidence of infection is 1%. Most infections are minor such as local skin infections, but may also be as severe as epidural and intradural abscesses, osteomyelitis and meningitis. The main risk factor for their occurrence is a history of diabetes mellitus.35,38
Haemorrhagic complications associated with the procedure include acute subdural as well as epidural and subarachnoidal haematomas.41,42
From the neurological standpoint there may be transient motor weakness, cauda equina syndrome (very few cases reported) with symptoms usually resolving within hours or days; there may also be direct neurological damage.43–45
Metabolic adverse events, associated with steroid use, include hyperglicemia with blood sugar levels derangement lasting at least 2 weeks in diabetic patients.46,47
Suppression of the hypothalamic-pituitary axis may also occur over a period of 4–7 days. Exceptionally, Cushing syndrome may be present when steroid doses are very high over very short periods of time.48
Other steroid-associated complications include psychotic reactions, transient blindness,49 vasovagal episodes,50 chorioretinopathy,51 myopathy, anaphylaxis and facial flushing52 after dexamethasone administration, among others.35,53,54
In this case series, the incidence of complications of less than 1% may be related to the use of fluoroscopy, which contributes to an important reduction thereof.
ConclusionsThe treatment of radicular pain is mainly conservative, based on pharmacological and physical therapy, but in cases of refractory pain, epidural methylprednisolone is an effective, safe and readily available therapeutic option.
FundingThis work was funded with own resources and with the advice of the Universidad Pontificia Bolivariana University and CES.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors thank the doctor and anesthesiologist Epidemiologist Nelson Fonseca for his contribution.
Please cite this article as: Correa AÁ, Díaz RCR, Lotero MAA. Eficacia de la metilprednisolona epidural en el dolor radicular. Rev Colomb Anestesiol. 2015;43:61–67.