Cardio respiratory arrest in adults arises as a consequence of coronary artery disease in more than 60% of cases. At present, it is considered a public health problem.
It is important to keep in mind that prevention, through the adoption of healthy habits, is the principle contributor to the reduction of morbimortality. Nevertheless, when a malign arrhythmia that leads to cardiac arrest presents itself, the outcomes are directly related to the speed and quality with which cardiopulmonary resuscitation maneuvers are put into effect, and to the integral management of the clinical condition that is post-cardiac arrest syndrome.
These clinical practice handbook aim to provide sufficient information in order to guarantee appropriate medical attention in these cases. It is based on international norms of the lex artis in terms of the understanding and management of cardiac arrest.
What's more, criteria for determining brain death, and the organization of the advanced resuscitation team, which goes by various names around the world, emergency medical system, code blue, mega code, advanced resuscitation code, are included here.
El paro cardiorrespiratorio en el adulto surge como una consecuencia de la enfermedad coronaria en más del 60% de los casos. Se considera en la actualidad un problema de salud pública.
Hay que tener en cuenta que la prevención, a través de la adopción de hábitos saludables es el factor principal de la reducción de morbimortalidad, sin embargo cuando se presenta la arritmia maligna que conlleva al paro cardiaco, su desenlace está directamente relacionado con la rapidez y calidad con que se realicen las maniobras de reanimación cerebro cardio pulmonar y del manejo integral de la condición clínica del síndrome posparo cardiaco.
Este manual de practica clínica pretende brindar la información suficiente para garantizar una atención apropiada de estos eventos, y está basada en los lineamientos internacionales de la lex artis de la comprensión y manejo del paro cardiaco.
Además, se incluyen los criterios para determinar la muerte cerebral y la organización del equipo de reanimación avanzada, que en el mundo tiene varias denominaciones: sistema de emergencia médica, código azul, código mega, código de reanimación avanzada.
This purpose of this handbook is to describe the current directives for immediate and organized attention that is coordinated by a human team (health providers, doctors, nurses, nursing auxiliaries, etc.) both in practice and in the S.C.A.R.E.’s simulation laboratory. These directives are related to integral patient management during a cardiopulmonary-cerebral resuscitation event, from the start all the way up to the accompaniment of the patient by a health professional in the Intensive Care Unit.
Institutional justificationFrom the 2010 Resuscitation handbooks, which are currently valid, this document was created to address recommendations on primary, organized and coordinated attention by the human medical team (health providers, physicians, nurses, nursing auxiliaries, etc.). This team is in charge of providing basic and advanced life support in both the fields of clinical practice and in the S.C.A.R.E.’s simulation laboratory.
Methodology and narrative justification for completing these handbooksThis document is the product of the review of the recommendations produced by the International Guidelines of the American Heart Association (AHA), the European Resuscitation Council (ERC), and the International Liaison Committee on Resuscitation (Ilcor), and their adaptation to the Colombian context.
The development group for these handbooks, made up of educators in the area of anesthesiology and resuscitation, and of cardiology and critical care, worked together on the review of the pertinent literature of the most recent resuscitation handbooks and adopted figures corresponding to the Chain of Survival and the Basic Life Support Algorithm.
Definitions- -
Cardio respiratory arrest (CRA): Defined as the sudden and unexpected cessation of heart activity confirmed by the absence of a detectable pulse, unconsciousness, or suspension of breathing in a person who previously seemed to be completely healthy.
- -
Cardiopulmonary-cerebral resuscitation (CPCR), basic: The attempt to re-establish effective circulation through the use of external chest compressions and insufflation of the longs with air from exhalation or from some oxygen source (using a hand respirator).
- -
Unconsciousness: A situation in which a person is senseless, does not respond to stimuli, has no reflexes, and is disconnected from their surroundings. To confirm unconsciousness, proceed to evaluate 3 points of interaction:
- •
Visual: Observe that the victim is not moving.
- •
Physical: Proceed to move the victim by the shoulders.
- •
Verbal: Ask him, “Are you alright?”
- •
- -
Trauma: An injury in the human body caused by accidents, wounds, falls, or strong blows. Anesthetic-surgical trauma may also be included here.
- -
Cervical spine: Describes the part of the spine that corresponds to the neck zone. It is of great importance since the spinal cord, which connects the brain with the rest of the body, passes through it. Injury of the spinal cord may cause definitive paralysis of the arms and legs.
- -
Arteriosclerosis: The presence of fatty substances that form plaque on the arterial walls, which gradually produces an obstruction that limits the transfer of blood to the organs. This can eventually obstruct blood transfer completely. Nevertheless, more frequent is the rupture of the plaque and exposure to blood formed elements, together with an obstructive blood clot.
- -
Coronary artery disease: The complete or partial obstruction of one of several of the arteries that carry blood to feed the heart (coronary arteries), due to arteriosclerosis plaques or blood clots, which produces distress in the heart fibers and manifests itself as pain in the chest. A complete obstruction may cause an infarct—the death of part of the heart.
- -
Ventricular fibrillation: The continual chaotic and undulating movement of the heart's ventricles, which is not strong enough to pump blood. It is identified on the electrocardiogram (EKG) by its characteristic tracing of undulations without the presence of ventricular complexes. The condition is treated with defibrillation using special electrical devices called defibrillators (manual, automatic, external).
Coronary diseases in the United States and Canada are the cause of 350000 deaths per year (half of these occur out of hospital). The estimated incidence of extra-hospital cardiac arrest, attended to by emergency care systems in these countries, is approximately 50–55/100000 individuals/year, and of these, 25% present pulseless ventricular arrhythmias. This type of arrest rhythm has a better prognosis than do pulseless electrical activity and asystole. Ischemic heart disease is the leading cause of death in the world. Sudden cardiac arrest is responsible for more than 60% of adult deaths due to coronary artery disease. The incidence of in-hospital cardiac arrest is difficult to evaluate since it is influenced by hospital admission factors and the implementation of no-resuscitate orders. In the United Kingdom, the incidence of primary cardiac arrest was 3.3/1000 admissions, in the University Hospital of North Norway it was 1.5/1000 admissions, and in the USA it was 3–6/1000 admissions.
The statistics in Colombia are not reliable because an international registry of cardiac arrests (that follows the Utstein guidelines) has not been implemented. Extra-hospital cardiac arrest survival in North American countries is less than 8%. Nonetheless, in zones where CPCR and external defibrillation programs are applied by lay resuscitators, first responders (such as in airports and casinos), and by police, survival rates after cardiac arrest due to ventricular fibrillation are as high as 49–74%. Hence the importance of implementing programs that promote planned and organized responses, as well as training for resuscitators.
Resuscitation management – CPCRFollowing the sequence called the Chain of Survival is fundamental. It has the following specific objectives:
- a.
Secure the scene and recognize unconsciousness
- b.
Activate the Emergency Medical System (rapid response code)
- c.
Diagnose cardiac arrest
- d.
Begin chest compressions
- e.
Administer 5 cycles of 30:2 (30 compressions to 2 breaths) in the space of 2min
- f.
Acquire a defibrillator, in order to rule out the most frequent cause of cardiac arrest (ventricular fibrillation), and administer appropriate treatment
- g.
Familiarize the human advanced resuscitation team with the steps of secondary ABCD
- h.
Take the necessary measures in order to offer integral post-cardiac arrest care
- i.
Establish the scientific and legal parameters for declaring a cardiac arrest victim to be dead (brain death)
The following objectives should be underlined among the health professional team:
- j.
Identifying the equipment, devices and materials that belong in a cardiac arrest cart (Annex 1. Cardiac Arrest Kit)
- k.
Programming CPCR training workshops at least twice a year
- l.
Being part of a well-trained Advanced Resuscitation team in the health center
This clinical handbook for Resuscitation Management has been divided into three parts:
- •
Cardiopulmonary-cerebral resuscitation attention
- •
Organized emergency response system
- •
Declaration of brain death
The basic objective of this section is the early identification (quickly and timely) of unconsciousness, respiratory arrest and cardiac arrest in the patient, which can have multiple causes. With a rapid clinical diagnosis and a timely and appropriate response from trained health personnel, lives can be saved.
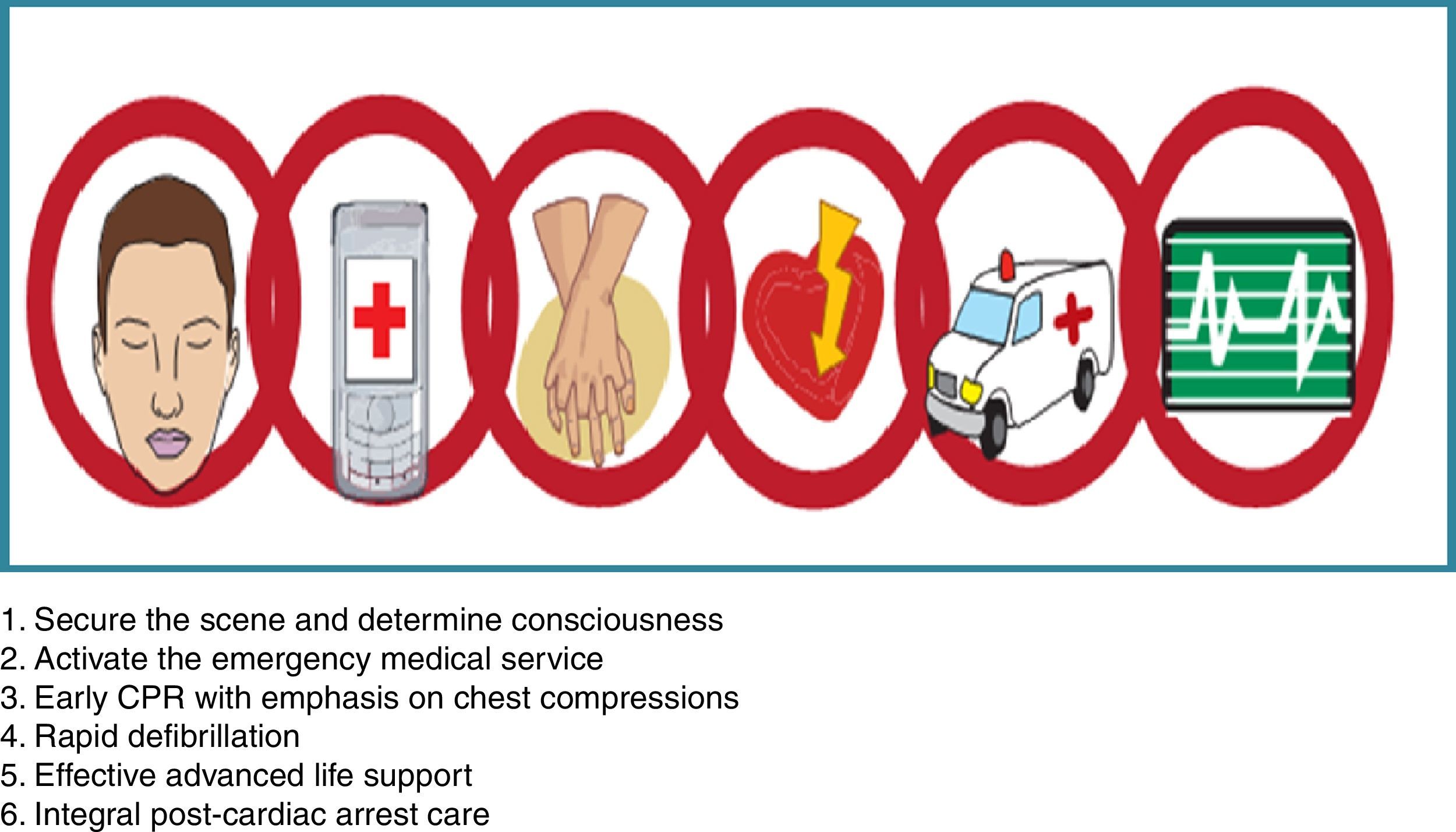
There are six links that make up the Chain of Survival (Fig. 1):
- •
Assessment of the state of consciousness
- •
Calling the Emergency Code
- •
CPCR maneuvers (with the new C–A–B sequence)
- •
Early defibrillation
- •
Advanced Life Support
- •
Integral Management of the post-cardiac arrest patient
Unconsciousness is when an individual suddenly loses consciousness. The diagnosis should be established within 10s the only exception is hypothermia, where the metabolism is in reality highly diminished. As such, 30–45s should be given to establish the diagnosis). The victim should be called by name, while resuscitators move his/her shoulders and produce some sort of sound stimulus close to the ears (e.g. clapping hands).
Activating the emergency response systemOnce the unconsciousness diagnosis has been established, the emergency response system of the hospitalary institution should be alerted through some sort of broadcasting medium (loud-speaker, internal phone system, mobile phone, direct calls, etc.). The key to this alert is to make clear, with an emergency code specific to the institution, that there is a patient that requires resuscitation, and concisely providing the location of the emergency.
Basic Life SupportIn this link of the chain, it will be established if the patient is in cardiac arrest by taking their carotid pulse for no more than 10s. Chest compressions must be initiated in a timely fashion at a rate of 30 compressions to 2 breaths in the space of 2min. The 30 compressions should take 18s in total and the 2 breaths should take 2s in total.
If the victim is unconscious but has a pulse, proceed to establishing if they are in respiratory arrest (Look, Listen and Feel ManeuverLook at the chest, listen to breathing, and feel breathing on cheek). Respiratory arrest is managed with breaths at the rate of one every 6s (10/min).
In resuscitation, teamwork is fundamental. That is why alerting the emergency response system (chain-link 2) is so vitally important.
Starting in the 2010 Resuscitation handbooks, the A–B–C sequence changes to C–A–B. The Look, Listen and Feel maneuver is not recommended at the beginning because resuscitators should proceed to establishing if the patient is in cardiac arrest through feeling for the carotid pulse and initiating chest compressions.
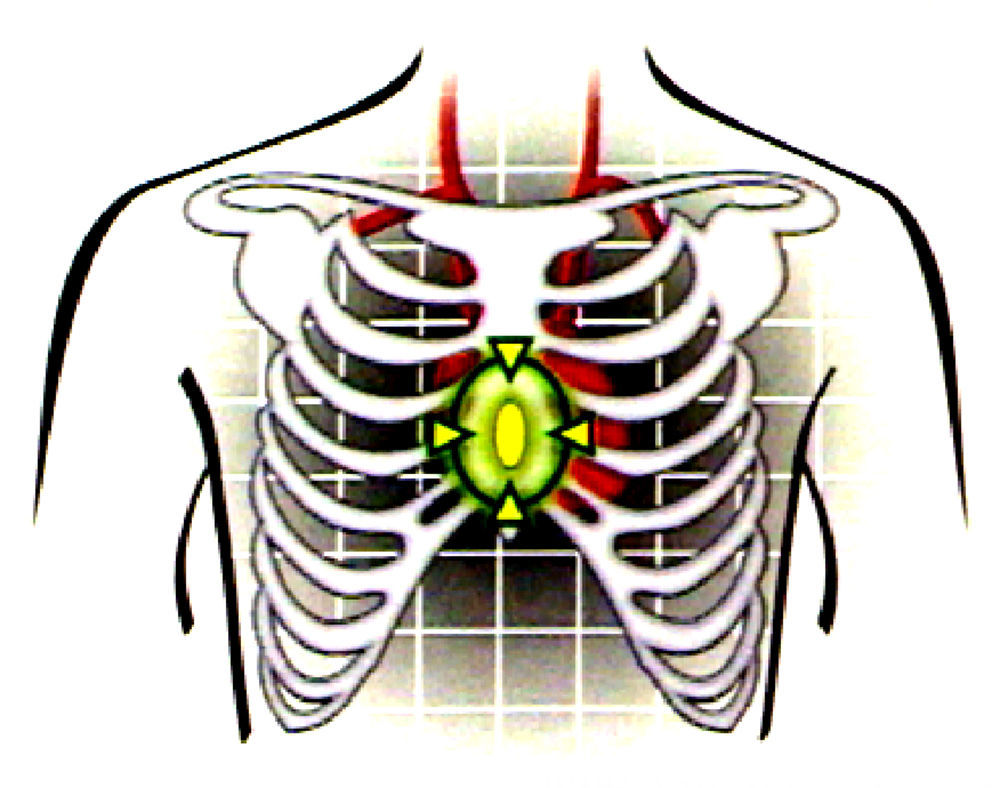
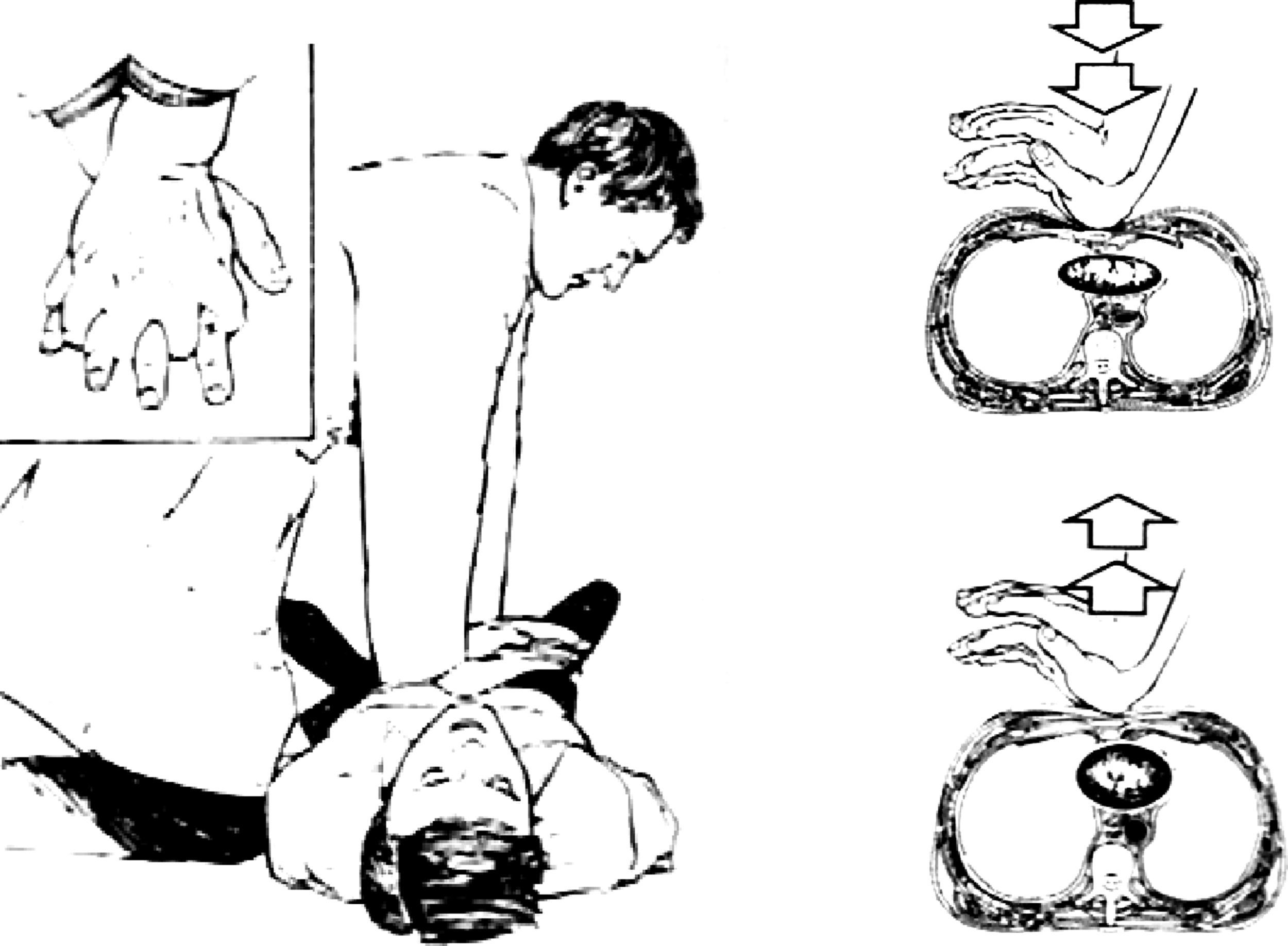
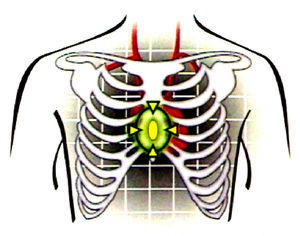
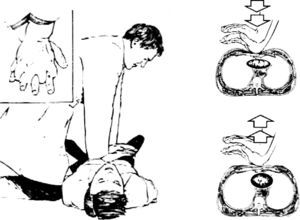
The resuscitator's hands should be placed in the center of the victim's thorax (Fig. 2) and the chest should be depressed at least 5cm. It is important to have the arms extended, allowing the weight of the resuscitator's body fall on the victim's thorax in such a way that the resuscitator's shoulders are perpendicular to the victim's midline. Proper chest compressions can be recognized by the resuscitator's use of the whole body, like a piston, with the only movement being in the hips (Fig. 3).
In health institutions, ventilation should administered with a manual ventilator (“bag-mask-reservoir” system), which helps provide 100% oxygen, with a tidal volume of 7ml/kg and in synch with the compressions (30 compressions: 2 breaths in 2min). Every 2min, the pulse should be assessed and the resuscitators should rotate tasks (chest compressions to ventilations and vice versa).
For successful ventilation when using an Ambu® bag, it is important to make use of an oropharyngeal tube of an appropriate size and to make sure that the insufflations follow the patient's exhalations.
The great advance in resuscitation, and practically the reason for the existence of the Chain of Survival, is the urgency with which defibrillation is administered. This link in the Chain of Survival is the D of the primary CABD paradigm and, at the same time, the beginning of the advanced resuscitation protocol. Today, it is known that cardiac arrest is a continuous event, where the two initial arrhythmias are pulseless ventricular tachycardia followed by ventricular fibrillation (the two most common causes of arrest—up to 80% of cases). Later, when the ATP of the myocardial fiber is exhausted, the heart enters into pulseless electrical activity and, later, falls into the rhythm of death and of the worst prognosis: asystole.
The practice of resuscitation has shown that poor use of the defibrillator (automatic or manual) is one of the most frequent medical errors. For this reason, it is vital that personnel working in the surgical area (operating, recovery and hospitalization rooms) know how the apparatus that they have at their disposal works in order to avoid, on one hand, accidents, and on the other hand, not providing an electric shock that could save a life on time.
The resuscitation handbooks recommend a single shock when defibrillating a ventricular fibrillation or a pulseless ventricular tachycardia.
The choice of shock depends on the type of defibrillator:
- –
If it is monophasic, 360J.
- –
If it has a rectilinear biphasic waveform, begin with 120J.
- –
If it has a truncated biphasic waveform, between 150 and 200J.
Early advanced life support depends on several factors:
- •
Trained and organized team with the authority and freedom to proceed according to their mission.
- •
Cardiac Arrest Cart, with sufficient and permanent resources, and unexpired medication.
- •
Response time of less than 5min at the in-hospital level and less than 10min at the out-of-hospital level.
Advanced life support, the secondary ABCD, is the initial stage of further treatment. It starts with:
- A.
Advanced management of the airway, whose class I therapeutic option is endotracheal intubation. When this is not possible for some reason, other proved extraglottic devices can be used, such as the classic laryngeal mask, the combitube, the SUPREME mask, the I-Gel, etc. (option IIa).
- B.
Refers to checking for and providing proper ventilation either manually or mechanically. The handbooks emphasize the use of the capnograph as a physiological monitor of appropriate resuscitation.
In this point, the 3 ventilation parameters should be assured:
- -
Tidal volume of 7ml/kg.
- -
Respiratory frequency of 10/min.
- -
1:1 inhalation/exhalation relationship.
- -
- C.
Consists of four procedures:
- •
Chest compressions
- •
Monitoring with electrodes
- •
Establishing IV lines
- •
Administration of medication
- •
- D.
Refers to differential diagnosis, which for simplicity and mnemonics has been summarized as ruling out the five Hs and five Ts.
The five Hs are: hypovolemia, hypothermia, H+ ion (acidosis), hypoxia and hypo/hyperkalemia. Previous handbooks eliminated hyperglycemia from the list, and placed it under the sixth link.
The five Ts are: cardiac taponade, coronary thrombosis (infarct), pulmonary thromboembolus, toxins and tension pneumothorax. Trauma was eliminated because its should be approached with another special algorithm that corresponds to the Advanced Life Support for Trauma workshop (Fig. 3).
It is important to underline that the scientific evidence recognizes basic life support, oxygenation and defibrillation as valid procedures and first-line therapeutic options when the cardiac arrest is produced by pulseless ventricular tachycardia and defibrillation. In the same way, in cardiac arrests from pulseless electrical activity or asystole, what is most important is the establishment of the differential diagnosis (the 5 Hs and the 5 Ts); it is probable that, despite adequate basic life support, the patient will not survive. For this reason, the American Heart Association (AHA) says: There are hearts too young to die (that deserve to be resuscitated) and hearts too old to live (that will not survive despite all efforts).
The alert system organized each institution is composed of a human resuscitation team, with all members of the surgical area (operating rooms, recovery rooms, hospitalization, sterilization) being trained in the field. Members of the team will be assigned a function according to their strengths and level of professional training. This team will congregate through the activation of a call or an emergency code and will respond immediately. The members of the team should arrive to the scene where the victim is (the team responds to the victim; the victim should not be moved to the team's location). It is recommended that only team members respond to the call in order to avoid chaos. To arrive to the emergency location, stairs should be used (not elevators). Each team member should know their functions and those of all other members so that if one person cannot perform their function, another can take their place.
All members should endeavor to achieve successful and verified processes. The emergency code ends when the team leader decides to suspend maneuvers in a patient that perishes, or until the victim that survives is appropriately moved and turned over to the intensive care unit. The team member in charge of the IV is responsible for the resuscitation records, but the entire team should be concerned with quality control through feedback.
The team is responsible for ensuring that medications and devices are replaced or put away if they are used, damaged or expired so that the cardiac arrest cart is always ready to be used in a new emergency. A communication channel should be kept open between the team and the attending physician and the family of the victim.
The response to the emergency code requires that a team leader be designated who directs the activities of the other members, takes care of the administration of medications, controls the verification processes, and carries out the major invasive procedures. This team member is also responsible for suspending maneuvers. Another member is in charge of the airway, of checking ventilation, of controlling devices like the capnograph and of managing medications that have the option of being administered intraosseously. Another member is responsible for running the defibrillator and for monitoring the patient. Yet another member is in charge of chest compressions and checking the pulse. The last member is in charge of establishing IV lines, taking blood samples, the administration of medication by IV, and of recording the activities and procedures that the team realizes.
First responder with trainingThe first responder will attempt to determine the state of consciousness along with the other elements described above. They will check the pulse for no more than 10s and, if they do not detect one, will initiate thirty compressions alternated with two breaths.
They will also ask someone to call for help by calling the agreed upon extension for activating the organized emergency response system (Code Blue). This is where this actor is different from the lay or untrained people who would limit themselves to administering compressions.
If the emergency occurs in one of the client care levels, they must call the head or auxiliary nurse to bring the cardiac arrest cart. Once the Code Blue team arrives, those in charge of compressions, airway management, and the administration of medications or shocks will be assigned.
The person in charge of administering compressions during the Code BlueThis member of the group will begin by giving thirty compressions once they determine the absence of a carotid pulse. They will alternate with the person in charge of the airway, who gives two ventilations after the thirty compressions (5 cycles of 30×2). It is important to depress the sternal area in adults and children by at least 5cm, and 4cm in lactating mothers so that the thoracic wall returns to its original position after the compression. This should be done at a speed of 100 compressions per minute, and without interruptions whenever possible. The person administering the compressions changes roles with the person administering ventilations every 2min in order to avoid fatigue and so facilitate the compressions.
Airway managementIf the responder is a layperson, or is untrained, it is best to disregard airway management and to focus, as was indicated above, on administering compressions until help arrives.
If the responder is a trained person, he should alternate thirty compressions with two breaths using the bag-mask device. Remember that giving mouth-to-mouth respiration without necessary protection (such as a face mask or shield) should be avoided when possible.
Other measuresIf possible, the patient should be monitored with the goal of determining the type of arrhythmia that produced the cardiac arrest: ventricular fibrillation (VF), pulseless ventricular tachycardia (PVT), and asystole or pulseless electrical activity (PEA). If it is determined that the patient has VF or PVT, the responder should proceed to defibrillation if a monophasic (360J/s) or biphasic (200J/s) defibrillator is available. For this, it is necessary to use conductive gel or cream. Likewise, the responder should ensure that a peripheral venous and/or intraosseous access has been established, if they have the necessary experience and equipment. Also, it is necessary to ensure that there is no “No Resuscitate” (NR) order.
Administration of vasoconstrictors and antiarrhythmicsAfter the first defibrillation, one may proceed with altering thirty compressions with two breaths for 2min and administering 1mg of epinephrine intravenously followed by 20ml of saline solution at 0.9% with the arm raised to the vertical position.
After this 2-min period, the carotid pulse is checked, along with the rhythm in the monitor. If VF or PVT persists, a second shock should be administered with the same amount of joules to continue, once again with another 2-min period of alternating breaths and compressions, and another dose of epinephrine (or a first and single 40U dose of vasopressin, if preferred). After the second period of compressions, the rhythm and the pulse should be evaluated again. If the arrhythmia persists, 300mg of amiodarone by IV are administered directly or in bolus. This is followed, once again by 20ml of saline at 0.9% in an elevated arm. If the shockable rhythms persist after this period, a third shock is administered. Try to determine why the patient has not recovered from the cardiac arrest. Is there a lack of ventilatory support, or are there other causes? (5 H–5 T). At this time, if no response has been obtained, securing the airway, ideally with a supraglottic device such as a laryngeal mask and a combitube, or with orotracheal intubation (OTT) if sufficiently trained, should be considered. Securing the airway should be only done under the orders of the team leader. If a capnometer is available, it should be used. The trachea should be used for the administration of medication only if it has not been impossible to establish intravenous or intraosseous access.
It is imperative that cardiac compressions and ventilation should follow each shock with no more than 5s of delay. Likewise, the electric shock should follow the compressions by no more than 5s. Epinephrine can be given every 3–5min; if the responder prefers to continue using only epinephrine, and if the arrythmias are persistent, a second 150mg dose of amiodarone by direct IV can be used followed by a saline flush with a raised arm. Remember that the other cardiac arrest rhythms, asystole and pulseless electrical activity, are not shockable.
ImportantAccompanying the resuscitation activities, there must be an active participation from all of the members of the team. Composure must be maintained in terms of not yelling or losing one's temper and of always providing constructive criticisms and mutual respect.
Once the maneuvers have ended, fill in the Code Blue form (Annex 2).
The success of the implementation of a Resuscitation Committee and the assembly of an immediate response team (Code Blue) depends on the determined participation of the Department of Education and the Scientific Subdirectory of the S.C.A.R.E. They will assign the resources needed for training and for the provision of necessary equipment for performing the resuscitation maneuvers. Definitely, the training process, through workshops, that is part of the development of psychomotor skills, requires declarative and procedural knowledge, something that implies a meticulous reading of the manuals at least 2 weeks prior to practicing.
Finally, the agreements, according to local legislation, will be established in order to define ethical norms, the No Resuscitation orders (NR) (that avoid maneuvers for victims that will not benefit from them), and the creation of monitoring mechanisms for the personnel that carry out resuscitation activities. It is highly recommended that the cardiac arrest records or Code Blue Forms (Annex 2) be applied and filled out. Therefore, the Resuscitation Committee should foster the use of these forms, as they will be useful for later research.
The last link in the Chain of Survival emphasizes the integral management of the post-cardiac arrest patient. It places importance on controlled hypothermia when the patient has already recovered spontaneous circulation, but continues in a comatose state. In addition, it is important to keep in mind that if the cause of cardiac arrest was acute myocardial infarction, it is necessary to carry out measures to ensure coronary circulation through fibronolysis, percutaneous coronary angioplasty, or revascularization. These are in no way contraindicated in patients in controlled hypothermia between 32°C and 34°C.
Declaration of brain deathThe concept of brain death was developed based on advances in medical science that, through technology, can replace the functions of the heart and the longs. Nevertheless, when the brain, which is the organ that is most sensitive to oxygen deprivation, suffers an irreversible anoxic degeneration, the spontaneous return to life is truly impossible. In 1968, the Harvard Ad Hoc Committee published a definition of irreversible coma as a synonym of brain death.
From the legal point of view in Colombia, Law 9/79 (National Health Code) defines brain death as the clinical state produced by irreversible changes that are incompatible with life and being necessary their certification by two doctors independent of the transplantation team. The clinical or para-clinical criteria are not defined. It is left up to the health professionals to determine what the irreversible pathological changes that are incompatible with life are. On the other hand, in the case of brain death, the physician has no ethical obligation to use techniques, pharmaceuticals or devices whose only use is to prolong the state of coma.
In the Second International Conference on Brain Death in Cuba in 1996, the following preconditions were considered:
- •
The cause of the coma should be documented and precisely establish as structural and irreparable brain damage. It must be sufficient so as to explain the loss of brain function.
- •
The patient should remain in a coma, ventilated with mechanical respiration, without any convulsive attacks, decorticate or decerebrate postures, or other responses originating in the encephalon (spinal reflexes may persist) for at least 30min.
- •
The following signs will be ruled out. If they are present (altered), they will need to be corrected:
- –
Hypothermia
- –
Systolic blood pressure greater than or equal to 85mm Hg
- –
If shock, it must be treated effectively and in a timely fashion
- –
The patient must not be in acute respiratory failure
- –
All primary and secondary metabolic disorders must be corrected
- –
- •
Diagnostic criteria
- –
Deep coma with no response to painful stimuli
- –
Absence of brainstem (photo-motor) reflexes
- –
The pupils do not respond to light stimuli
- –
Doll's eye phenomenon (i.e. the eyes of the patient with brain death remain fixed, just like the eyes of a doll when its head is moved)
- –
Corneal reflex; no blink response when the corneal epithelium is stimulated
- –
Absence of pharyngeal or tracheal reflexes —there are no gag or cough reflexes when stimulating the pharyngeal or tracheal mucus.
- –
Absence of Masseter reflex —no response to painful stimulation (pinch the cheek or the upper lip region)
- –
- •
Negative atropine test. 2–4mg of atropine are injected intravenously to see if there are changes in heart rate. The results are considered negative when there is no acceleration of the heart rate within 6min following the injection.
- •
Positive apnea test.
- –
The patient is oxygenated to 100% during at least 10min, while at the same time the ventilator is adjusted to achieve a PaCO2 of 40mmHg.
- –
The ventilator is disconnected and the patient is oxygenated at 8–12L/min with a tracheal cannula. If hypotension, arrhythmias or any sign of instability appears, the test should be suspended and the patient connected to a ventilator immediately.
- –
During the test, the existence of spontaneous ventilation will be evaluated. After 10min without evidence of spontaneous ventilation, a gasometry will be carried out and the patient will be connected once again to the ventilator.
The PaCO2 should exceed 60mmHg. This ensures a maximum stimulation of the respiratory centers. To summarize: If the PaCO2 exceeds 60mmHg and spontaneous breathing does not occur, the patient presented a positive apnea test. If spontaneous ventilation appears, the patient does not have apnea, and so does not comply with this diagnostic criterion for brain death.
EEG (electrical cerebral silence) – optionalObservation period: The criteria must be present for at least 30min and persist for 6h after. When rostrocaudal deterioration is observed despite treatment, the observation period may be shortened to 4h.
In conclusion, the diagnosis of brain death is clinical. Today, it is accepted that the apnea test, carried out in adequate conditions, is sufficient for this clinical diagnosis.
Complementary examinations are optional. Although the EEG can be administered, it frequently gives false positives in the results (isoelectric results) in situations involving intoxications or hypothermia. The nuclear brain scan and the transcranial Doppler test, which demonstrate the absence of cerebral flow, have high sensitivity (91%) and specificity (100%).
MedicationThe minimum of essential medications necessary to initiate cardiopulmonary-cerebral resuscitation can be found in Annex 1. This list should always be in the resuscitation team's bag so that, at the end of each month, the chief of the surgical area can ensure that they are present in sufficient quantities and that they are not expired. In each check, all medications that will expire before the end of the next month should be thrown out (destroyed).
The other elements, such as syringes, serums, tracheal tubes, probes, catheters, batteries, etc., should be replaced every three months in the case of the most recent supplies. The excluded supplies should be sent to the operating rooms to be used as quickly as possible.
If the resuscitation equipment is used, it is the responsibility of the coordinator of the Committee, or of the person in charge, to resupply the Resuscitation Team's bag (or the inventory) that very day after the suspension of resuscitation maneuvers.
RecommendationsThe clinical practice fields should have access to a resuscitation kit with a defibrillator in a cardiac arrest cart in the operating room or very close by. There should also be another resuscitation kit without a defibrillator in an easy-to-move box in the post-anesthesia recovery room, no matter the number of beds.
If there are three or more operating rooms, there should be two additional cardiac arrest carts (one in each operating room, and another in the recovery room), and also a resuscitation kit in the hospitalization area. If hospitalization is not next to the operating rooms of the recovery room, another cardiac arrest kit should be available. The cardiac arrest kit should always have a defibrillator and a cardiac arrest cart (wheeled transport of equipment, supplies and other necessary elements). The resuscitation kit does not contain a defibrillator and is transported in a special, easy-to-move box that contains all the medications and other elements necessary.
Basic Life Support algorithm (BLS)Chain of Survival:
- 1
1Diagnosis of unconsciousness
- 2
Activate emergency response system
- 3
Basic Life Support
- 4
If cardiac arrest, connect AED and proceed with algorithm
Whenever the AED “analyzes” or shocks, all personnel must stay away from the patient!
_____________________
AP: Arterial pressure
HR: Heart Rate
CPR: Compressions and breaths
The main author is the current president of the Colombian Society of Anesthesiology and Resuscitation.
Please cite this article as: Vargas JRN, Camacho HM. Manual de práctica clínica basado en la evidencia:: Reanimación cardiocerebropulmonar. Rev Colomb Anestesiol. 2015;43:9–19.
- Léalo en español
- Descargar PDF
- Material adicional