Hypothermia is recognized as a risk factor for perioperative complications in paediatric patients. High surgical risk procedures serve as a model of exposure to that risk factor. In particular, surgical correction of craniosynostosis serves as a model for measuring the impact of hypothermia.
ObjectiveTo assess hypothermia-related morbidity and mortality in paediatric patients taken to craniosynostosis correction.
MethodologyHistorical cohort study of patients taken to craniosynostosis correction and exposed to hypothermia.
ResultsWith prior approval of the Ethics Committee of the institution, 54 records were included in the analysis. No statistically significant differences were found between hypothermia and its impact in terms of morbidity and mortality (death, major bleeding, massive haemorrhage massive transfusion, disseminated intravascular coagulation, need for vasopressor support, mechanical ventilation time and length of stay, including admission to the intensive care unit). A clinically significant increase in bleeding (severe and massive) and severe hypothermia was found (28.6% vs. 40% and 14.3% vs. 40%, respectively).
ConclusionsNo statistical differences were found in terms of morbidity and mortality with severe hypothermia (and moderate/severe hypothermia).
La hipotermia es un reconocido factor de riesgo de complicaciones peri-operatorias en pacientes pediátricos. Para el estudio de sus impactos, las cirugias de alto riesgo quirurgico se comportan como un modelo de exposición a dicho factor de riesgo. En este punto, la correcion quirurgica de Craneosinostosis se comporta como un modelo para la medición de los impactos de la hipotermia.
ObjetivoEvaluar morbilidad y mortalidad relacionada a hipotermia en pacientes pediátricos llevados a corrección de Craneosinostosis.
MetodologiaEstudio de Cohorte Histórico en pacientes pediátricos llevados a corrección de Craneosinostosis expuestos a hipotermia.
ResultadosPrevia aprobación del Comité de Ética Institucional, incluimos 54 registros en el análisis. No encontramos diferencias estadisticamente significativas entre Hipotermia e Impactos en terminos de morbimortalidad (Mortalidad, Hemorragia Severa, Hemorragia Masiva, Trasfusión Masiva, Coagulación Intravascular Diseminada, Necesidad de Soporte Vasopresor y Tiempos de Ventilacion Mecanica, y Hospitalización, incluso en Cuidado Intensivo). Hallamos un aumento clinicamente significativo en la hemorragia (severa y masiva) e Hipotermia Severa, (28.6% Vs. 40% y 14.3% Vs. 40%, respectivamente).
ConclusionesLa hipotermia severa (y moderada a severa) no demostro en nuestros pacientes diferencias estadisticas para morbilidad y mortalidad.
As a risk factor for perioperative complications, hypothermia has been found to increase morbidity and mortality in paediatric patients. In the therapeutic context, the use of mild hypothermia has been advocated because of its neuroprotective effects and minor complications when compared with other more severe levels of hypothermia.1–3
Surgery for craniosynostosis repair in the paediatric population has been characterized as a subspecialized procedure with high rates of bleeding, transfusions and complications, primarily of hematologic nature.
An analysis of prior databases in our institution revealed that some complications (morbidities) would appear to change in incidence as a direct result of hypothermia. In the Colombian study by González et al.,4 the prevalence of disseminated intravascular coagulation (DIC) after craniosynostosis correction surgery was 35%, pointing to hypothermia as a probable causal factor according to the internal post hoc analyses.
Aware of the significance of this issue, a systematic review of the literature was conduced in PUBMED and LILACS with no restrictions of time, language or type of publication. The search terms Hypothermy AND Craniosynostoses, and Hipotermia AND Craneosinostosis, respectively, were used initially. No articles were found using these strategies. Then, when the terms Hypothermy, Surgical Procedures Operative AND Paediatric were used, the search yielded four publications in the form of review articles with information similar to the one cited previously; and six citations were found for the descriptors Hipotermia, Cirugia, AND Pediatria in the form of review articles or case reports (four) plus an additional two more focused on the effects on patients under cardiopulmonary by-pass circulation undergoing cardiovascular procedures. With this latter information it was not possible either to consider a hypothesis to answer our questions. In view of the above, it was concluded that there is a significant information gap regarding the impact of intraoperative hypothermia in paediatrics, which is even more notorious in non-cardiac high-complexity and high surgical risk procedures.5–7
Based on the scant evidence at the present time, and given the unknown impact of exposure to hypothermia, this study was developed with the aim to assess the impact of moderate/severe and severe hypothermia on morbidity and mortality associated with the surgical correction of craniosynostosis.
Materials and methodsFollowing the approval by the Research Committee and the Ethics Committee for Research in Human Subjects at Fundación Hospital Infantil Universitario de San José, and by the research division and the graduate programme office of Fundacion Universitaria de Ciencias de la Salud, an analytical observational study with a historical cohort design was conducted in paediatric patients taken to craniosynostosis repair surgery at our hospital between 2008 and 2015. The inclusion criterion was patients with a complete intraoperative temperature record. Records lacking adequate temperature data and/or with no temperature entries in the anaesthesia record were excluded. In an initial analysis, exposure was defined as mild hypothermia or euthermia, and in a second analysis exposure was defined as the presence of severe hypothermia (only). For discrimination between those diagnoses, the definitions in the article by Castillo et al.8 were adopted as follows: mild hypothermia – temperatures (T°) below 36°C and above 34.9°C, moderate hypothermia – T° below 35°C and above 33.9°C, and severe hypothermia – T° below 34°C and above 32°C.
The main objective was to measure the impact of hypothermia on the incidence of complications in that cohort. Based on the assumption that moderate-to-severe and severe hypothermia are associated with an incidence as high as 35% of disseminated intravascular coagulation,4 and that normothermia or mild hypothermia could lower that incidence by up to 5%, we arrived at total number of 54 patients (27 in each arm) needed for the assessment, using two tails, a 95% accuracy, a power of 80% and a 1:1 ratio between exposed and non-exposed patients.
Quantitative statistics were presented based on their type, using central trend measurements (means or medians) and scatter measurements (ranges and standard deviations), depending on their distribution; qualitative variables were presented as absolute frequencies and percentages. Hypothesis comparisons were performed according to the statistical requirement, using the χ2 test for qualitative variable comparisons and the student t test or the U Mann Whitney test for quantitative variables. If the measurement required it, impact was calculated in RR plus 95% confidence intervals. A p value of <0.05 was used for statistical significance. Data were processed using the STATA 12.0 software package. For adverse event descriptions, the follow-up period was standardized as the first five days in the hospital, meaning that only immediate or early perioperative adverse events were included.
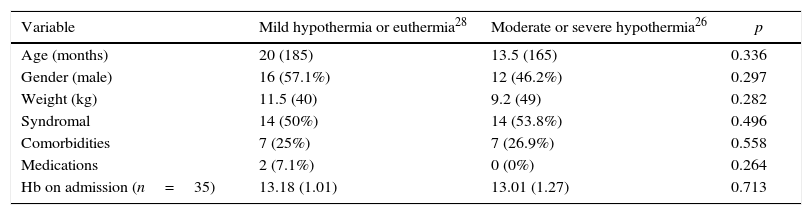
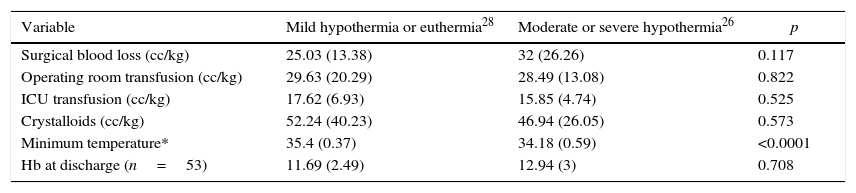
ResultsOverall, 81 records were collected for the selected time period. Of these, only 54 met the selection criteria. Demographic and surgical characteristics are presented below (Table 1). There were no statistically significant differences between the groups in terms of the preoperative characteristics. In 100% of patients there was no hypothermia at the start of the procedure. Table 2 shows the comparison of powered intraoperative outcomes. The only relevant difference was lower mean temperature during surgery.
Demographic variables. There were no statistically significant differences between the groups.
| Variable | Mild hypothermia or euthermia28 | Moderate or severe hypothermia26 | p |
|---|---|---|---|
| Age (months) | 20 (185) | 13.5 (165) | 0.336 |
| Gender (male) | 16 (57.1%) | 12 (46.2%) | 0.297 |
| Weight (kg) | 11.5 (40) | 9.2 (49) | 0.282 |
| Syndromal | 14 (50%) | 14 (53.8%) | 0.496 |
| Comorbidities | 7 (25%) | 7 (26.9%) | 0.558 |
| Medications | 2 (7.1%) | 0 (0%) | 0.264 |
| Hb on admission (n=35) | 13.18 (1.01) | 13.01 (1.27) | 0.713 |
Source: Authors.
Surgical outcomes (*statistically significant differences).
| Variable | Mild hypothermia or euthermia28 | Moderate or severe hypothermia26 | p |
|---|---|---|---|
| Surgical blood loss (cc/kg) | 25.03 (13.38) | 32 (26.26) | 0.117 |
| Operating room transfusion (cc/kg) | 29.63 (20.29) | 28.49 (13.08) | 0.822 |
| ICU transfusion (cc/kg) | 17.62 (6.93) | 15.85 (4.74) | 0.525 |
| Crystalloids (cc/kg) | 52.24 (40.23) | 46.94 (26.05) | 0.573 |
| Minimum temperature* | 35.4 (0.37) | 34.18 (0.59) | <0.0001 |
| Hb at discharge (n=53) | 11.69 (2.49) | 12.94 (3) | 0.708 |
Source: Authors.
No statistically significant differences were found for outcomes of interest such as intraoperative blood loss and transfusions, comparing the groups exposed to the two levels of hypothermia included in the protocol (Table 2). Temperature was the only variable showing important clinical and statistical differences.
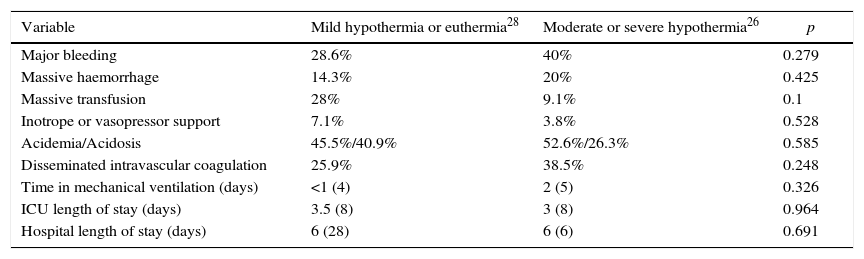
Regarding reported outcomes such as morbidity, no statistically significant differences were found between the groups (see Table 3).
Medical and surgical complications (comparing mild hypothermia euthermia vs. moderate–severe hypothermia). No statistically significant differences were found.
| Variable | Mild hypothermia or euthermia28 | Moderate or severe hypothermia26 | p |
|---|---|---|---|
| Major bleeding | 28.6% | 40% | 0.279 |
| Massive haemorrhage | 14.3% | 20% | 0.425 |
| Massive transfusion | 28% | 9.1% | 0.1 |
| Inotrope or vasopressor support | 7.1% | 3.8% | 0.528 |
| Acidemia/Acidosis | 45.5%/40.9% | 52.6%/26.3% | 0.585 |
| Disseminated intravascular coagulation | 25.9% | 38.5% | 0.248 |
| Time in mechanical ventilation (days) | <1 (4) | 2 (5) | 0.326 |
| ICU length of stay (days) | 3.5 (8) | 3 (8) | 0.964 |
| Hospital length of stay (days) | 6 (28) | 6 (6) | 0.691 |
Source: Authors.
When the analyses described above were performed assessing the effect of severe hypothermia compared to mild hypothermia or euthermia, only five patients (9.25%) of this cohort were found in this subgroup.
The mean temperature in the severe hypothermia group (33.38°C, SD=0.39°C) versus (35.4°C, SD=0.37°C) the non-exposed group was significantly lower (p<0.0001).
In the records with severe hypothermia, median age was 11 months (range=20) and median weight was 8 Kg (range=6), unlike those with mild hypothermia or euthermia (age=20 [range 185] and weight=11.5 [range 40]) where there were no statistically significant differences (p=0.093 and p=0.051, respectively). The borderline nature of those values is debatable and their true ability to cancel the hypothesis is nil.
Syndromal nature (p=0.53), comorbidities (p=0.277), medications (p=0.716), and Hb on admission (0.122) were not different between the groups. Also, no statistically significant differences were found between the groups when surgical outcomes were measured: discharge Hb (p=0.123), intraoperative transfusion (p=0.696), ICU transfusion (0.496) and crystralloids (p=0.482). Only intraoperative blood loss was significantly higher (p=0.007) in patients exposed to severe hypothermia (54.24cc/kg SD=47.04 vs. 25.03cc/kg SD=13.38).
Table 4 summarizes the findings regarding the complications included in the protocol.
Medical and surgical complications (mild hypothermia – euthermia vs. severe hypothermia). No statistically significant differences were found.
| Variable | Mild hypothermia or euthermia28 | Severe hypothermia5 | p |
|---|---|---|---|
| Major bleeding | 28.6% | 40% | 0.485 |
| Massive haemorrhage | 14.3% | 40% | 0.216 |
| Massive transfusion | 28% | 20% | 0.595 |
| Inotrope or vasopressor support | 7.1% | 0% | 0.716 |
| Acidemia/Acidosis | 45.5%/40.9% | 80%/0% | 0.213 |
| Intravascular disseminated coagulation | 25.9% | 40% | 0.437 |
| Time in mechanical ventilation (days) | <1 (4) | 2 (5) | 0.364 |
| ICU length of stay (days) | 3.5 (8) | 4 (6) | 0.542 |
| Hospital length of stay (days) | 6 (28) | 8 (5) | 0.478 |
Source: Authors.
It is important to clarify that no statistically significant differences were found between the exposure groups for those outcomes, except for intraoperative blood loss volumes.
DiscussionNo statistically significant differences were found in our results when comparing the items studied (major bleeding, massive haemorrhage, massive transfusion, DIC, need for vasopressor support and time in mechanical ventilation, ICU and hospital stay, and mortality) with regard to the various types of hypothermia. Notwithstanding, it is important to highlight the increase in major bleeding and massive haemorrhage in patients with severe hypothermia; although not supported by a relevant statistical value, this points to a potential difference in clinical relevance. A larger sample of patients exposed to this factor is needed in order to confirm this finding.
Notwithstanding our findings, it is difficult to infer or conclude that hypothermia, as it was studied, does not impact morbidity and mortality in paediatric patients taken to craniosynostosis repair. There are still many measurement limitations, and the multiple risk factors involved preclude a final conclusion.9–14 However, based on these data and in contrast with traditional thinking, at these levels of hypothermia (moderate and severe) surgical outcomes may not worsen and there is no increase in the incidence of morbidity and mortality.
It was not easy to arrive at a clear axiomatic definition of hypothermia and, in fact, several diagnostic classifications have been published.7,14 In our case, we worked with the definition by Castillo et al. published in Revista Colombiana de Anestesiología (Colombian Journal of Anaesthesia).8 Although it is feasible to find more stringent classifications regarding temperature lowering, we believe that in patients undergoing this procedure, the probability of lowering the temperature below 32°C in the operating room is quite atypical. During the protocol phase, including a critical reading of our previous study, we found that not all of the patients intervened in the program were subjected to temperatures below those mentioned above.
It is striking that the percentage of patients with any degree of hypothermia during the surgical procedure despite the usual techniques used to maintain the temperature in our hospital (in 81% of cases) is higher than that reported by Crisotomo et al. (43.8%) and very different from that reported by Lee (0.4%).9 Our protocols are similar to those of these authors because, like those institutions, were also use warm flow blankets, so far considered a very effective method to counteract the decrease in central temperature.15,16
Our population was similar to those of other reports in terms of weight, age, gender, comorbidities and associated syndromes, the only difference being the presence of different degrees of hypothermia. The latter enables us to estimate and analyze different data based on the confirmation that this cohort indeed had similar preoperative conditions and was different only in terms of exposure, the outcome being absent at the start of surgery.13,15,17,18
In analysing this work, it is of the utmost importance to mention that we suspected a high probability of finding an association between severe hypothermia and morbidity, considering that this condition has been associated for decades with increased morbidity and mortality, in particular coagulopathy.5,14,18–20 However, no direct or statistical association was found between patients exposed to lower temperatures and bleeding. Consequently, estimating RR for that outcome was not warranted.
For Stricker,21 increased blood loss in a similar population occurred with temperatures under 34°C. However, that hypothesis was not confirmed by the results of this study, perhaps because of the small sample size included in the extreme low levels and the absence of records of less than 32°C.
Like Kho and Gries,22 although we did not find differences in our study in terms of the transfused packed red blood cells (PRBC) or the percentage of massive transfusions, it must be stated that it is not realistic to avoid blood loss in this type of procedure. It is impossible despite technical and medical breakthroughs and, therefore, blood product transfusions are unavoidable in the majority of these patients, despite the protocols studied that change the volume to be used of PRBC.9,15,17,19,22,23
Despite being aware of the value of early restrictive transfusions in this type of procedure and patient (with immature haemostatic systems),20 we continue to advocate the use of strategies that limit and may eventually replace this strategy (often massive transfusion), which has been correlated with multiple risks and potential complications.9,12,15,19,22,23
The mean length of our procedures had been estimated in the past at 303.1min (SD=92) with little variation between surgeries, but this is secondary to our management protocol and the need to strengthen the surgical team day by day (González et al.).4 Nonetheless, we have a choice of defining the maximum hypothermia time until control is achieved, and of selecting the therapies to be used. It is important to clarify that, not being an intervention (ethical considerations), hypothermia cannot be observed without first instituting some form of control therapy. The approach in this study was to include patients exposed to hypothermia, measured in real time with the use of trans-oesophageal thermometers. This criterion defined the feasibility of including a considerable sample without any form of additional temperature measurement. However, owing to the nature of this criterion, it did not work on the assumption of an association between accurate hypothermia times, variations and effect and primary and secondary outcomes using correlation coefficients or linear/logistic regression models.
Considering that this procedure is associated with substantial blood loss,17,19,23, the study data are similar to those of other researchers in the world. Fearon et al.24 estimated a preoperative Hb of 13, similar to the value in this study, but postoperative behaviour and level were very different (+/−9 versus +/−12 in our study), analyzed as secondary to a lower transfusion rate (15% vs. 68%, respectively). For Meyer et al.,25 the reported transfusion rate was as high as 66% during the perioperative period, similar to what is described in this article.
There were clinical and statistically significant differences in intraoperative blood loss in patients exposed to severe hypothermia (p=0.007) when compared with blood loss volumes in cases of mild hypothermia or euthermia (54.24cc/kg SD=47.04 vs. 25.03cc/kg SD=13.38). Despite consistency between these findings and what severe hypothermia has been shown to do in terms of the pathophysiology, the isolated value was not compounded by other medically or surgically relevant outcomes. In fact, the incidence of severe or massive haemorrhage and of massive transfusion was similar in both groups. Bleeding rates, although different, perhaps were not as relevant.
Although the number of transfusions in our patients was high, no increase was observed in mortality, and only DIC and acid–base imbalances towards acidosis or academia were found to be increased. These findings are in agreement with those published and supported by Choi et al.10 and Meyer.25
Despite its clinical significance, in our cases we focused on primary management of other outcomes (e.g. bleeding), and acid–base status was a dependent variable resulting from other compromises requiring a more prompt intervention. This may explain the high percentage of metabolic acidosis/acidemia found in our study (close to 50%) compared to that reported by Stricker (19%).21
The reliability of intraoperative and ICU bleeding data needs to be highlighted. This is the result of the medical protocol and of the fact that it is the basis for the decision to proceed with early transfusion of blood products. In contrast, several other reports recognize the weakness of their estimates.
DIC is mentioned as one of the main complications of this procedure. Indeed, the figure in our previous report was 35%, and the figure in this report is 32.1%, its clinical occurrence being more frequent among patients with severe and moderate/severe hypothermia than in patients with mild hypothermia/euthermia. Considering this stable figure and the potential outcomes of this form of coagulopathy, it is critical to use timely diagnostic measures (e.g. thromboelastography) in order to guide the therapy based on rational and objective goals.
Although beyond the scope of our research, we included other types of complications such as croup, acute renal failure, adrenal insufficiency, pneumonia and bronchospasm. The incidence of these complications was similar to that reported in previous studies (Allareddy et al. – close to 10%).26 This author included complications of cardiac origin (0.7%) in that percentage; in our study, no evidence of those complications was found, and air embolism was not included in either of the two studies as a cause of neurological complications.27
As was the case in the studies by Lee and Hutson,9 in our population we found an increase in Apert and Crouzon syndromes. However, there is no clinical relation with patients with syndromal craniosynostosis, hypothermia and morbidity and mortality variation, consistent with Barnett, Vega and Debeer.17,28
Blood pressure measurements as impact variables were not included in our analysis, despite the availability of invasive arterial measurements in all patients. The decision was based on the various studies that confirm that the presence of hypotension in paediatric patients is not always related to hypovolemia or tissue oxygenation alteration, and the infrequent choice of vasopressor support in the study groups. For this reason, future studies must consider assessing the impact of permissive or deliberate hypotension during surgery in order to optimize transient haemostasis measures together with other measures to control the impact of bleeding, once they are endorsed for use in the paediatric population both ethically as well as scientifically. (Data discussed by Stricker,21 Fearon,24 and Seruya29.)
Regarding ICU and hospital length of stay, we found similar statistics to those shown by Goyal et al.11 (ICU, 2 days (1–12) vs. 3.5 days (1–14), and hospital, 5 days (1–25) vs. 6 days (range 28)). This could be explained on the basis of the existence of similar care processes for patients with craniosynostosis worldwide.
Based on the results and the contrasting hypotheses between the exposure groups, no statistically significant differences for known complications were found for this cohort. Consequently, we support the use of a closed longitudinal cohort with a more firmly established protocol before the start of data collection, in order to estimate powered variables with a higher degree of validity and no memory or misclassification biases, based on theoretically similar methods but not calibrated for research purposes.
ConclusionsIn this study, patients exposed to severe (and moderate and severe) hypothermia compared to those exposed to mild hypothermia or euthermia, there were no statistically significant differences for the morbidities included in the protocol. However, in patients exposed to severe hypothermia there was a clinical increase in the incidence of major and massive bleeding. This does not exclude the presence of clinical differences in other morbidities associated with severe hypothermia, hence our recommendation to confirm these finding using a larger population for that degree of hypothermia (severe).
Hypothermia has to be understood as a complication, it being the outcome of a logarithmic model that includes many variables pertaining to both the surgical as well as the medical realm. But it is also a predisposing factor for other situations than may modify or aggravate the vital conditions of the patient. Because of this, isolating hypothermia as a cause or effect is not only a complex matter but also pointless. Therefore, it is highly advisable to use all possible measures available to normalize central body temperature or, otherwise, allow for mild hypothermia30 in paediatric patients, until sounder evidence is forthcoming regarding the more liberal use of thermal control in the operating room.
It is of the utmost importance to take into consideration that non-concurrent recording of some parameters under a non-investigational methodology introduces bias, something which is to be expected in this observational study with a historical cohort design. Consequently, we propose the creation of a concurrent registry and verification of our hypothesis in the light of a more valid prospective observational analytical methodology in populations similar to the one included in this cohort.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingThe present study was supported with personal budget of authors.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: González-Cárdenas VH, Vanegas-Martínez MV, Rojas-Rueda ME, Burbano-Paredes CC, Pulido-Barbosa NT. Impacto de la hipotermia durante la intervencion quirurgica de craneosinostosis. Rev Colomb Anestesiol. 2016;44:235–241.