Neurogenic bladder predispose to patients with spinal cord injuria to reflex incontinence, urinary tract infections, autonomic dysreflexia and renal failure, which is one of the key causes of mortality. Neuromodulation of the anterior sacral roots is a treatment for bladder dysfunction. The anesthesiology publications about this procedure are very rarely.
ObjectivesTo describe the hemodynamic behavior and the adverse events during the intraoperative and immediate postoperative period of patients undergoing implantation of the sacral anterior roots stimulator.
MethodsRetrospective, descriptive study of series of cases of patients with chronic spinal cord trauma implanted with the anterior sacral roots stimulator.
ResultsOut of 50 patients studied, 34% had an upper chest injury, 58% had a spinal injury secondary to a fire weapon bullet, 40% had a history of autonomic dysreflexia, 98% were had arterial line monitoring, 90% of the patients were hypotensive and 86% required vasopressors; 34% experienced bradycardia and 88% required atropine management.
ConclusionsHypotension and bradycardia are the major adverse events in the management of these patients, but they exhibit adequate response to medical treatment. Studies are needed to assess the association between the level of the injury versus the presence of bradycardia and hypotension and the ideal monitoring during the procedure.
La vejiga neurogénica predispone a los pacientes con traumatismo raquimedular a incontinencia refleja, infecciones del tracto urinario, disreflexia autonómica y fallo renal, el cual es una de las principales causas de mortalidad. La neuromodulación de las raíces sacras anteriores es un tratamiento de la disfunción vesical. Es raro encontrar publicaciones en anestesiología sobre este procedimiento.
ObjetivosDescribir el comportamiento hemodinámico y los efectos adversos durante el intraoperatorio y post-operatorio inmediato en los pacientes que han recibido implantación de estimulador de raíces sacras anteriores.
MétodosEstudio descriptivo retrospectivo de pacientes con trauma- tismo raquimedular crónico que han recibido implantación de estimulador de raíces sacras anteriores.
ResultadosDe 50 pacientes estudiados, el 34% tenían lesión torácica alta, un 58% tenía lesión espinal secundaria a herida por proyectil de arma de fuego, el 40% con antecedente de disreflexia autonómica, el 98% empleo de monitoría con línea arterial, el 90% de los pacientes presentó hipotensión y el 86% requirió manejo vasopresor, el 34% presentó bradicardia y el 88% requirió manejo con atropina.
ConclusionesLa hipotensión y la bradicardia son los principales efectos adversos durante el manejo de estos pacientes pero con adecuada respuesta al tratamiento médico. Se deben realizar estudios que evalúen la asociación entre nivel de la lesión con bradicardia e hipotensión y la monitorización ideal durante este procedimiento.
The incidence of spinal cord injury (SCI) is 15–40 cases per million people around the world; in the United States the prevalence is 200,000 in the US population with an incidence of 12,000 new cases of SCI per year.1,2
Neurogenic bladder dysfunction contributes to the morbidity and mortality of these patients3 and neuromodulation of the physiological responses of different organs through the stimulation of sacral roots is an option for treating bladder disorders,4 as well as fecal incontinence, constipation5 and sexual dysfunction.6
The sacral anterior roots stimulator (SARS) is an electronic device designed for controlling the sphincters in patients with spinal cord injuries; at the Hospital Pablo Tobón Uribe (HPTU), an urologist and a neurosurgeon implant the device. Following a spinal cord injury there is a loss of voluntary control of urination, defecation and penile erections, secondary to disruption in the conduction of nerve stimulus through the various nerve pathways. Bladder and intestinal functions as well as penile erections are governed by the sacral roots that convey the sensitive nervous or motor impulses from these organs to the brain and vice versa, and the SARS consists of a series of electrodes implanted in those sacral roots (S2, S3 and S4) to enable the spinal cord injured person to voluntarily control micturition, assist in defecation and improve the erectile function in males and vaginal lubrication in women, in addition to avoiding the need to use catheters or diapers and prevent the complications associated with their use (urinary infections, urethral injuries, kidney stones, dermatitis).
Due to their pathophysiological disorders this group of patients pose a challenge to the anesthesiologist because of the risk of cardiopulmonary complications, including autonomic dysreflexia.7–9
The information about the anesthetic technique for this procedure in PubMed and SciELO is limited. This article is aimed at describing the anesthetic experience of patients with chronic SCI undergoing SARS implantation.
Materials and methodsThis is a retrospective descriptive study of chronic SCI patients undergoing SARS implantation at the Hospital Pablo Tobón Uribe (HPTU) in Medellín, Colombia, between April 2009 and June 2011.
Prior approval by the Research and Ethics Committee of the HPTU hospital, for a review of 50 clinical records was completed to obtain demographic variables and SCI-associated characteristics. The monitoring, medicines and hemodynamic events pertaining to the management of anesthesia were recorded. Adverse events were recorded in the first 24h after surgery.
The confidentiality of the clinical records was maintained and the information was uploaded in an Access database. A frequency distribution of the different variables was used and the Kolmogorov–Smirnov test was used to establish normality. The categorical variables were represented with their absolute value and percentage, while the continuous variables were represented with their mean and standard deviation measurements (normal distribution).
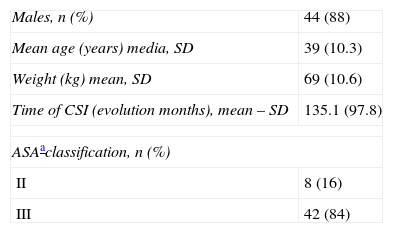
Results50 patient-records were reviewed, of which 44 (88%) were males and 6 (12%) were females. They had an ASIA (American Spinal Injury Association) A classification 42 (84%), ASIA B 1 (2%), ASIA C 2 (4%) and in 5 (10%) the information was missing. The major etiology was fire weapon bullet wound in 29 (58%), followed by 11 traffic accidents (22%). The level of the injury was T1–T6 in 17 (34%) cases, followed by cervical and low thoracic, each with 16 patients (32%) and only one patient (2%) with lumbar injury. Twenty patients (40%) had a history of autonomic dysreflexia triggered by pain, pressure sores treatment and bladder distention. The most frequent comorbidities were autonomic dysfunction, 8 (16%); hypothyroidism and neuropathic pain, each with 3 patients (6%). Table 1 illustrates the patients’ characteristics.
Patients characteristics.
| Males, n (%) | 44 (88) |
| Mean age (years) media, SD | 39 (10.3) |
| Weight (kg) mean, SD | 69 (10.6) |
| Time of CSI (evolution months), mean – SD | 135.1 (97.8) |
| ASAaclassification, n (%) | |
| II | 8 (16) |
| III | 42 (84) |
Patients underwent basic monitoring; an arterial line was placed in 49 patients (98%) of which 10 (20%) were placed with the patient awake and only one patient required a central venous catheter because of difficult venous accesses.
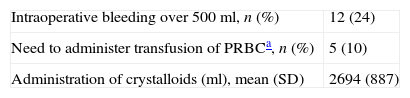
With regards to the anesthetic technique, general anesthesia was always used; 41 (82%) patients received remyfentanyl infusion, neuromuscular block induction was used in 23 (46%) patients and midazolam in 28 (56%). Orotracheal intubation was always used. The urologist placed a tree-way Foley catheter connected to the bladder pressure-recording instrument. Then, a sacral laminectomy was performed with the patient in prone decubitus. Hypotension, defined as a systolic blood pressure (SBP) less than 90mmHg was present in 45 (90%), with an average time of 17.3min (SD=25.7), that required ethylephrine 37 (74%), 1 (2%) dopamine and another patient required low-dose adrenalin bolus. No episodes of hypertension were recorded (PAS≥180mmHg and/or diastolic blood pressure≥110mmHg). Bradycardia was present in 17 (34%) of the patients with an average time of 18.4min (SD=21.6) and atropine was used in 15 (30%). 40 (80%) of the patients received analgesia with dipyrone, 10 (20%) received morphine and 9 (18%) tramadol. All patients were extubated in the operating room. Table 2 lists the intraoperative fluids. The average surgical time was 4.19h (SD=0.84) and the average duration of anesthesia was 5.35h (DE=0.795).
Intraoperative fluids.
| Intraoperative bleeding over 500ml, n (%) | 12 (24) |
| Need to administer transfusion of PRBCa, n (%) | 5 (10) |
| Administration of crystalloids (ml), mean (SD) | 2694 (887) |
During the immediate postoperative period (POP), 4 patients required vasopressors, 2 received ethylephrine and 2 received dopamine. Two patients required atropine due to bradycardia. 21 (42%) experienced pain, and of these, 14 (66.7%) was mild and only 1 case was severe; there were 9 cases of nausea 9 (18%) and 4 cases of vomiting 4 (8%). During the POP the patients were managed mostly in the general ward 43 (86%) and 7 (14%) required management in the Special Care Unit. There were no episodes of perioperative cardiorespiratory arrest, infection of the operative site, re-intervention or intraoperative por recall in the first 24h of the POP.
DiscussionJust as the stimulation of the posterior cord is used to manage chronic pain,10 SARS implants are increasingly being used for sphincteric control in spinal cord-injured patients.
The implantation of the SARS requires the anesthesiologist to provide the surgeon with the appropriate conditions to assess the motor and autonomic responses that shall determine the success of the surgical procedure.
Autonomic dysreflexia is reported in 85% of the injuries above T6,11 a figure far below the figure from our study in which 40% presented with this type of underlying injury.
While the definition of hypotension under general anesthesia in the literature is quite variable, we believe that the selected value reflects its high frequency, not only because of the physiological changes in the patient with chronic spinal cord injury – in whom the sevoflurane requirements decrease 20–39% below the level of the injury9 – but also because of the position in which the procedure is performed, the length of the surgery, blood losses and probably autonomic phenomena as a consequence of the rhizotomy.
In 98% of the study patients a radial arterial line was placed to monitor the occurrence of dysreflexia, particularly when the sacral roots are dissected and stimulated. Dysreflexia is extremely useful to make an early diagnosis.
In none of the patients was neuromuscular relaxation monitoring used which should be important in this type of surgery, since there must not be any neuromuscular block effect during sacral root stimulation.
Because of the retrospective nature of our study, one of the flaws was the lack of information. Additional studies are required to ratify or deny the association between the level of the injury with trans-operative hypotension and between the level of the injury and the presence of bradycardia, in order to standardize the anesthetic technique and appraise the addition of bi-spectral monitoring to titrate more accurately the anesthetic agents and attenuate the hemodynamic responses, in addition to monitoring of neuromuscular relaxation.
FinancingHospital Pablo Tobón Uribe and authors’ resources.
Conflict of interestThe authors have no conflicts of interest to declare.
At the PTU hospital, we express our gratitude to doctor Juan Carlos Castaño Botero, urologist and coordinator of the SARS program and to doctor Carlos Enrique Yepes Delgado, Esp. M.Sc. Ph.D. from the Research Unit.
Please cite this article as: Berrío Valencia MI, et al. Implantación de estimulador de raíces sacras anteriores: experiencia e implicaciones del manejo anestésico en el Hospital Pablo Tobón Uribe entre abril de 2009 y junio de 2011, Medellín, Colombia. Rev Colomb Anestesiol. 2013;41:16–9.