Even though foreign body aspiration (FBA) is rare in adult patients, they sometimes require the performance of rigid bronchoscopy for its extraction. Ventilation for this procedure is challenging, especially in patients with pulmonary disease.
Clinical, diagnostic evaluation and interventionsWe described the case of a 71-year old man who presented with a FBA in the left upper lobe associated with a controlateral pneumothorax. After the placement of a pleural drainage, the foreign body was extracted, using rigid bronchoscopy under general anesthesia and high flow jet ventilation with no further hemodynamic or pulmonary complications, suggesting that this technique is safe in patients with pulmonary leaks.
ConclusionIn the case described, rigid bronchoscopy minimized the risk of aspiration of blood and detritus due to continuous flow of gas upward, and avoided the increase of the air leak through the pneumothorax thank to limited airway pressures, making it a clear indication.
Aunque la aspiración de cuerpos extraños es rara en adultos, requiere en algunas ocasiones la realización de una broncoscopia rígida para su extracción. El modo ventilatorio para este procedimiento es un reto, especialmente en pacientes con enfermedad pulmonar.
Clínica, evaluación diagnóstica e intervencionesDescribimos aquí el caso de un paciente de 71 años con aspiración de un cuerpo extraño enclavado a nivel del lóbulo superior izquierdo asociado a un neumotórax contralateral. Después de insertar un tubo de tórax se extrajo el cuerpo extraño utilizando broncoscopia rígida bajo anestesia general y ventilación jet de alto flujo sin complicaciones hemodinámicas o pulmonares adicionales, sugiriendo que esta técnica es segura en pacientes con fugas pulmonares.
ConclusionesEn el presente caso clínico, la broncoscopia rígida minimizó el riesgo de aspiración de sangre y detritus gracias a la inyección de un flujo continuo de gas ascendente, y evitó así el incremento de la fuga a través del neumotórax por las presiones limitadas en la vía aérea, constituyendo una indicación clara de esta técnica.
High frequency jet ventilation (HFJV) is a recognized ventilation technique for surgical and endoscopic interventions on the bronchial tree, in particular after a foreign body aspiration (FBA). Even though few clinical cases were reported about its use in adults,1 we report the case of a patient with a FBA complicated with a pneumothorax who was ventilated with HFJV for the FBA extraction.
Patient informationWe report a case of a 71-year old male with a history of COPD and pulmonary silicosis.
Clinical findings, diagnostic assessment and interventionsHe was admitted to the emergency department of our hospital for sudden dyspnea after choking while eating, resulting in an increased work of breathing, and desaturation despite oxygen administration with reservoir mask.
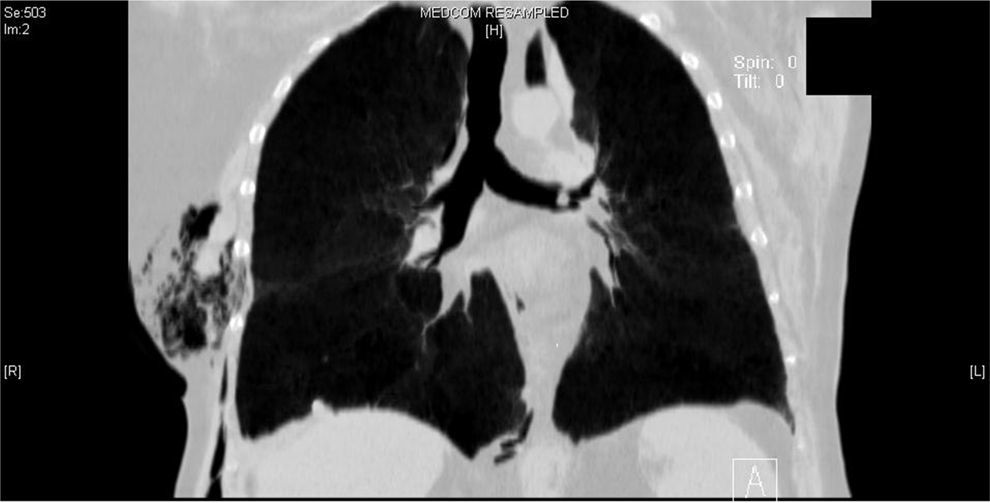
A right chest tube was placed after the diagnosis of a pneumothorax on the chest X-ray and permitted to obtain a clinical improvement. Due to the persistence of an atelectasis of the left upper lobe, a chest CT scan was performed and allowed to identify a round image of 5mm in relation with a foreign body, 3.8mm distal to the carina, which occupied the left main bronchus (Fig. 1). Given the stable clinical situation, we decided to perform a rigid bronchoscopy to extract this foreign body under general anesthesia, using HFJV (FiO2=1; pressure of 2atm; f=150cycles/min, and I-time of 50%), once the patient had accomplished the fasting time of 6h.
Follow-up and resultAfter an uneventful procedure, the patient did not present any complication, was transferred to the post anesthetic care unit, and discharged to the ward 2h after.
Discussion of the medical literatureTracheobronchial FBA is uncommon in adults, compared with children. The more common aspirated materials are dental debris, appliances, or prosthesis even though food debris are also described, especially in elderly patients and patients with neurological disorders.2
Rigid bronchoscopy is more invasive than flexible bronchoscope, but it gives more operability to the pneumologist or the thoracic surgeon and remains the gold standard when consistent mass of material is planned to be removed, since the working channels are significantly larger.3
HFJV has demonstrated its usefulness especially in neonates and pediatric patients, providing adequate gas exchange and minimizing risk of chronic respiratory diseases.
In adults, it is used for anesthesia in the upper airway surgery, ensuring the ventilation of the patient through a cannula inserted into the trachea, below the surgical field, while it improves the surgeon's comfort, suppressing the movement of the surgical field. In surgical resection of the descending thoracic aortic aneurysms, with selective lung ventilation, HFJV demonstrated its interest to ensuring the oxygenation in the non-ventilated lung. Also it has been used for lung resection, left atrial ablation by percutaneous radiofrequency, lithotripsy and laparoscopic surgery.4–6
It has been described as well for acute respiratory failure in patients with shock, applying small tidal volumes during high frequency ventilation: the lower intrathoracic pressure minimizes the interferences with venous return to the heart. In the presence of high flow bronchopleural fistula or pneumothorax, HFJV facilitates alveolar recruitment and increases the mean pressure in the airway, but decreases peak pressure and the leak. In severe respiratory failure, HFJV can maintain higher end- expiratory volumes, increasing functional residual capacity without increasing the maximum alveolar pressure. A recent publication showed that the association of HFJV with PEEP in rabbits suffering from acute lung injury improved oxygenation.7
Literature concerning the interest of HFJV in the management of patients with pneumothorax is scarce. HFJV is a known cause of pneumothorax due to barotrauma, and this is the reason why monitoring airway pressures during its use is so important. However, when there is a preexistent pneumothorax, the adequate use of HFJV probably helps to reduce the air leak through the bronchopleural fistula because a lower elevation in the airway pressure, associated with a good compromise on the oxygenation.8,9
LessonsIn the case described, rigid bronchoscopy minimized the risk of aspiration of blood and detritus due to continuous flow of gas upward, and avoided the increase of the air leak through the pneumothorax thanks to limited airway pressures, making it a clear indication and utility.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
FundingNone.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Latorre J, Brogly N, Maggi G, Quinteros F, Peña del Ser N, Gilsanz F. Ventilación jet para la extracción de un cuerpo extraño endobronquial en un paciente con neumotórax drenado: informe de caso. Rev Colomb Anestesiol. 2017;45:140–142.