Appropriate replacement of blood losses is essential to reduce morbidity and mortality in the surgical pediatric patient.
ObjectiveNon-systematic review of the literature on the management of perioperative bleeding in children.
MethodologyA systematic literature review using Pubmed, Medline, Ovid and Cochrane databases was completed on articles describing the management of perioperative bleeding in children.
ResultsReadiness is a must in situations where massive bleeding is expected. You should be knowledgeable about the indications for transfusion therapy, the prevention and management of complications of massive transfusion and the use of perioperative hemostatic agents when indicated.
Un reemplazo apropiado de las pérdidas sanguíneas es esencial para la reducción de la morbimortalidad en el paciente quirúrgico pediátrico.
ObjetivoRevisión no sistemática de la literatura sobre el manejo del sangrado perioperatorio en niños.
MetodologíaSe realizó una revisión de la literatura no sistemática, en las bases de datos de Pubmed, Medline, Ovid y Cochrane, sobre artículos que describieran el manejo del sangrado perioperatorio en niños.
ResultadosEs necesario estar preparados en las situaciones donde se espera un sangrado masivo. Se deben conocer las indicaciones de la terapia transfusional, prevenir y manejar las complicaciones de la transfusión masiva y utilizar los hemostáticos perioperatorios cuando estén indicados.
Hypovolemia is the result of blood losses and is one of the major causes of morbidity and mortality in the pediatric surgical patient; therefore, the anesthesiologists responsible for the perioperative period must be knowledgeable about the key considerations in the management of this age group.
The purpose of this paper was to make a literature review on the management of perioperative bleeding in children.
MethodologyA non-systematic literature review was completed on the management of perioperative bleeding in children, using Pubmed, Medline, Ovid and Cochrane.
ResultsThe findings of the review are listed according to the different steps of patient preparation and care.
In order to ensure adequate replacement of blood losses during the perioperative period of pediatric patients, the following steps must be considered:
1Preparation for the scheduled surgical procedure- -
In the case of surgeries with major risk of bleeding, evaluate the hemoglobin, hematocrit, clotting tests and platelets.
- -
Estimate the volemia and any allowable blood losses.
- -
Communication with the blood bank to confirm the blood reservation. Request leukoreduced, irradiated, washed blood components when indicated.1
- -
If there is risk of massive transfusion, ask for red blood cells collected less than a week ago. Hyperkalemia is one of the most feared complications in massive transfusions, particularly in children. There is a progressive increase of extracellular potassium during the storage of red blood cells; the level of potassium measured in 1unit of red blood cells after collection is 12meq/l; at 21 days it is 32meq/l and at 35 days the values are as high as 50meq/l.
Blood losses of less than 30% of the circulating blood volume: Routine monitoring.
Blood losses of 30–50% of the circulating blood volume: Routine monitoring, urinary catheter 2 peripheral blood accesses.
Blood losses of 50–100% of the circulating blood volume: Routine monitoring, urinary catheter, central venous catheter, arterial line, 2 large peripheral venous accesses.
Blood losses of over 100% of the circulating blood volume: Routine monitoring, urinary catheter, central venous line, arterial line, 2 peripheral venous accesses, rapid infusion equipment.
- -
If a massive bleeding is expected, do acid base, metabolic, and coagulation monitoring during the trans operative period.2
- -
Prevent hypothermia.
- -
A blood transfusion shall be indicated in situations where the benefits really exceed the risks.3
Transfusion thresholdA baby over 4 months old tolerated a hemoglobin decline of up to 7g/dl, as long as the baby is not hypovolemic. If the patient remains hemodynamically stable and showing signs of adequate tissue perfusion with higher hemoglobin levels, then the blood transfusion is not indicated. Children who require a higher transfusion threshold are infants under 4 months of age, children with cyanotic heart disease, chronic pneumonia and hemoglobinopathies.4–10
The red blood cell transfusion guide for children under 4 months old includes:
- -
Anemia first 24h of life: 12g/dl.
- -
Newborn babies in mechanical ventilation: 12g/dl.
- -
Children with FIO2 requirement over 35%: 12g/dl.
- -
Children with FIO2 requirement under 35%: 10g/dl.
- -
Severe chronic pneumonia, cyanotic cardiopathy, and congestive heart failure: HB 12g/dl.
- -
Blood losses over 10%.4
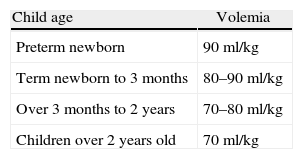
In surgeries with significant risk of bleeding, the child's volemia and the permissible blood losses (PBL) must be calculated based on his/her age (Table 1), in order to have a transfusion guide when the volume calculated has already been lost.11
The volume of blood to be transfused must be calculated for achieving the desired hematocrit. Calculating a suboptimal volume places the child at risk of a repeated blood transfusion from a different donor.
There are several methods to calculate the blood volume to be transfused. These include:
- -
VTT (volume to transfuse): 10–15ml/kg of weight.
The following formula indicated the volume of red packed cells to be transfused, in accordance with the desired hematocrit.
Volume to transfuse (VTT):
Estimated blood volume×(ideal hematocrit−actual hematocrit)/Hematocrit 1unit packed red blood cells (60–70).
Example: 1-year-old child and 12kg of weight.
Actual hematocrit: 21Ideal hematocrit: 35.
Hematocrit of 1Unit of packed red blood cells: 60–70.
- -
VTT: (12×75)×(35−21)/70
900×14/70
180ml of red blood cells to transfuse.
Platelets
Indications:
- -
Qualitative or quantitative platelet deficiency.
- -
Acute bleeding and platelets below 50,000mm3.
- -
Invasive procedures and platelets under 50,000mm3.
- -
Central nervous system procedures and platelets under 100,000mm3.
Doses:
1–2Unit/10kg or 10–15cc/kg.12–14
Fresh frozen plasma
Indications:
- -
Coagulation factors deficiency (liver disease, vitamin K deficiency, malabsortion syndrome, atresia of the extra hepatic biliary tract).
- -
Disseminated intravascular coagulation.
- -
Emergency reversal of warfarin.
- -
Dilutional coagulopathy in massive transfusion.
- -
Replacement of specific coagulation factors (factors II, V, X, XI, XIII).
- -
Hereditary angioedema.
- -
Microvascular bleeding with PT and extended TPT.
Dose:
1Unit/10kg or 10–15cc/kg.
Fresh frozen plasma is contraindicated as plasma expander en hypoalbuminemia or malnutrition and whenever specific coagulation factors are available.15,16
Cryoprecipitate:
Contains factor VIII (80Units) Von Willebrand factor, factor XIII, fibrinogen (150–250mg) and fibronectin.
Dose:
1Unit/5–10kg.
Indications:
- -
Concentration of fibrinogen less than 150mg/dl and microvascular bleeding.
- -
Massive transfusion with fibrinogen concentration under 150mg/dl and active bleeding.
- -
Deficiency of fibrinogen, dysfibrinogenemia, and afibrinogenemia.17,18
- 1.
Recognize the children at high risk for trauma-induced coagulopathy.
- 2.
Induce permissive hypotension until achieving bleeding control (except in patients with head or spinal trauma).
- 3.
Activate the massive transfusion protocol (blood bank, laboratory, surgery).
- 4.
Secure a rapid and final bleeding control (surgery, endovascular therapy).
- 5.
Constantly temperature monitoring.
- 6.
Prevent and provide early treatment for hypothermia, acidosis, hypocalcemia, hypomagnesemia, and hyperkalemia.
- 7.
Monitor coagulation at admission (thromboelastography or coagulation tests) until the coagulopathy has been corrected and the bleeding stopped.
- 8.
Frequent monitoring of lactate, arterial gases and electrolytes.
- 9.
Limit crystalloid infusion to prevent dilutional coagulopathy and thrombocytopenia.
- 10.
Transfuse the blood products in a 1:1:1 ratio in accordance with the child's bodyweight: (1unit per every 10kg of weight; for each component).
- 11.
Request red blood cells collected less than 1 week ago to reduce the risk of hyperkalemia and storage injuries.
- 12.
Use perioperative hemostatic agents as appropriate.19–21
Keep in mind the complications from blood transfusion, particularly the metabolic complications such as hypocalcemia, Hiperkalemia, hypomagnesemia, metabolic acidosis and changes in the hemoglobin dissociation curve.22,23
These complications are more frequent in children than in adults due to the relationship between the blood component administered and their volemia. For instance, 1 unit of red cells administered to an infant may represent replacing the total circulating blood volume, while 1 unit of red blood cells administered to an adult only represents replacing 10% of their volemia.24Hypocalcemia:
The citrate present in blood products chelates the calcium and produces hypocalcemia; this is more frequent with frozen fresh plasma that exhibits a higher concentration of citrate per unit of volume.
The degree of hypocalcemia depends on the blood product administered, the transfusion rate and the liver function.
Children and neonates with liver dysfunction are at high risk because of their inability to metabolize the citrate in the liver. Neonates are particularly vulnerable to hypocalcemia because their cardiac function is very much dependent on the ionized calcium levels for proper myocardial contraction and relaxation.
There may be a severe myocardial dysfunction secondary to citrate-induced hypocalcemia and this is worsened by the myocardial depressant effect of halogenated anesthetics.
Severe myocardial dysfunction may be prevented limiting the infusion rate of blood products to a maximum of 1ml/kg/min; administering a prophylactic calcium infusion and decreasing the concentration of halogenated agents.
The treatment of hypocalcemia is based on the administration of calcium chloride 5–10mg/kg or calcium gluconate 15–30mg/kg IV.
In continuous blood losses such as in the case of liver transplant, the recommendation is to administer a continuous infusion of calcium chloride 10mg/kg/h, particularly during the anhepatic phase.25Hyperkalemia:
One of the serious complications of blood transfusions is hyperkalemia that may be lethal because of arrhythmia.
The highest K levels are found in red blood cells units that are about to expire, in irradiated red blood cells and in total blood.
The recommendations include requesting red blood cells collected less than 1 week ago, using a maximum blood transfusion rate of 1ml/kg/min.
In case of arrhythmia, administer sodium bicarbonate 1meq/kg and calcium gluconate 60mg/kg or calcium chloride 20mg/kg IV.
Other measures to reduce the circulating K include the administration of dextrose insulin, hyperventilation and the use of betamimetics.25Hypomagnesemia:
This is another complication secondary to massive transfusion because the citrate chelates both calcium and magnesium. Magnesium is essential for stabilizing the membrane potential and to preserve cardiovascular stability.
If there is arrhythmia (ventricular tachycardia or ventricular fibrillation) and it is not responsive to the administration of calcium, consider hypomagnesimia and administer magnesium sulfate 25–50mg/kg IV.25Hypothermia:
Children experience a higher heat loss due to their large surface area versus their bodyweight. Furthermore, they are particularly sensitive to hypothermia and to its deleterious effects such as: hypoglycemia, apnea, decreased drug metabolism, decrease oxygen delivery to the tissues, increased oxygen consumption, worsening of coagulopathy resulting in higher morbidity and mortality. Consequently, it is absolutely indispensable to prevent hypothermia through different means.
5Pharmacological interventions to reduce perioperative bleedingAntifibrinolysis:
Tranexamic acid and epsilon-aminocaproic acid are synthetic analogs of lysine that competitively inhibit the activation of plasminogen to plasmin; the molecule responsible for fibrin degradation.
The meta-analysis published in Pediatric Critical Care concludes that antifibrinolytics reduce perioperative bleeding in major pediatric surgery and the tranexamic acid is as effective as aprontin to reduce blood losses and decrease the allogeneic transfusion in cardiac surgery and scoliosis.26
Studies on the use of tranexamic acid in craniosynostosis conclude that it is a useful therapeutic tool to reduce perioperative bleeding and lower the use of hemoderivatives in this type of patients.27,28
It has been concluded that in scoliosis surgery, antifibrinolysis such as tranexamic acid, reduce blood losses in children and consequently, this therapeutic tool may be added to other blood sparing methods.29
The recommended dose of tranexamic acid as bolus is 20mg/kg and continuous infusion of 10mg/kg/h.30
DesmopressinDesmopressin increases the factor VIII and Von Willebrand (VWF) factor plasma concentrations due to the induced release of the VWB factor from the Weibel Palade bodies in the vascular endothelium; desmopressin affects the platelet activity through its adhesion to the vascular wall; raises 3- to 5-fold the levels of the Von Willebrand factor and factor VIII following its IV administration and keeps these levels high for up to 10h.
Dose 0.3μg/kg IV.31
Exercise care in children under 2 years of age because of the high risk of hyponatremia; 66% of the fluid basal requirements must be reduced, and dextrose should be avoided; do not administer hypotonic fluids and control Na regularly.
Indications:
Congenital disorders:
Von Willebrand disease: type I, contraindicated in type 2B; ineffective in type III.
Mild a hemophilia:
Effective for minor procedures or dental extractions.
Platelet function congenital disorders:
Bernard Soulier Syndrome.
Vascular disorders:
Ehlher–Danlos, Marfan Syndrome.
Acquired disorders:
Acquired Von Willebrand syndrome:
It is rare, however may occur in children with tumor lesions such as Wilms tumor, myelo/lymphoproliferative diseases, hypothyroidism, congenital heart disease.
Acquired hemophilia A:
May present in children with autoimmune diseases or neoplasias.
Other indications include children with liver disease, uremia, and aspirin platelet dysfunction.32
It has also been used in patients with no history of coagulation disorders and massive intraoperative bleeding.33,34
Recombinant factor VIIInitially factor VII was approved for bleeding episodes in hemophilic patients who develop antibodies against factor VIII and factor IX. It was later approved for patients with platelet disorders such as Glazmann thrombasthenia.35Actually, it has been used off-label for the management of bleeding in pediatric patients.36–39
A literature review article evaluating the use of factor VII with off-label indications in children reports that the current evidence is not conclusive on the safety and efficacy of factor VII with off-label indications in pediatric patients.40
A retrospective multicenter cohort study,41 evaluates the use of factor VII with off-label indications in pediatric patients and the incidence of thrombotic events. It has been concluded that the use of factor VII in children has rapidly increased in the last few years, the mortality among patients receiving factor VII for off-label indications is higher and there is a higher incidence of thrombotic events.42
The literature shows that there are lots of questions about the safety and efficacy of factor VII in children with off-label indications. Ideally, the use of factor VII should be limited to clinical situations of refractory and incontrollable surgical or trauma bleeding where treatment options are limited.43
Fibrinogen concentrateFibrinogen concentrate may be used for certain types of perioperative or trauma bleeding in patients with no prior fibrinogen congenital deficiency or dysfunction and in patients with a reduced fibrinogen synthesis due to liver failure.
Its indications are hemorrhagic diathesis in congenital disorders such as hypofibrinogenemia, dysfibrinogenemia, and afibrinogenemia as well as in acquired hypofibrinogenemias such as synthesis disorders, increased intravascular consumption and hyperfibrinolysis. The recommended dose is 30–50mg/kg.44
Prothrombin complexThe prothrombin complex (PCC) contains factors II, VII, IX, and X, as well as anticoagulant factors such as Protein S, Protein C and heparin traces, although its primary indication is to reverse Warfarin and for the treatment of bleeding in hemophilic patients with inhibitors and deficiency of specific coagulation factors. PCC has been used in the management of perioperative bleeding refractive to the use of fresh frozen plasma, platelets and cryoprecipitate. It has the advantage of decreasing the incidence of volume overload, the most frequent complication in pediatric patients and with the lowest risk of viral transmission. The recommended dose is 20–30UI/kg calculated with factor II. There are few studies in children and there is not yet a strong recommendation for its use in pediatric patients.45,46
6Consider the usefulness and limitations of the various coagulation testsPT, TPT, and platelets are quantitative measurements done in vitro, without taking into account the complete coagulation cascade or the intervening cell elements: furthermore, these tests are done with plasma poor in platelets and at a constant temperature of 37°C, so usually they fail to reflect exactly what is going on with the patient.Thromboelastography (TEG) provides overall information about the hemostasis in each coagulation phase, in the formation of the initial clot, the retraction of the clot and the fibrinolysis. It has been particularly useful in liver transplantation, heart surgery, and trauma.47–49
7Blood conservation methodsJust as in adults, strategies have been used in children to reduce allogeneic transfusion. The most extensively used surgical procedures have been cardiac surgery, liver transplant, scoliosis, and craniosynostosis.
The strategies used are preoperative autologous transfusion, acute normovolemic hemodilution, controlled hypotension, and administration of preoperative erythropoietin, cell saver use, and blood transfusion threshold.50,51
ConclusionsEvery hospital must develop a multidisciplinary protocol to treat massive bleeding in accordance with the resources available at the institution and the needs of the community. Specialist who take care of children with severe bleeding must anticipate coagulopathy and focus on achieving hemostasis as soon as possible; early intervention is in order for the multiple aspects of hemorrhagic shock such as hypothermia, acidosis, and hemodilution.52
Sources of financingAuthor's resources.
Conflict of interestThe author states that there is no conflict of interest.
Please cite this article as: Zuluaga Giraldo M. Manejo del sangrado perioperatorio en niños. Revisión paso a paso. Rev Colomb Anestesiol. 2013;41:50–6.